Prevalence and patient awareness of inflammatory bowel disease in Kazakhstan: a cross-sectional study
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Research Institute of Cardiology and Internal Diseases, Almaty, Kazakhstan
- 2Department of Epidemiology, Biostatistics and Evidence Based Medicine, Al-Farabi Kazakh National University, Almaty, Kazakhstan
- 3Kazakhstan School of Public Health, Almaty, Kazakhstan
- 4Division of Gastroenterology, McMaster University, Hamilton, ON, Canada
- KMID: 2508573
- DOI: http://doi.org/10.5217/ir.2019.00099
Abstract
- Background/Aims
There has been a paucity of published data on the epidemiology of inflammatory bowel disease (IBD) in Central Asia and Kazakhstan. Therefore, we aimed to study IBD prevalence and patient awareness among adults in Kazakhstan.
Methods
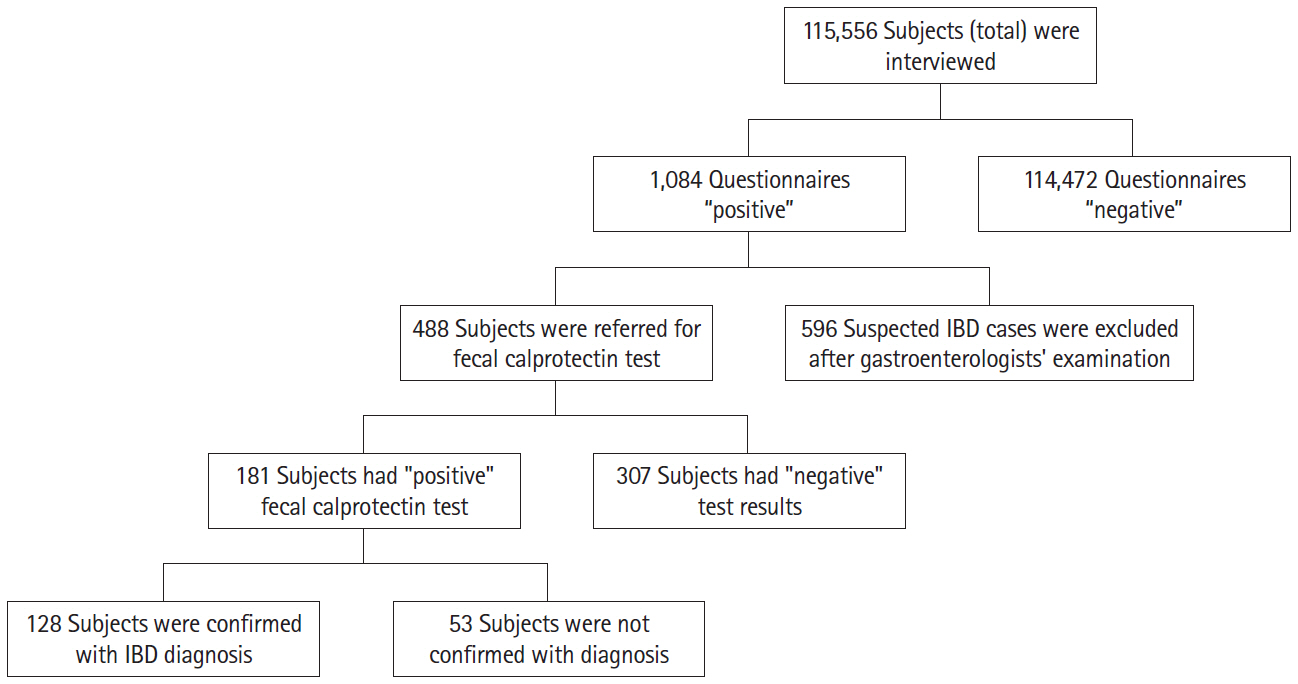
The cross-sectional study was carried out among subjects of both sexes aged 18 years and older using IBD Alert Questionnaire (CalproQuest), single fecal calprotectin test, and endoscopy with biopsy to verify IBD from January to December 2017, across regions of Kazakhstan. All participants were included in the study after providing informed consent.
Results
Out of 115,556 subjects, there were 128 confirmed IBD cases, in which 36 Crohn’s disease (CD) and 92 ulcerative colitis (UC) cases identified. The age and sex-adjusted IBD prevalence were 113.9 (95% confidence interval [CI], 69.0–158.9) per 100,000 population. The age- and sex-adjusted prevalence for UC were 84.4 (95% CI, 44.8–123.9) and for CD were 29.5 (95% CI, 8.2–50.9) per 100,000 population.
Conclusions
This is the first report on the prevalence of IBD with a verified diagnosis in the Central Asia and could be used to better plan and allocate healthcare resources for IBD management program.
Keyword
Figure
Cited by 6 articles
-
The first step to unveil the epidemiology of inflammatory bowel disease in Central Asia
Seung Wook Hong, Byong Duk Ye
Intest Res. 2020;18(4):345-346. doi: 10.5217/ir.2020.00121.Fecal S100A12 is associated with future hospitalization and step-up of medical treatment in patients with Crohn’s disease in clinical remission: a pilot study
Sun-Ho Lee, Sung Wook Hwang, Sang Hyoung Park, Dong-Hoon Yang, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang, Byong Duk Ye
Intest Res. 2022;20(2):203-212. doi: 10.5217/ir.2021.00020.Update on the epidemiology of inflammatory bowel disease in Asia: where are we now?
Sang Hyoung Park
Intest Res. 2022;20(2):159-164. doi: 10.5217/ir.2021.00115.Evaluation of nutritional status using bioelectrical impedance analysis in patients with inflammatory bowel disease
Seung Hyuk Kim, You Sun Kim, Si Hyeong Lee, Hyun Mi Lee, Won Eui Yoon, Seo Hyun Kim, Hee Jun Myung, Jeong Seop Moon
Intest Res. 2022;20(3):321-328. doi: 10.5217/ir.2021.00022.Natural history of inflammatory bowel disease: a comparison between the East and the West
Eun Mi Song, Suk-Kyun Yang
Intest Res. 2022;20(4):418-430. doi: 10.5217/ir.2021.00104.Real-world effectiveness and safety of ustekinumab induction therapy for Korean patients with Crohn’s disease: a KASID prospective multicenter study
Kyunghwan Oh, Hee Seung Hong, Nam Seok Ham, Jungbok Lee, Sang Hyoung Park, Suk-Kyun Yang, Hyuk Yoon, You Sun Kim, Chang Hwan Choi, Byong Duk Ye
Intest Res. 2023;21(1):137-147. doi: 10.5217/ir.2021.00173.
Reference
-
1. Longobardi T, Jacobs P, Bernstein CN. Work losses related to inflammatory bowel disease in the United States: results from the National Health Interview Survey. Am J Gastroenterol. 2003; 98:1064–1072.
Article2. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794.
Article3. Anderson A, Click B, Ramos-Rivers C, et al. The association between sustained poor quality of life and future opioid use in inflammatory bowel disease. Inflamm Bowel Dis. 2018; 24:1380–1388.
Article4. Graff LA, Walker JR, Lix L, et al. The relationship of inflammatory bowel disease type and activity to psychological functioning and quality of life. Clin Gastroenterol Hepatol. 2006; 4:1491–1501.
Article5. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018; 390:2769–2778.
Article6. Results of the II National Forum on the IBD. Kazakhstan Pharmaceutical Bulletin Web site. http://pharmnews.kz/ru/article/itogi-ii-nacionalnogo-foruma-po-vzk_13762. Updated June 8, 2018. Accessed April 16, 2019.7. Hasler S, Zahnd N, Müller S, et al. VAlidation of an 8-item-questionnaire predictive for a positive calprotectin tEst and Real-life implemenTation in primary care to reduce diagnostic delay in inflammatory bowel disease (ALERT): protocol for a prospective diagnostic study. BMJ Open. 2015; 5:e007306.
Article8. Chmiel C, Vavricka SR, Hasler S, et al. Feasibility of an 8-item questionnaire for early diagnosis of inflammatory bowel disease in primary care. J Eval Clin Pract. 2019; 25:155–162.
Article9. Hessels J, Douw G, Yildirim DD, Meerman G, van Herwaarden MA, van den Bergh FA. Evaluation of Prevent ID and Quantum Blue rapid tests for fecal calprotectin. Clin Chem Lab Med. 2012; 50:1079–1082.
Article10. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1: diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25.
Article11. Magro F, Gionchetti P, Eliakim R, et al. Third european evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017; 11:649–670.
Article12. Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences. 7th ed. New York: John Wiley & Sons;1999.13. Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008; 14:1660–1666.
Article14. Freeman HJ. Use of the Crohn’s disease activity index in clinical trials of biological agents. World J Gastroenterol. 2008; 14:4127–4130.
Article15. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article16. Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998; 52:119–126.
Article17. Bains N. Standardization of rates. Association of Public Health Epidemiologists in Ontario Web site. http://core.apheo.ca/resources/indicators/Standardization%20report_NamBains_FINALMarch16.pdf. Updated 2009. Accessed May 2, 2017.18. Burisch J, Pedersen N, Čuković-Čavka S, et al. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut. 2014; 63:588–597.
Article19. Belousova EA, Abdulganieva DI, Alexeeva OP, et al. Social and demographic characteristics, features of disease course and treatment options of inflammatory bowel disease in Russia: results of two multicenter studies. Almanac Clin Med. 2018; 46:445–463.
Article20. Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015; 12:720–727.
Article21. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017; 152:313–321.
Article22. Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007; 5:1424–1429.
Article23. NCD Risk Factor Collaboration (NCD-RisC). Rising rural bodymass index is the main driver of the global obesity epidemic in adults. Nature. 2019; 569:260–264.24. Soon IS, Molodecky NA, Rabi DM, Ghali WA, Barkema HW, Kaplan GG. The relationship between urban environment and the inflammatory bowel diseases: a systematic review and meta-analysis. BMC Gastroenterol. 2012; 12:51.
Article25. Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A. Epidemiology of Crohn’s disease and ulcerative colitis in a central Canadian province: a population-based study. Am J Epidemiol. 1999; 149:916–924.26. Loftus EV Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn’s disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998; 114:1161–1168.27. Molinié F, Gower-Rousseau C, Yzet T, et al. Opposite evolution in incidence of Crohn’s disease and ulcerative colitis in Northern France (1988-1999). Gut. 2004; 53:843–848.
Article28. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.
Article29. Abegunde AT, Muhammad BH, Bhatti O, Ali T. Environmental risk factors for inflammatory bowel diseases: evidence based literature review. World J Gastroenterol. 2016; 22:6296–6317.
Article30. Winther KV, Jess T, Langholz E, Munkholm P, Binder V. Survival and cause-specific mortality in ulcerative colitis: follow-up of a population-based cohort in Copenhagen County. Gastroenterology. 2003; 125:1576–1582.
Article31. Burri E, Beglinger C. Faecal calprotectin in the diagnosis of inflammatory bowel disease. Biochem Med (Zagreb). 2011; 21:245–253.
Article32. Puolanne AM, Kolho KL, Alfthan H, Ristimäki A, Mustonen H, Färkkilä M. Rapid faecal tests for detecting disease activity in colonic inflammatory bowel disease. Eur J Clin Invest. 2016; 46:825–832.
Article33. Brookes MJ, Whitehead S, Gaya DR, Hawthorne AB. Practical guidance on the use of faecal calprotectin. Frontline Gastroenterol. 2018; 9:87–91.
Article34. Laserna-Mendieta EJ, Lucendo AJ. Faecal calprotectin in inflammatory bowel diseases: a review focused on meta-analyses and routine usage limitations. Clin Chem Lab Med. 2019; 57:1295–1307.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Landscape of inflammatory bowel disease in Singapore
- Differentiation of fibrotic and inflammatory component of Crohn’s disease-associated strictures
- Irritable bowel syndrome and inflammatory bowel disease overlap syndrome: pieces of the puzzle are falling into place
- Update on the epidemiology of inflammatory bowel disease in Asia: where are we now?
- Diagnostic Tips for Making the Diagnosis of Inflammatory Bowel Disease