Intest Res.
2020 Oct;18(4):412-420. 10.5217/ir.2019.00130.
Phenotypic characteristics of pediatric inflammatory bowel disease in Japan: results from a multicenter registry
- Affiliations
-
- 1Division of Gastroenterology, National Center for Child Health and Development, Setagaya, Japan
- 2Inflammatory Bowel Disease Center, Yokohama City University Medical Center, Yokohama, Japan
- 3Department of General Pediatrics and Gastroenterology, Miyagi Children’s Hospital, Sendai, Japan
- 4Division of Gastroenterology and Hepatology, Saitama Children’s Medical Center, Saitama, Japan
- 5Department of Gastroenterology, Tokyo Metropolitan Children’s Medical Center, Fuchu, Japan
- 6Department of Pediatrics and Child Health, Kurume University School of Medicine, Kurume, Japan
- 7Department of Pediatric and Adolescent Medicine, Juntendo University Graduate School of Medicine, Bunkyo, Japan
- 8Department of Pediatrics, Shinshu University School of Medicine, Matsumoto, Japan
- 9Department of Pediatrics, Gunma University Graduate School of Medicine, Maebashi, Japan
- 10Department of Pediatrics, Osaka Medical College, Takatsuki, Japan
- 11Department of Gastrointestinal and Pediatric Surgery, Mie University Graduate School of Medicine, Tsu, Japan
- 12Department of Pediatric Surgery, Chiba University Graduate School of Medicine, Chiba, Japan
- 13Department of Pediatrics, Okinawa Prefectural Chubu Hospital, Okinawa, Japan
- 14Department of Pediatrics, Tokyo Medical University, Shinjuku, Japan
- 15Department of Pediatrics, Jichi Medical University, Shimotsuke, Japan
- 16Department of Pediatrics, Osaka General Medical Center, Osaka, Japan
- 17Division of Infectious Disease and Immunology, Aichi Children’s Health and Medical Center, Obu, Japan
- 18Department of Pediatrics, Osaka Police Hospital, Osaka, Japan
- 19Department of Pediatrics, Akita University Graduate School of Medicine, Akita, Japan
- 20Department of Gastroenterology, Yamagata Prefectural Central Hospital, Yamagata, Japan
- 21Inflammatory Bowel Disease Center, Toho University Sakura Medical Center, Sakura, Japan
- 22Department of Global Health Promotion, Tokyo Medical and Dental University, Bunkyo, Japan
- KMID: 2508568
- DOI: http://doi.org/10.5217/ir.2019.00130
Abstract
- Background/Aims
There are few published registry studies from Asia on pediatric inflammatory bowel disease (IBD). Registry network data enable comparisons among ethnic groups. This study examined the characteristics of IBD in Japanese children and compared them with those in European children.
Methods
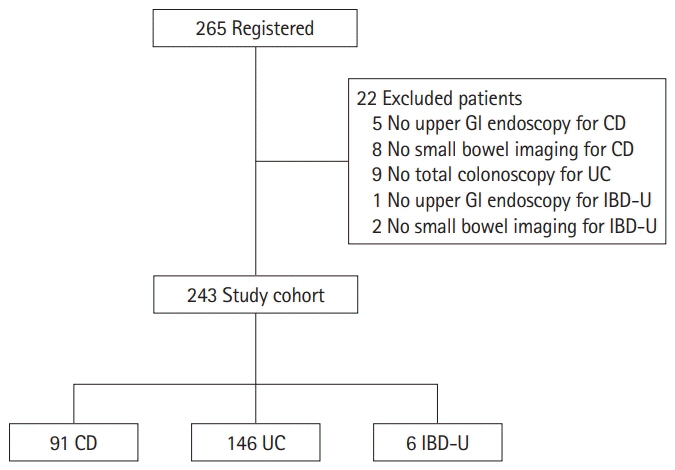
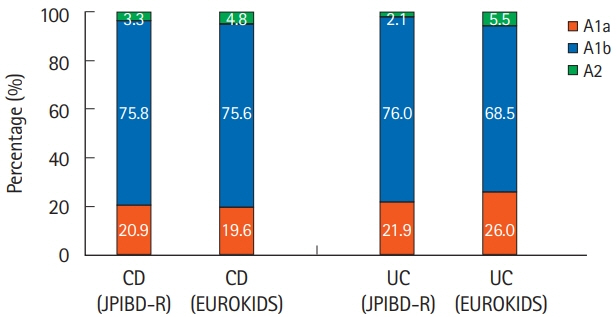
This was a cross-sectional multicenter registry study of newly diagnosed Japanese pediatric IBD patients. The Paris classification was used to categorize IBD features, and results were compared with published EUROKIDS data.
Results
A total of 265 pediatric IBD patients were initially registered, with 22 later excluded for having incomplete demographic data. For the analysis, 91 Crohn’s disease (CD), 146 ulcerative colitis (UC), and 6 IBD-unclassified cases were eligible. For age at diagnosis, 20.9% of CD, 21.9% of UC, and 83.3% of IBD-unclassified cases were diagnosed before age 10 years. For CD location, 18.7%, 13.2%, 64.8%, 47.3%, and 20.9% were classified as involving L1 (ileocecum), L2 (colon), L3 (ileocolon), L4a (esophagus/stomach/duodenum), and L4b (jejunum/proximal ileum), respectively. For UC extent, 76% were classified as E4 (pancolitis). For CD behavior, B1 (non-stricturing/non-penetrating), B2 (stricturing), B3 (penetrating), and B2B3 were seen in 83.5%, 11.0%, 3.3%, and 2.2%, respectively. A comparison between Japanese and European children showed less L2 involvement (13.2% vs. 27.3%, P< 0.01) but more L4a (47.3% vs. 29.6%, P< 0.01) and L3 (64.8% vs. 52.7%, P< 0.05) involvement in Japanese CD children. Pediatric perianal CD was more prevalent in Japanese children (34.1% vs. 9.7%, P< 0.01).
Conclusions
Upper gastrointestinal and perianal CD lesions are more common in Japanese children than in European children.
Figure
Cited by 2 articles
-
Very early onset inflammatory bowel disease in a South Asian country where inflammatory bowel disease is emerging: a distinct clinical phenotype from later onset disease
Rupa Banerjee, Partha Pal, Zaheer Nabi, Upender Shava, Girish Ganesh, D. Nageshwar Reddy
Intest Res. 2021;19(4):398-407. doi: 10.5217/ir.2020.00107.Clinical features of very early-onset inflammatory bowel disease in Japan: a retrospective single-center study
Masaaki Usami, Ichiro Takeuchi, Reiko Kyodo, Yuri Hirano, Kosuke Kashiwagi, Hiroki Fujikawa, Hirotaka Shimizu, Toshinao Kawai, Katsuhiro Arai
Intest Res. 2022;20(4):475-481. doi: 10.5217/ir.2021.00142.
Reference
-
1. Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012; 380:1590–1605.
Article2. Jelenova D, Prasko J, Ociskova M, et al. Quality of life in adolescents with inflammatory bowel disease and their parents: comparison with healthy controls. Neuro Endocrinol Lett. 2015; 36:787–792.3. Nicholas DB, Otley A, Smith C, Avolio J, Munk M, Griffiths AM. Challenges and strategies of children and adolescents with inflammatory bowel disease: a qualitative examination. Health Qual Life Outcomes. 2007; 5:28.
Article4. Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Ulcerative colitis. Lancet. 2012; 380:1606–1619.
Article5. Otley AR, Griffiths AM, Hale S, et al. Health-related quality of life in the first year after a diagnosis of pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:684–691.
Article6. Viazis N, Mantzaris G, Karmiris K, et al. Inflammatory bowel disease: Greek patients’ perspective on quality of life, information on the disease, work productivity and family support. Ann Gastroenterol. 2013; 26:52–58.7. Burisch J, Vardi H, Pedersen N, et al. Costs and resource utilization for diagnosis and treatment during the initial year in a European inflammatory bowel disease inception cohort: an ECCO-EpiCom Study. Inflamm Bowel Dis. 2015; 21:121–131.
Article8. Niewiadomski O, Studd C, Hair C, et al. Health care cost analysis in a population-based inception cohort of inflammatory bowel disease patients in the first year of diagnosis. J Crohns Colitis. 2015; 9:988–996.
Article9. Sin AT, Damman JL, Ziring DA, et al. Out-of-pocket cost burden in pediatric inflammatory bowel disease: a cross-sectional cohort analysis. Inflamm Bowel Dis. 2015; 21:1368–1377.10. Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011; 17:423–439.
Article11. Heyman MB, Kirschner BS, Gold BD, et al. Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr. 2005; 146:35–40.
Article12. Ishige T, Tomomasa T, Takebayashi T, et al. Inflammatory bowel disease in children: epidemiological analysis of the nationwide IBD registry in Japan. J Gastroenterol. 2010; 45:911–917.
Article13. Martín-de-Carpi J, Rodríguez A, Ramos E, et al. Increasing incidence of pediatric inflammatory bowel disease in Spain (1996-2009): the SPIRIT Registry. Inflamm Bowel Dis. 2013; 19:73–80.
Article14. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.
Article15. Kelsen J, Baldassano RN. Inflammatory bowel disease: the difference between children and adults. Inflamm Bowel Dis. 2008; 14(Suppl 2):S9–S11.
Article16. Buderus S, Scholz D, Behrens R, et al. Inflammatory bowel disease in pediatric patients: characteristics of newly diagnosed patients from the CEDATA-GPGE Registry. Dtsch Arztebl Int. 2015; 112:121–127.17. Castro M, Papadatou B, Baldassare M, et al. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996-2003). Inflamm Bowel Dis. 2008; 14:1246–1252.
Article18. de Bie CI, Paerregaard A, Kolacek S, et al. Disease phenotype at diagnosis in pediatric Crohn’s disease: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis. 2013; 19:378–385.19. Kugathasan S, Judd RH, Hoffmann RG, et al. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: a statewide population-based study. J Pediatr. 2003; 143:525–531.
Article20. Lee HA, Suk JY, Choi SY, et al. Characteristics of pediatric inflammatory bowel disease in Korea: comparison with EUROKIDS data. Gut Liver. 2015; 9:756–760.
Article21. Levine A, de Bie CI, Turner D, et al. Atypical disease phenotypes in pediatric ulcerative colitis: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis. 2013; 19:370–377.22. Müller KE, Lakatos PL, Kovacs JB, et al. Baseline characteristics and disease phenotype in inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2016; 62:50–55.
Article23. Urlep D, Trop TK, Blagus R, Orel R. Incidence and phenotypic characteristics of pediatric IBD in northeastern Slovenia, 2002-2010. J Pediatr Gastroenterol Nutr. 2014; 58:325–332.
Article24. White JM, O’Connor S, Winter HS, et al. Inflammatory bowel disease in African American children compared with other racial/ethnic groups in a multicenter registry. Clin Gastroenterol Hepatol. 2008; 6:1361–1369.
Article25. De Greef E, Hoffman I, Smets F, et al. Paediatric Crohn disease: disease activity and growth in the BELCRO cohort after 3 years follow-up. J Pediatr Gastroenterol Nutr. 2016; 63:253–258.26. Brückner A, Werkstetter KJ, de Laffolie J, et al. Incidence and risk factors for perianal disease in pediatric Crohn disease patients followed in CEDATA-GPGE Registry. J Pediatr Gastroenterol Nutr. 2018; 66:73–78.
Article27. Day AS, Ledder O, Leach ST, Lemberg DA. Crohn’s and colitis in children and adolescents. World J Gastroenterol. 2012; 18:5862–5869.
Article28. Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011; 17:1314–1321.
Article29. IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis: the Porto criteria. J Pediatr Gastroenterol Nutr. 2005; 41:1–7.30. Levine A, Koletzko S, Turner D, et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014; 58:795–806.
Article31. Turner D, Otley AR, Mack D, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology. 2007; 133:423–432.
Article32. Adler J, Dong S, Eder SJ, Dombkowski KJ; ImproveCareNow Pediatric IBD Learning Health System. Perianal Crohn disease in a large multicenter pediatric collaborative. J Pediatr Gastroenterol Nutr. 2017; 64:e117–e124.
Article33. Prideaux L, Kamm MA, De Cruz P, et al. Comparison of clinical characteristics and management of inflammatory bowel disease in Hong Kong versus Melbourne. J Gastroenterol Hepatol. 2012; 27:919–927.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Inflammatory Bowel Disease (IBD): Phenotypic, Genetic and Therapeutic Differences between Early-Onset and Adult-Onset IBD
- Inflammatory Bowel Disease in Pediatric Age
- Very early onset inflammatory bowel disease in a South Asian country where inflammatory bowel disease is emerging: a distinct clinical phenotype from later onset disease
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence
- Epidemiology and Registry Studies of Stroke in Japan