J Korean Med Sci.
2020 Oct;35(39):e323. 10.3346/jkms.2020.35.e323.
National Trends in the Treatment of Ruptured Cerebral Aneurysms in Korea Using an Age-adjusted Method
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 2Department of Urology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 3Department of Biostatistics, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- KMID: 2507606
- DOI: http://doi.org/10.3346/jkms.2020.35.e323
Abstract
- Background
Two primary treatment methods are used for ruptured cerebral aneurysms, surgical clipping and endovascular coiling. In recent decades, endovascular coiling has shown remarkable progress compared to surgical clipping, along with technological developments. The aim of this study was to investigate the recent trends in treatments for ruptured cerebral aneurysms in Korea.
Methods
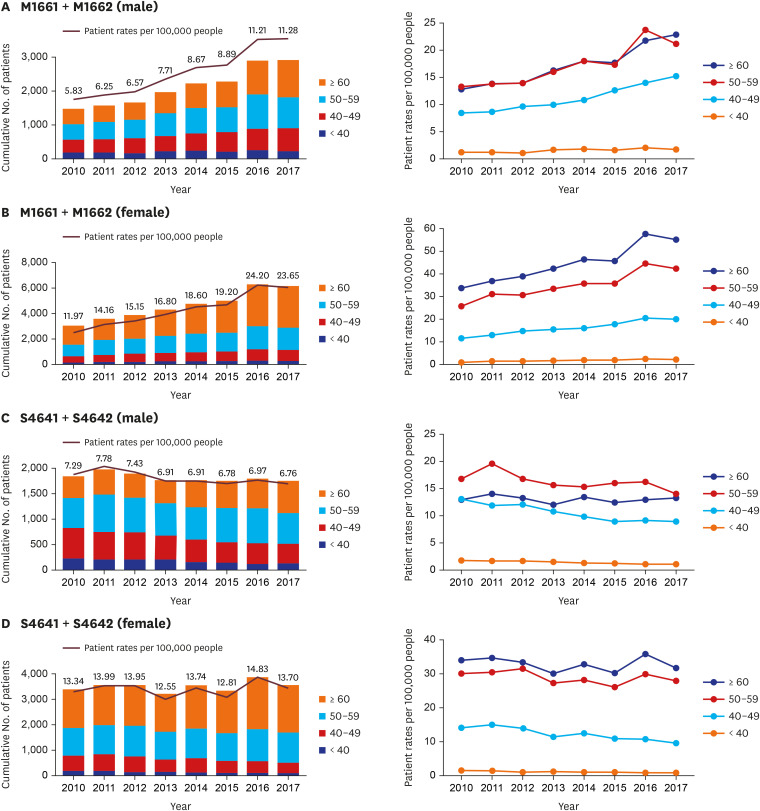
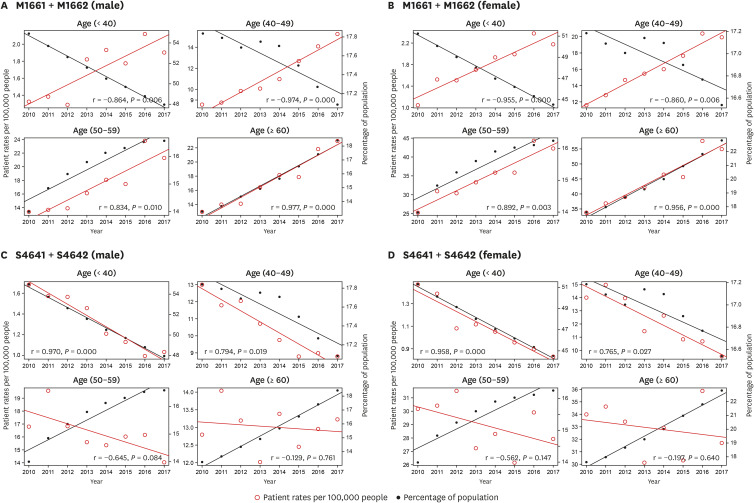
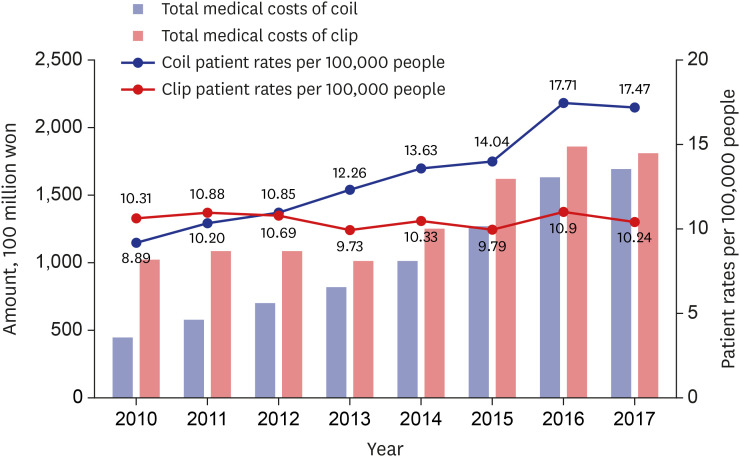
The data were obtained from the National Health Insurance database. We evaluated the trends in endovascular coiling and surgical clipping for ruptured aneurysms for the period 2000–2017. We obtained the number of prescriptions with International Classification of Diseases, 9th Revision, clinical modification codes related to nontraumatic subarachnoid hemorrhage and prescription codes S4641/4642 for surgical clipping and M1661/1662 for endovascular coiling. The medical expenses for each prescription were also obtained. The primary outcomes included the cumulative number of patients, patient rates per 100,000 people, and the correlation between patient rates and the percentage of the population in each age group.
Results
In the case of surgical clipping, there were no increasing or decreasing trends in the cumulative number of patients when the population/age group was ignored. When examining the trends in patient rates per 100,000 population at each year in male, there was no increasing or decreasing trend in the number of surgical clippings between the age groups, in spite of a decreasing tendency in the number of surgical clipping in male in their 40s and older than 60. In females, the surgical clipping rates tended to decrease only in patients older than 60 years, but there was no tendency to increase or decrease in the other ages. In contrast, the cumulative number of patients who underwent endovascular coiling for ruptured cerebral aneurysms increased year by year regardless of the population/age group. In both male and female, there was no increasing or decreasing trend only in the group aged 40 or younger and there was an increasing tendency in the rest of the age groups. In the trend of medical expenses, both the cost of surgical clipping and endovascular coiling showed increases. Specifically, the medical expense trend in endovascular coiling increased more rapidly than that for surgical clipping.
Conclusion
There was a significant increase in the proportion of patients with ruptured aneurysms undergoing endovascular coiling between 2010 and 2017, whereas the use of surgical clipping decreased. The endovascular coiling was significantly increased in all age groups and surgical clipping was decreased in all age groups, especially in patients under 50 years of age.
Figure
Reference
-
1. Molyneux A, Kerr R. International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. J Stroke Cerebrovasc Dis. 2002; 11(6):304–314. PMID: 17903891.
Article2. McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, et al. The barrow ruptured aneurysm trial. J Neurosurg. 2012; 116(1):135–144. PMID: 22054213.
Article3. Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, et al. The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. 2015; 123(3):609–617. PMID: 26115467.
Article4. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea : Part I. Intracranial aneurysm, intracerebral hemorrhage, and arteriovenous malformation. J Korean Neurosurg Soc. 2020; 63(1):56–68. PMID: 31064041.
Article5. Kim JJ, Cho KC, Jung WS, Suh SH. Endovascular treatment for intracranial aneurysms: a nationwide survey in Korea. Neurointervention. 2020; 15(1):18–24. PMID: 31955548.
Article6. Qureshi AI. Endovascular treatment of cerebrovascular diseases and intracranial neoplasms. Lancet. 2004; 363(9411):804–813. PMID: 15016492.
Article7. Qureshi AI, Janardhan V, Hanel RA, Lanzino G. Comparison of endovascular and surgical treatments for intracranial aneurysms: an evidence-based review. Lancet Neurol. 2007; 6(9):816–825. PMID: 17706565.
Article8. Derdeyn CP, Barr JD, Berenstein A, Connors JJ, Dion JE, Duckwiler GR, et al. The International Subarachnoid Aneurysm Trial (ISAT): a position statement from the Executive Committee of the American Society of Interventional and Therapeutic Neuroradiology and the American Society of Neuroradiology. AJNR Am J Neuroradiol. 2003; 24(7):1404–1408. PMID: 12917138.9. Raabe A, Schmiedek P, Seifert V, Stolke D. German society of neurosurgery section on vascular neurosurgery: position statement on the International Subarachnoid Hemorrhage Trial (ISAT). Zentralbl Neurochir. 2003; 64(3):99–103. PMID: 12975743.10. Qureshi AI, Hutson AD, Harbaugh RE, Stieg PE, Hopkins LN. North American Trial of Unruptured and Ruptured Aneurysms Planning Committee. Methods and design considerations for randomized clinical trials evaluating surgical or endovascular treatments for cerebrovascular diseases. Neurosurgery. 2004; 54(2):248–264. PMID: 14744272.11. van der Schaaf I, Algra A, Wermer M, Molyneux A, Clarke M, van Gijn J, et al. Endovascular coiling versus neurosurgical clipping for patients with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2005; (4):CD003085. PMID: 16235314.
Article12. Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013; 44(1):29–37. PMID: 23238862.13. Hwang JS, Hyun MK, Lee HJ, Choi JE, Kim JH, Lee NR, et al. Endovascular coiling versus neurosurgical clipping in patients with unruptured intracranial aneurysm: a systematic review. BMC Neurol. 2012; 12:99. PMID: 22998483.
Article14. Kim JE, Lim DJ, Hong CK, Joo SP, Yoon SM, Kim BT. Treatment of unruptured intracranial aneurysms in South Korea in 2006 : a nationwide multicenter survey from the Korean Society of Cerebrovascular Surgery. J Korean Neurosurg Soc. 2010; 47(2):112–118. PMID: 20224709.
Article15. Fargen KM, Mocco J, Neal D, Dewan MC, Reavey-Cantwell J, Woo HH, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurgery. 2013; 73(3):466–472. PMID: 23756744.
Article16. Liu KC, Ding D, Starke RM, Geraghty SR, Jensen ME. Intraprocedural retrieval of migrated coils during endovascular aneurysm treatment with the Trevo Stentriever device. J Clin Neurosci. 2014; 21(3):503–506. PMID: 24332812.
Article17. Crobeddu E, Lanzino G, Kallmes DF, Cloft HJ. Review of 2 decades of aneurysm-recurrence literature, part 1: reducing recurrence after endovascular coiling. AJNR Am J Neuroradiol. 2013; 34(2):266–270. PMID: 22422180.
Article18. Gory B, Klisch J, Bonafé A, Mounayer C, Beaujeux R, Moret J, et al. Solitaire AB stent-assisted coiling of wide-necked intracranial aneurysms: mid-term results from the SOLARE study. Neurosurgery. 2014; 75(3):215–219. PMID: 24818784.19. Alaraj A, Wallace A, Dashti R, Patel P, Aletich V. Balloons in endovascular neurosurgery: history and current applications. Neurosurgery. 2014; 74(Suppl 1):S163–S190. PMID: 24402485.20. Bekelis K, Gottlieb D, Labropoulos N, Su Y, Tjoumakaris S, Jabbour P, et al. The impact of hybrid neurosurgeons on the outcomes of endovascular coiling for unruptured cerebral aneurysms. J Neurosurg. 2017; 126(1):29–35. PMID: 26918479.
Article21. Lanzino G, Rabinstein AA. Endovascular neurosurgery in the United States: a survey of 59 vascular neurosurgeons with endovascular training. World Neurosurg. 2011; 75(5-6):580–585. PMID: 21704910.
Article22. Johnston SC. Effect of endovascular services and hospital volume on cerebral aneurysm treatment outcomes. Stroke. 2000; 31(1):111–117. PMID: 10625724.
Article23. Smith GA, Dagostino P, Maltenfort MG, Dumont AS, Ratliff JK. Geographic variation and regional trends in adoption of endovascular techniques for cerebral aneurysms. J Neurosurg. 2011; 114(6):1768–1777. PMID: 21314274.
Article24. Suh SH. The annual trends between neurointerventional and neurosurgical procedures in Korea: analysis using HIRA data from 2010 to 2016. Neurointervention. 2017; 12(2):77–82. PMID: 28955509.
Article25. Bender MT, Wendt H, Monarch T, Lin LM, Jiang B, Huang J, et al. Shifting treatment paradigms for ruptured aneurysms from open surgery to endovascular therapy over 25 years. World Neurosurg. 2017; 106:919–924. PMID: 28736346.
Article26. Gnanalingham KK, Apostolopoulos V, Barazi S, O'Neill K. The impact of the International Subarachnoid Aneurysm Trial (ISAT) on the management of aneurysmal subarachnoid haemorrhage in a neurosurgical unit in the UK. Clin Neurol Neurosurg. 2006; 108(2):117–123. PMID: 16364540.
Article27. Halkes PH, Wermer MJ, Rinkel GJ, Buskens E. Direct costs of surgical clipping and endovascular coiling of unruptured intracranial aneurysms. Cerebrovasc Dis. 2006; 22(1):40–45. PMID: 16567936.
Article28. Hoh BL, Chi YY, Dermott MA, Lipori PJ, Lewis SB. The effect of coiling versus clipping of ruptured and unruptured cerebral aneurysms on length of stay, hospital cost, hospital reimbursement, and surgeon reimbursement at the university of Florida. Neurosurgery. 2009; 64(4):614–619. PMID: 19197221.
Article29. Park KW, Park CW, Jun YI, Yoo CJ, Kim YB, Park CW. Cost analysis for the management of cerebral aneurysms: comparison between clipping and coiling. Korean J Cerebrovasc Surg. 2006; 8(4):260–266.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Frequency and Characteristics of Paraclinoid Aneurysm in Ruptured Cerebral Aneurysms
- A Study of Morphological Characteristics of Cerebral Aneurysms
- Surgical Treatment of Unruptured Cerebral Aneurysms
- Ruptured Very Small Cerebral Aneurysms and the Usefulness of Coil Embolization
- M1 Fenestration in a Patient with Multiple Cerebral Arterial Aneurysms: Case Report