Korean J Transplant.
2020 Sep;34(3):185-192. 10.4285/kjt.2020.34.3.185.
Impact of extended-criteria donor lungs according to preoperative recipient status and age in lung transplantation
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Pulmonology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 4Division of Infectious disease, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2507163
- DOI: http://doi.org/10.4285/kjt.2020.34.3.185
Abstract
- Background
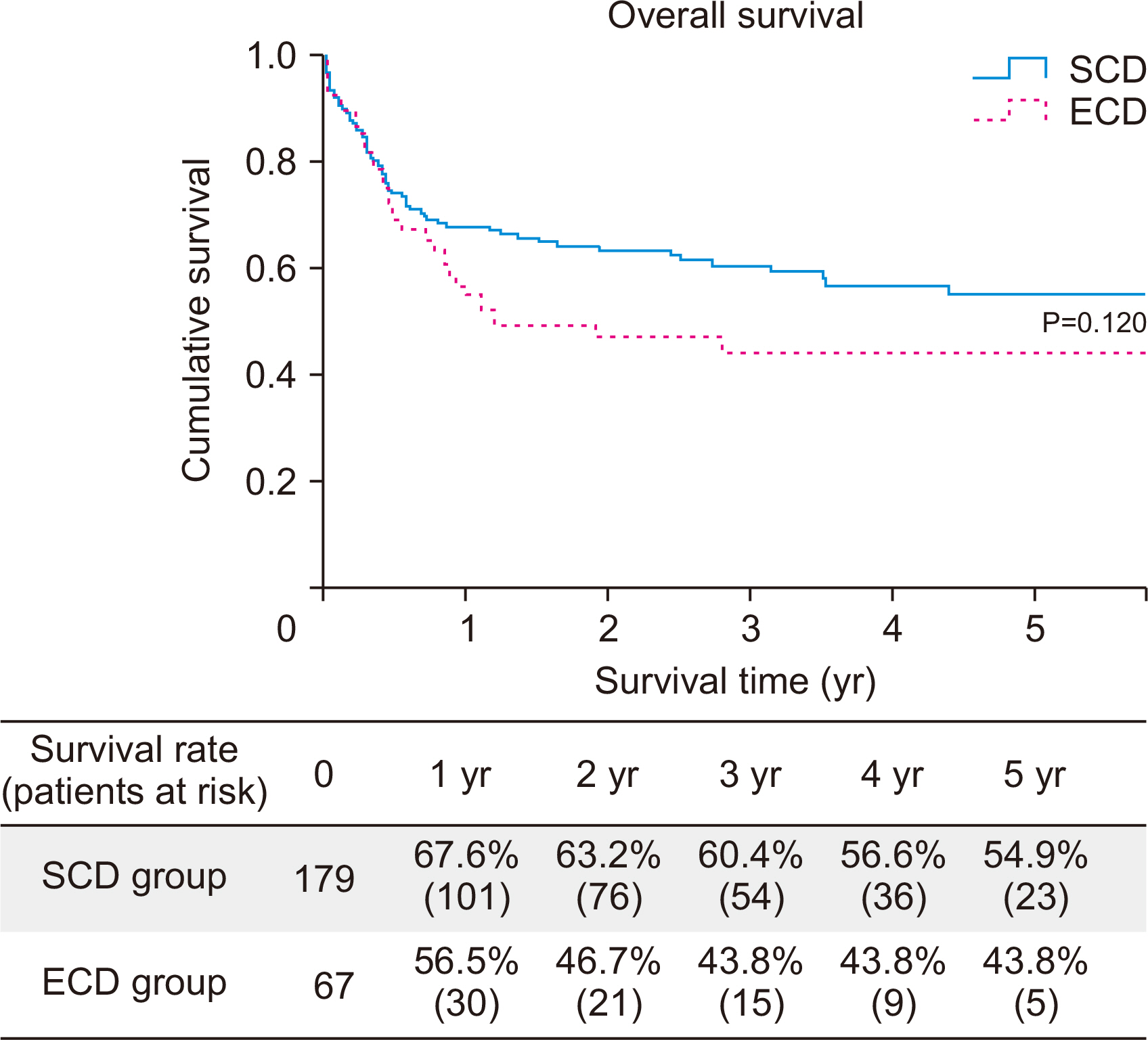
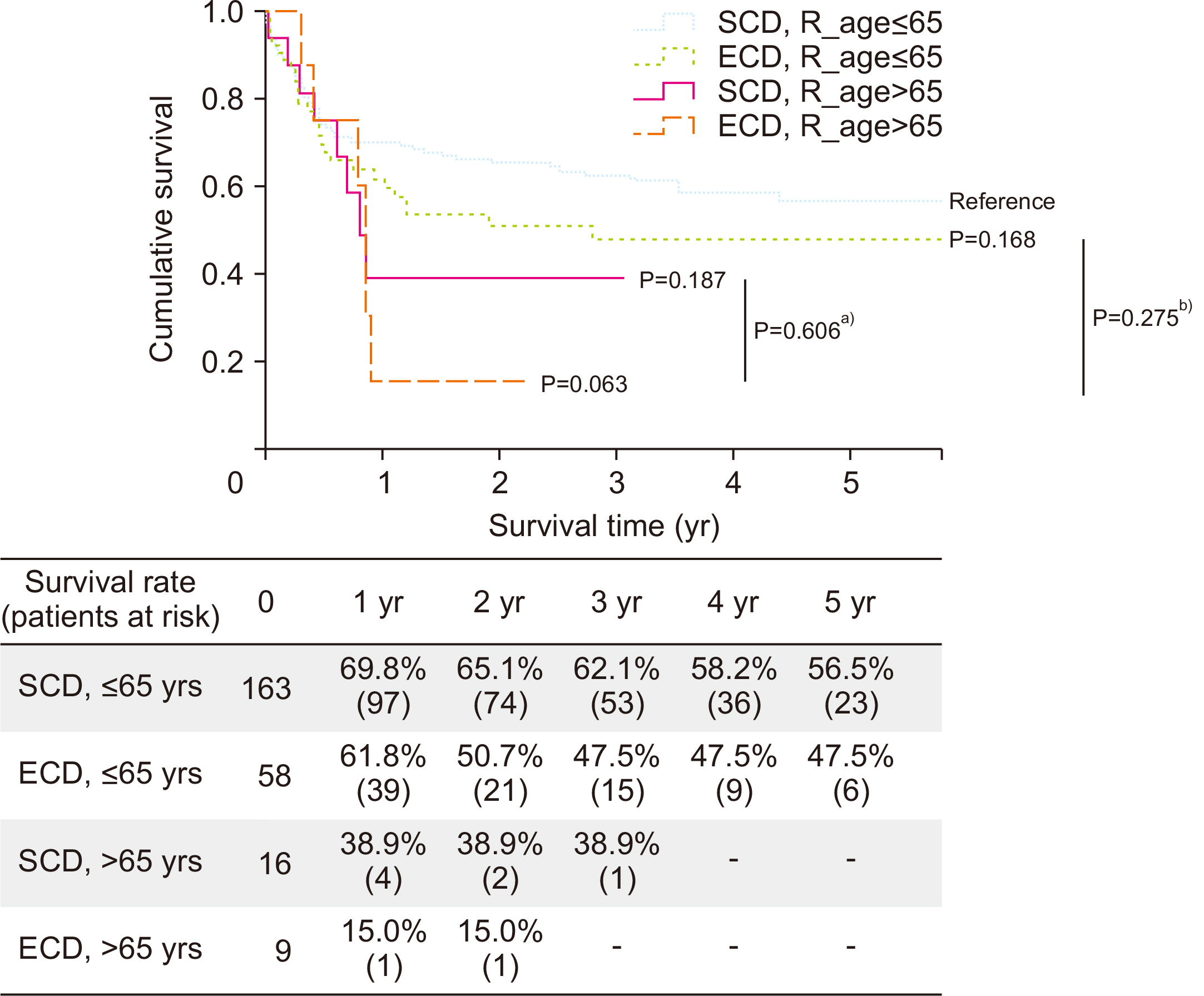
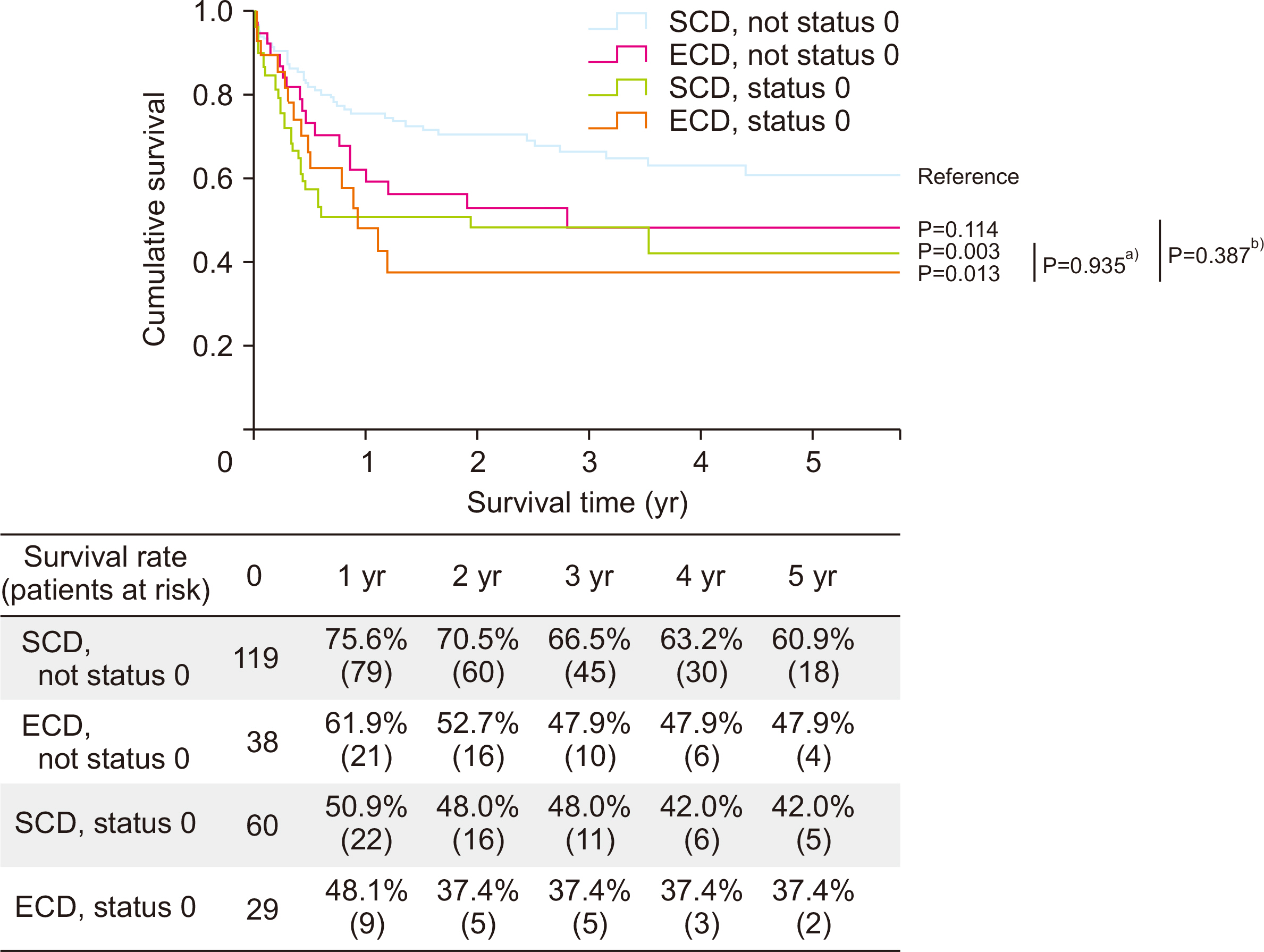
Organ donor shortage remains as one of the limiting factors for lung transplantation. Given the increase in waiting time, preoperative condition has worsened and affects surgical outcomes. This study aimed to evaluate the immediate postoperative and long-term outcomes of lung transplantation in extended-criteria donor (ECD) lungs compared with standard-criteria donor (SCD) lungs.
Methods
A total of 246 patients who had undergone double-lung transplantation during the study period were enrolled. SCD was defined based on the following characteristics: age <55 years, <20 pack-years smoking history, and PaO 2 /fraction of O 2 ratio >300 mmHg. Organ donors who do not fulfill these criteria were classified as ECD. Pre- and postoperative data for outcomes and survival data were analyzed.
Results
ECD showed significant association with extracorporeal membrane oxygenation weaning in the operating room (hazard ratio [HR], 0.531; 95% confidence interval [CI], 0.291–0.970; P=0.039) considering recipient’s age and status at operation. The ECD group showed comparable survival rate with the SCD group (HR, 1.413; 95% CI, 0.885– 2.255; P=0.148), with adjustment of other factors. However, when the recipient had Korean Network for Organ Sharing (KONOS) status 0 at the time of transplantation (HR, 1.662; 95% CI, 1.025–2.568; P=0.039), G3 primary graft dysfunction at 72 hours after surgery (HR, 2.508; 95% CI, 1.416–4.440; P=0.002) was a risk factor that decreased survival.
Conclusions
The outcome of ECD is not inferior to that of SCD. Therefore, ECD lung should be considered a potential donor organ following active donor management rather than a contraindication of transplantation in highly selected recipients.
Keyword
Figure
Reference
-
1. Korean Network for Organ Sharing (KONOS). 2018. 2018 Annual data report, in Korean Network for Organ Sharing [Internet]. KONOS;Seoul: Available from: https://www.konos.go.kr/konosis/common/bizlogic.jsp.cited 2020 Aug 20.2. Neizer H, Singh GB, Gupta S, Singh SK. 2020; Addressing donor-organ shortages using extended criteria in lung transplantation. Ann Cardiothorac Surg. 9:49–50. DOI: 10.21037/acs.2019.10.01. PMID: 32175239. PMCID: PMC7049552.
Article3. Reyes KG, Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, et al. 2010; Guidelines for donor lung selection: time for revision? Ann Thorac Surg. 89:1756–64. DOI: 10.1016/j.athoracsur.2010.02.056. PMID: 20494023.
Article4. Zych B, García Sáez D, Sabashnikov A, De Robertis F, Amrani M, Bahrami T, et al. 2014; Lung transplantation from donors outside standard acceptability criteria: are they really marginal? Transpl Int. 27:1183–91. DOI: 10.1111/tri.12410. PMID: 25070600.5. Sommer W, Kühn C, Tudorache I, Avsar M, Gottlieb J, Boethig D, et al. 2013; Extended criteria donor lungs and clinical outcome: results of an alternative allocation algorithm. J Heart Lung Transplant. 32:1065–72. DOI: 10.1016/j.healun.2013.06.021. PMID: 23953918.
Article6. Moreno P, Alvarez A, Santos F, Vaquero JM, Baamonde C, Redel J, et al. 2014; Extended recipients but not extended donors are associated with poor outcomes following lung transplantation. Eur J Cardiothorac Surg. 45:1040–7. DOI: 10.1093/ejcts/ezt501. PMID: 24163362.
Article7. Sommer W, Ius F, Salman J, Avsar M, Tudorache I, Kühn C, et al. 2015; Survival and spirometry outcomes after lung transplantation from donors aged 70 years and older. J Heart Lung Transplant. 34:1325–33. DOI: 10.1016/j.healun.2015.06.002. PMID: 26186805.
Article8. Suh JW, Lee JG, Jeong SJ, Park MS, Kim SY, Paik HC. 2020; Risk of bronchial dehiscence in lung transplant recipients with carbapenemase-producing klebsiella. Ann Thorac Surg. 110:265–71. DOI: 10.1016/j.athoracsur.2020.01.076. PMID: 32151582.
Article9. Yeo HJ, Yoon SH, Lee SE, Jeon D, Kim YS, Cho WH, et al. 2017; Current status and future of lung donation in Korea. J Korean Med Sci. 32:1953–8. DOI: 10.3346/jkms.2017.32.12.1953. PMID: 29115076. PMCID: PMC5680493.
Article10. Dahlman S, Jeppsson A, Scherstén H, Nilsson F. 2006; Expanding the donor pool: lung transplantation with donors 55 years and older. Transplant Proc. 38:2691–3. DOI: 10.1016/j.transproceed.2006.07.037. PMID: 17098041.
Article11. Bittle GJ, Sanchez PG, Kon ZN, Claire Watkins A, Rajagopal K, Pierson RN 3rd, et al. 2013; The use of lung donors older than 55 years: a review of the United Network of Organ Sharing database. J Heart Lung Transplant. 32:760–8. DOI: 10.1016/j.healun.2013.04.012. PMID: 23664760.
Article12. Schultz HH, Møller CH, Zemtsovski M, Ravn J, Perch M, Martinussen T, et al. 2017; Donor smoking and older age increases morbidity and mortality after lung transplantation. Transplant Proc. 49:2161–8. DOI: 10.1016/j.transproceed.2017.09.021. PMID: 29149977.
Article13. Hayes D Jr, Black SM, Tobias JD, Higgins RS, Whitson BA. 2015; Influence of donor and recipient age in lung transplantation. J Heart Lung Transplant. 34:43–9. DOI: 10.1016/j.healun.2014.08.017. PMID: 25301358. PMCID: PMC7489336.
Article14. Pierre AF, Sekine Y, Hutcheon MA, Waddell TK, Keshavjee SH. 2002; Marginal donor lungs: a reassessment. J Thorac Cardiovasc Surg. 123:421–7. DOI: 10.1067/mtc.2002.120345. PMID: 11882811.
Article15. Mulligan MJ, Sanchez PG, Evans CF, Wang Y, Kon ZN, Rajagopal K, et al. 2016; The use of extended criteria donors decreases one-year survival in high-risk lung recipients: a review of the United Network of Organ Sharing Database. J Thorac Cardiovasc Surg. 152:891–8. DOI: 10.1016/j.jtcvs.2016.03.096. PMID: 27234027.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Donor Selection, Management, and Procurement for Lung Transplantation
- Ex vivo lung perfusion and the Organ Care System: a review
- Ex Vivo Lung Perfusion in Lung Transplantation
- Impact of extended living donor criteria on donor safety in living donor liver transplantation
- Patient management for thoracic organ donor candidates: the lung transplantation team’s view