J Cerebrovasc Endovasc Neurosurg.
2020 Sep;22(3):134-140. 10.7461/jcen.2020.22.3.134.
Dual antiplatelet treatment associated with reduced risk of symptomatic vasospasm and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Institute of Wonkwang Medical Science, School of Medicine, Wonkwang University, Iksan, Korea
- KMID: 2506760
- DOI: http://doi.org/10.7461/jcen.2020.22.3.134
Abstract
Objective
Cerebral vasospasm and delayed cerebral ischemia (DCI) are considered complications after aneurysmal subarachnoid hemorrhage (aSAH). Several hypotheses involving platelet activation have been asserted in the pathophysiology of cerebral vasospasm and DCI. This study aimed to investigate the effect of dual antiplatelet treatment (DAPT) on symptomatic vasospasm and DCI in patients with aSAH.
Methods
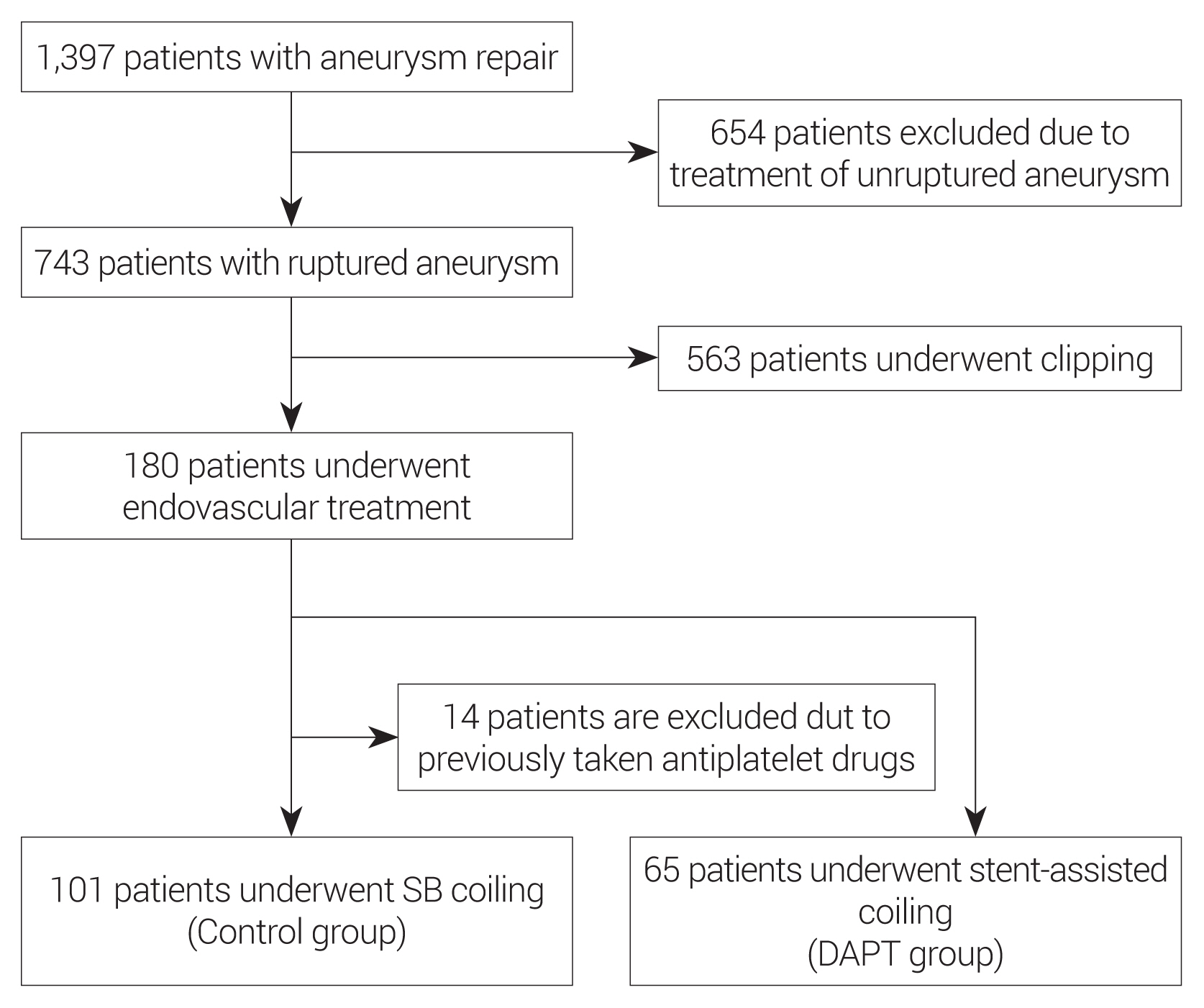
A retrospective study was conducted on patients with aSAH from 2009 to 2018. The patients are divided into 2 groups according to the treatment method such as simple or balloon-assisted coil embolization group (SB coiling), and stent-assisted coil embolization group. Patients treated by SB coiling without DAPT were classified as the control group. Patients who required dual antiplatelet treatment due to stent-assisted coil embolization were classified as DAPT group. The incidence of symptomatic vasospasm and DCI was compared between the two groups.
Results
Of 743 patients with aSAH, 563 patients were treated with clipping, 115 patients treated with SB coiling, and 65 patients receive stent-assisted coiling. Among 115 patients underwent SB coiling, 14 patients were excluded by the exclusion criteria. Total number of control group (SB coiling) was 101, DAPT group (stent-assisted coiling) was 65. Depending on whether or not taking DAPT, the incidence of symptomatic vasospasm was lower in the DAPT group (p=0.010). DCI incidence was also lower in the DAPT group, which was statistically significant (p=0.029).
Conclusions
DAPT reduces the frequency of symptomatic vasospasm and DCI in patients with aSAH in our single-center study. To warranting this topic, further, larger prospective and randomized studies should be needed.
Figure
Reference
-
1. Cagnazzo F, Derraz I, Lefevre PH, Gascou G, Dargazanli C, Riquelme C, et al. Antiplatelet therapy in patients with aneurysmal SAH: impact on delayed cerebral ischemia and clinical outcome. A meta-analysis. AJNR Am J Neuroradiol. 2019; Jul. 40(7):1201–6.
Article2. Castanares-Zapatero D, Hantson P. Pharmacological treatment of delayed cerebral ischemia and vasospasm in subarachnoid hemorrhage. Ann Intensive Care. 2011; May. 1(1):12.
Article3. Darkwah Oppong M, Gembruch O, Pierscianek D, Köhrmann M, Kleinschnitz C, Deuschl C, et al. Post-treatment antiplatelet therapy reduces risk for delayed cerebral ischemia due to aneurysmal subarachnoid hemorrhage. Neurosurgery. 2019; Dec. 85(6):827–33.
Article4. Dumont AS, Dumont RJ, Chow MM, Lin CL, Calisaneller T, Ley KF, et al. Cerebral vasospasm after subarachnoid hemorrhage: putative role of inflammation. Neurosurgery. 2003; Jul. 53(1):123–33. discussion 133–5.
Article5. Findlay JM, Nisar J, Darsaut T. Cerebral vasospasm: a review. Can J Neurol Sci. 2016; Jan. 43(1):15–32.
Article6. Helmy A, De Simoni MG, Guilfoyle MR, Carpenter KL, Hutchinson PJ. Cytokines and innate inflammation in the pathogenesis of human traumatic brain injury. Prog Neurobiol. 2011; Nov. 95(3):352–72.
Article7. Le Roux AA, Wallace MC. Outcome and cost of aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010; Apr. 21(2):235–46.
Article8. Lucke-Wold BP, Logsdon AF, Manoranjan B, Turner RC, McConnell E, Vates GE, et al. Aneurysmal subarachnoid hemorrhage and neuroinflammation: a comprehensive review. Int J Mol Sci. 2016; Apr. 17(4):497.
Article9. Mees SD, Rinkel GJ, Feigin VL, Algra A, van den Bergh WM, Vermeulen M, et al. Calcium antagonists for aneurysmal subarachnoid haemorrhage. Cochrane database of systematic reviews. Cochrane Database Syst Rev. 2007; Jul. 2007(3):CD000277.10. Ohta H, Ito Z. Cerebral infarction due to vasospasm, revealed by computed tomography. Neurol Med Chir (Tokyo). 1981; Apr. 21(4):365–72.
Article11. Rowland MJ, Hadjipavlou G, Kelly M, Westbrook J, Pattinson KT. Delayed cerebral ischaemia after subarachnoid haemorrhage: looking beyond vasospasm. Br J Anaesth. 2012; Sep. 109(3):315–29.
Article12. Senbokuya N, Kinouchi H, Kanemaru K, Ohashi Y, Fukamachi A, Yagi S, et al. Effects of cilostazol on cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a multicenter prospective, randomized, open-label blinded end point trial. J Neurosurg. 2013; Jan. 118(1):121–30.
Article13. Spallone A, Acqui M, Pastore FS, Guidetti B. Relationship between leukocytosis and ischemic complications following aneurysmal subarachnoid hemorrhage. Surg Neurol. 1987; Mar. 27(3):253–8.
Article14. Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006; Jan. 354(4):387–96.
Article15. Vergouwen MD, Vermeulen M, Coert BA, Stroes ES, Roos YB. Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab. 2008; Nov. 28(11):1761–70.
Article16. Wartenberg KE. Update on the management of subarachnoid hemorrhage. Future Neurol. 2013; Feb. 8(2):205–24.
Article17. Wu CT, Wong CS, Yeh CC, Borel CO. Treatment of cerebral vasospasm after subarachnoid hemorrhage--a review. Acta Anaesthesiol Taiwan. 2004; Dec. 42(4):215–22.18. Yoshimoto T, Shirasaka T, Fujimoto S, Yoshidumi T, Yamauchi T, Tokuda K, et al. Cilostazol may prevent cerebral vasospasm following subarachnoid hemorrhage. Neurol Med Chir (Tokyo). 2009; Jun. 49(6):235–40. discussion 240–1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relation between Thromboembolism and Delayed Ischemic Neurological Deficits in Aneurysmal Subarachnoid Hemorrhage
- Effects of Antiplatelet Agents on Cerebral Vasospasm and Delayed Cerebral Ischemia in Aneurysmal Subarachnoid Hemorrhage Patients Treated with Coil Embolization
- Thromboembolism: Another substantial cause of delayed ischemic neurologic deficits after aneurysmal subarachnoid hemorrhage
- Evaluation of Subarachnoid Hemorrhage due to Aneurysmal Rupture and Cerebral Vasospasm by CT
- Protocol Based Real-Time Continuous Electroencephalography for Detecting Vasospasm in Subarachnoid Hemorrhage