Arch Hand Microsurg.
2020 Sep;25(3):175-180. 10.12790/ahm.20.0023.
Usefulness of Ultrasonography in Diagnosis and Management of Tendon Injuries in Hand
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Bundang Jesaeng Hospital, Seongnam, Korea
- 2Department of Radiology, Bundang Jesaeng Hospital, Seongnam, Korea
- 3Department of Plastic and Reconstructive Surgery, Cheju Halla General Hospital, Jeju, Korea
- KMID: 2505898
- DOI: http://doi.org/10.12790/ahm.20.0023
Abstract
- Purpose
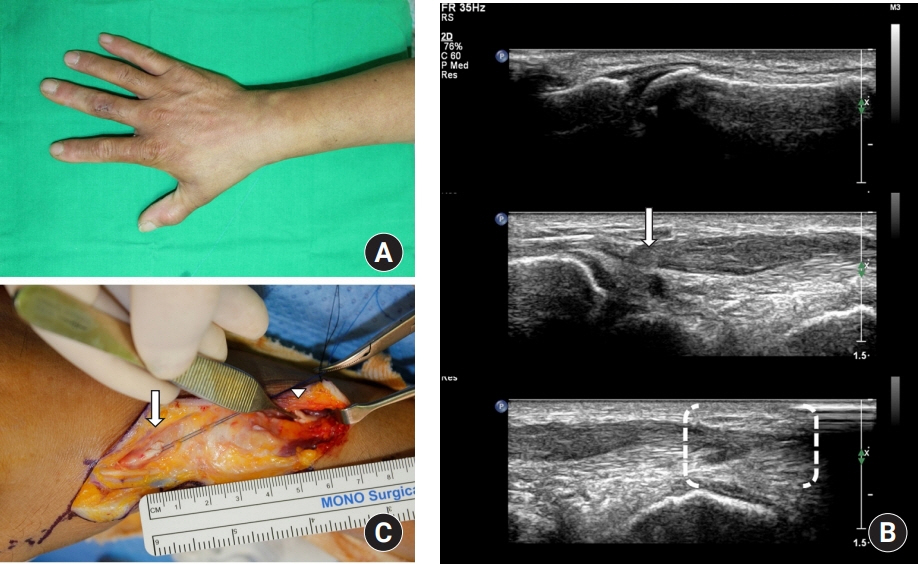
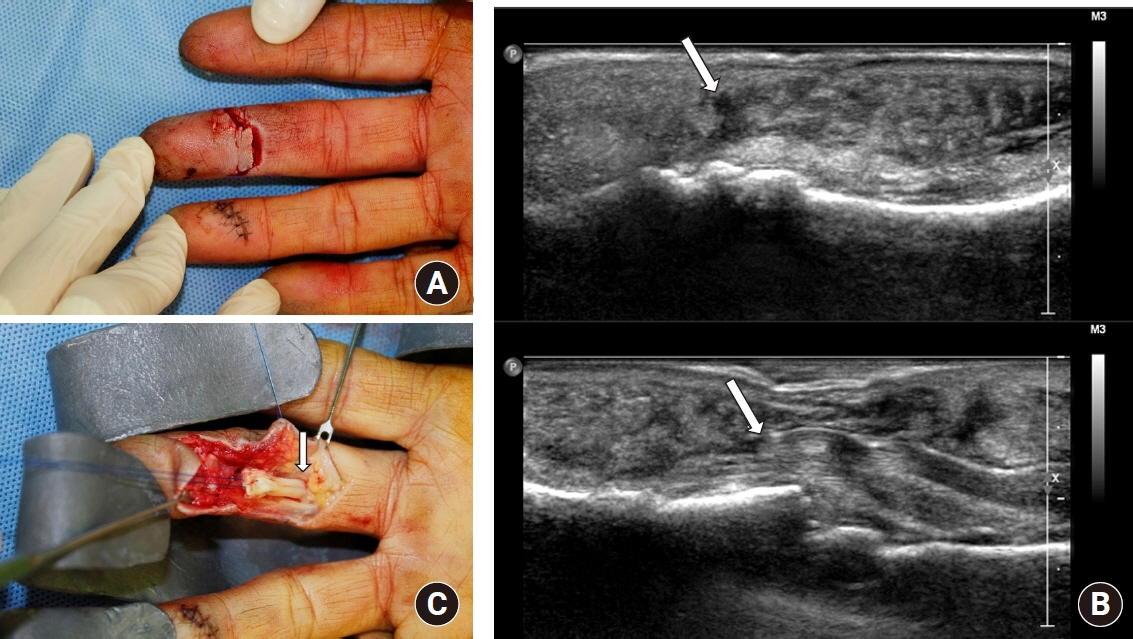
Tendon injuries in hand were one of the most frequent injuries caused by trauma. Although consequent tenorrhaphy is frequently conducted, in complete tendon rupture the location of retracted tendon stumps cannot be identified clearly, which causes difficulties in surgical management. Ultrasonography is known to be a fast, accurate, and cost-effective diagnostic method for tendon injury; therefore, the authors studied the usefulness of preoperative ultrasonography in diagnosis and management of tendon injuries in hand.
Methods
Among the 34 patients who had hand tendon injuries and visited between January 2017 and March 2018, retrospective studies were conducted on six patients with unidentified tendon stumps. By identifying the location of the tendon injuries and ruptured tendon stumps through preoperative ultrasonography, the operation was conducted under a predetermined surgical plan. The authors compared the ultrasonography results and the surgical findings.
Results
For diagnosis of the unidentified tendon injuries and location of ruptured tendon stumps, the ultrasonography results and the surgical findings were matched for all six patients. By prior planning of the operation incision line using the preoperative ultrasonography results, the length of the incision site was minimized without additional incision, and the operation time was shortened.
Conclusion
For hand tendon injuries with unidentified tendon stumps, identifying the location of tendon stumps through preoperative ultrasonography is helpful for determining the incision range for the operation. Therefore, preoperative ultrasonography may be useful in the diagnosis and management of tendon injuries in hand.
Figure
Reference
-
1. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008; 39:1338–44.
Article2. Mohammadrezaei N, Seyedhosseini J, Vahidi E. Validity of ultrasound in diagnosis of tendon injuries in penetrating extremity trauma. Am J Emerg Med. 2017; 35:945–8.
Article3. Sandvall BK, Kuhlman-Wood K, Recor C, Friedrich JB. Flexor tendon repair, rehabilitation, and reconstruction. Plast Reconstr Surg. 2013; 132:1493–503.
Article4. Soni P, Stern CA, Foreman KB, Rockwell WB. Advances in extensor tendon diagnosis and therapy. Plast Reconstr Surg. 2009; 123:52e–7e.
Article5. Nugent N, Coyle J, Barry J, O’Shaughnessy M. The use of ultrasound in evaluating flexor tendons following surgical repair. Plast Reconstr Surg. 2012; 129:392e–4e.
Article6. Wu TS, Roque PJ, Green J, et al. Bedside ultrasound evaluation of tendon injuries. Am J Emerg Med. 2012; 30:1617–21.
Article7. Scott CF Jr. Length of operation and morbidity: is there a relationships? Plast Reconstr Surg. 1982; 69:1017–21.8. Read JW, Conolly WB, Lanzetta M, Spielman S, Snodgrass D, Korber JS. Diagnostic ultrasound of the hand and wrist. J Hand Surg Am. 1996; 21:1004–10.
Article9. Lee JC, Healy JC. Normal sonographic anatomy of the wrist and hand. Radiographics. 2005; 25:1577–90.
Article10. Moschilla G, Breidahl W. Sonography of the finger. AJR Am J Roentgenol. 2002; 178:1451–7.
Article11. Robinson P. Sonography of common tendon injuries. AJR Am J Roentgenol. 2009; 193:607–18.
Article12. Daenen B, Houben G, Bauduin E, Debry R, Magotteaux P. Sonography in wrist tendon pathology. J Clin Ultrasound. 2004; 32:462–9.
Article13. Lee SA, Kim BH, Kim SJ, Kim JN, Park SY, Choi K. Current status of ultrasonography of the finger. Ultrasonography. 2016; 35:110–23.
Article14. Sharpe RE, Nazarian LN, Parker L, Rao VM, Levin DC. Dramatically increased musculoskeletal ultrasound utilization from 2000 to 2009, especially by podiatrists in private offices. J Am Coll Radiol. 2012; 9:141–6.
Article15. Ravnic DJ, Galiano RD, Bodavula V, Friedman DW, Flores RL. Diagnosis and localisation of flexor tendon injuries by surgeon-performed ultrasound: a cadaveric study. J Plast Reconstr Aesthet Surg. 2011; 64:234–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Ultrasound Diagnosis of Acute Tendon Injury in Hand
- The Utility of Ultrasonography in the Emergency Department for the Diagnosis of Finger Tendon Injury
- Tendon reconstruction of the hand in Patients with Old Flexor Tendon Injuries
- Two-Stage Tendon Reconstruction Using Hunter Silicone Rod Prosthesis
- Rupture of the extensor digitorum communis tendon in extensor zone V due to plant thorn injuries: a report of two cases