Healthc Inform Res.
2020 Jul;26(3):185-192. 10.4258/hir.2020.26.3.185.
User Acceptance of Electronic Medical Record System: Implementation at Marie Stopes International, Myanmar
- Affiliations
-
- 1Department of Tropical Hygiene (Biomedical and Health Informatics), Faculty of Tropical Medicine, Mahidol University, Thailand
- 2Center of Excellence for Biomedical and Public Health Informatics (BIOPHICS), Faculty of Tropical Medicine, Mahidol University, Thailand
- 3Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Thailand
- 4Health Systems Research Institute, Ministry of Public Health, Nonthaburi, Thailand
- 5Marie Stopes International Myanmar (MSI-M), Yangon, Myanmar
- 6Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
- KMID: 2505259
- DOI: http://doi.org/10.4258/hir.2020.26.3.185
Abstract
Objectives
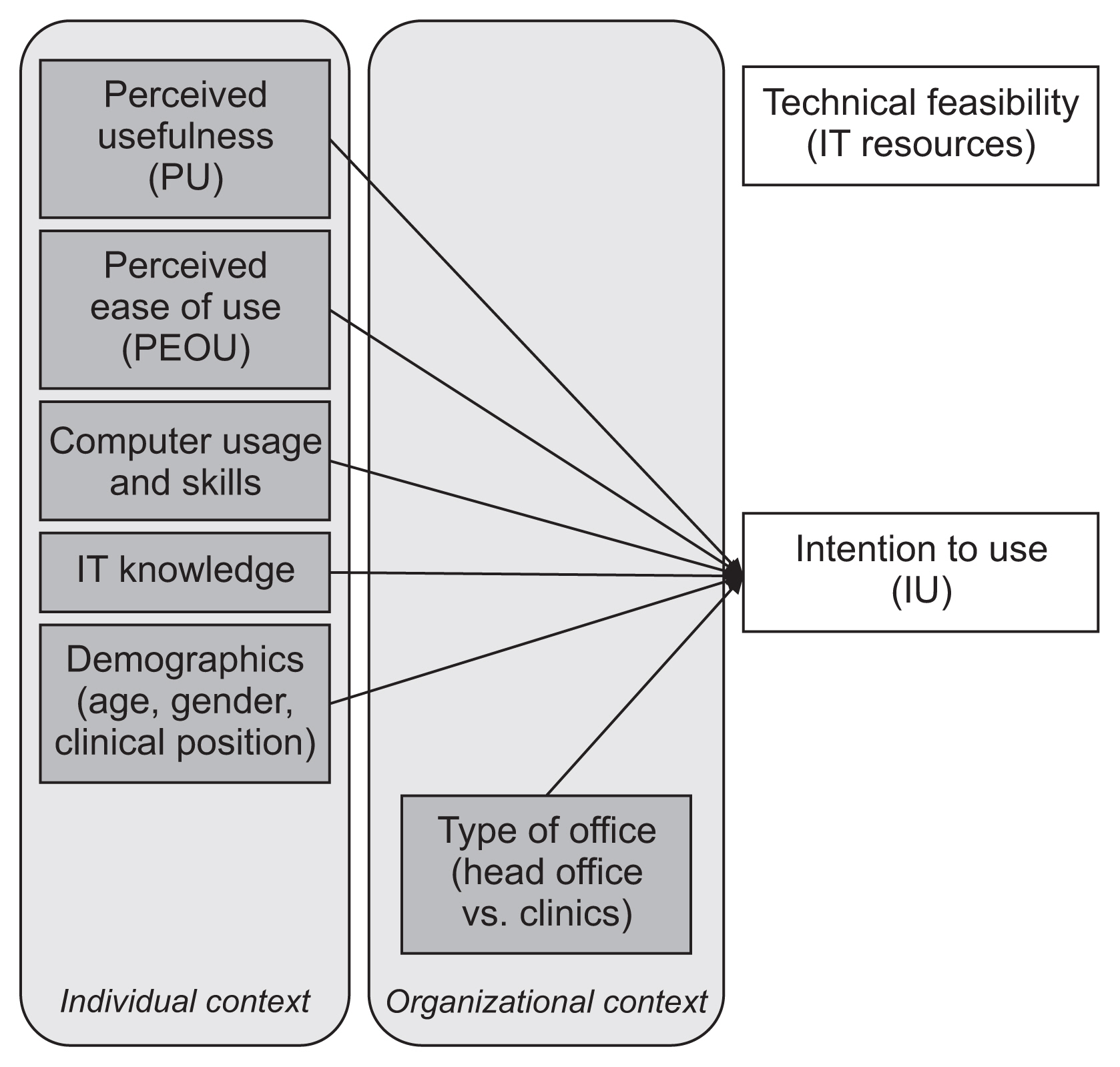
This study assessed the technical feasibility and aimed to determine the factors influencing intention to use Electronic Medical Records (EMRs) at Marie Stopes International, Myanmar (MSI-M).
Methods
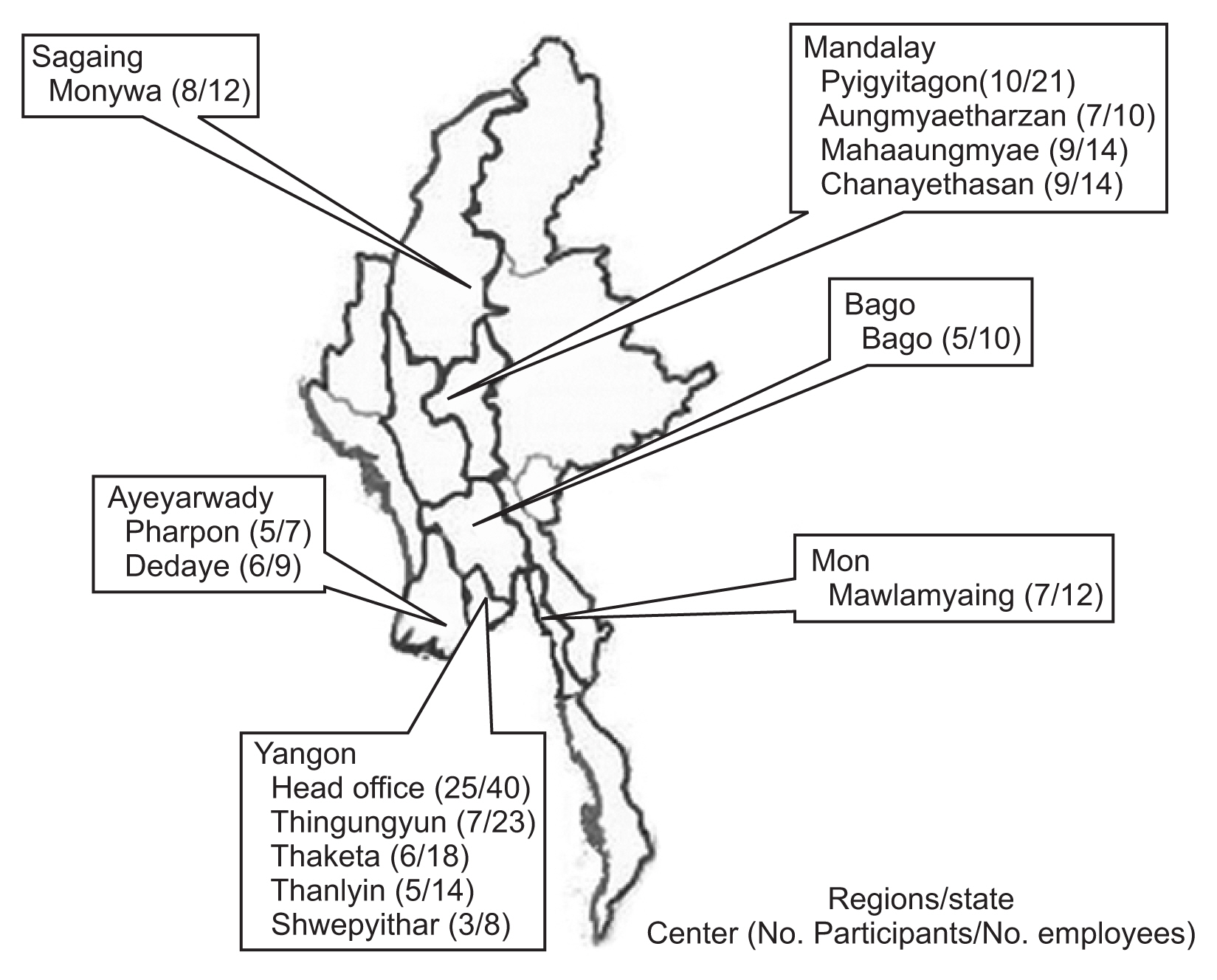
A cross-sectional survey was conducted among 112 participants who were working at the clinics and head office of MSI-M. Demographic information, type of office, technical feasibility, information communication technology knowledge, computer usage, and user acceptance towards the proposed system were obtained from the participants.
Results
The results indicated low health information technology usage and network availability at MSI-M clinics. Positive perception of EMRs was found among the staff members of MSI-M, which was reflected by positive responses regarding perceived usefulness (average score of 4.15), perceived ease of use (average score of 4.03), and intention to use (average score of 4.10) on a 5-point Likert scale. Statistically, staff from the head office expressed less desire to implement an EMR system (odds ratio = 0.07; 95% confidence interval, 0.01–0.97), especially when they do not perceive the usefulness of the system (odds ratio = 5.05; 95% confidence interval, 2.39–10.69).
Conclusions
Since health information technology usage and network availability were low in MSI-M, it is important to strengthen the information and communication technology infrastructure and introduce a policy for capacity building at MSI-M. Adequate training and strong leadership support are recommended for the successful initial implementation and sustainability of an EMR system at MSI-M.
Figure
Reference
-
References
1. Kruse CS, Kothman K, Anerobi K, Abanaka L. Adoption factors of the electronic health record: a systematic review. JMIR Med Inform. 2016; 4(2):e19.
Article2. Organisation for Economic Cooperation and Development. Health at a Glance: Europe 2018: State of Health in the EU Cycle. Paris, France: Organisation for Economic Cooperation and Development;2018.3. Hoyt RE, Sutton M, Yoshihashi A. Medical informatics: practical guide for the healthcare professional. Pensacola (FL): University of West Florida;2009.4. Aldosari B. Patients’ safety in the era of EMR/EHR automation. Informatics in Medicine Unlocked. 2017; 9:230–3.
Article5. Cook-Moine C, Cramer L. Financial savings from an electronic medical record in a small group practice. Chicago (IL): Healthcare Information and Management Systems Society Inc;2018.6. Alpert JS. The electronic medical record in 2016: Advantages and disadvantages. Digit Med. 2016; 2(2):48–51.
Article7. Evans RS. Electronic health records: then, now, and in the future. Yearb Med Inform. 2016; Suppl 1(Suppl 1):S48–61.
Article8. Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to electronic health record adoption: a systematic literature review. J Med Syst. 2016; 40(12):252.
Article9. Thit WM, Kaewkungwal J, Soonthornworasiri N, Theera-Ampornpunt N, Kijsanayotin B, Lawpoolsri S, et al. Electronic medical records in Myanmar: user perceptions at Marie Stopes International Clinics in Myanmar. Southeast Asian J Trop Med Public Health. 2016; 47(4):799–809.10. Watkinson-Powell A, Lee A. Benefits of an electronic medical records system in rural Nepal. JNMA J Nepal Med Assoc. 2012; 52(188):196–200.
Article11. Marie Stopes International. Where in the world, Myanmar [Internet]. London, UK: Marie Stopes International;c2020. [cited at 2020 Jul 25]. Available from: http://www.mariestopes.org/where-in-the-world#myanmar.12. Kijsanayotin B, Speedie S. Are health centers in Thailand ready for health information technology? A national survey. AMIA Annu Symp Proc. 2006; 2006:424–8.13. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989; 13(3):319–340.
Article14. Htun KS. An investigation of ICT development in Myanmar. Electron J Inf Syst Dev Ctries. 2019; 85(2):e12068.
Article15. Lewis T, Synowiec C, Lagomarsino G, Schweitzer J. E-health in low- and middle-income countries: findings from the Center for Health Market Innovations. Bull World Health Organ. 2012; 90(5):332–40.
Article16. Ayaad O, Alloubani A, ALhajaa EA, Farhan M, Abuseif S, Al Hroub A, et al. The role of electronic medical records in improving the quality of health care services: Comparative study. Int J Med Inform. 2019; 127:63–7.
Article17. Gidwani R, Nguyen C, Kofoed A, Carragee C, Rydel T, Nelligan I, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017; 15(5):427–33.
Article18. Thu SW, Kijsanayotin B, Kaewkungwal J, Soonthornworasiri N, Pan-Ngum W. Satisfaction with paper-based dental records and perception of electronic dental records among dental professionals in Myanmar. Healthc Inform Res. 2017; 23(4):304–13.
Article19. van der Zande MM, Gorter RC, Aartman IH, Wismeijer D. Adoption and use of digital technologies among general dental practitioners in the Netherlands. PLoS One. 2015; 10(3):e0120725.
Article20. Afrizal SH, Hidayanto AN, Handayani PW, Budiharsana M, Eryando T. Narrative review for exploring barriers to readiness of electronic health record implementation in primary health care. Healthc Inform Res. 2019; 25(3):141–52.
Article21. Muinga N, Magare S, Monda J, English M, Fraser H, Powell J, et al. Digital health systems in Kenyan Public Hospitals: a mixed-methods survey. BMC Med Inform Decis Mak. 2020; 20(1):2.
Article22. San AN, Yee CJ. The modified technology acceptance model for private clinical physicians: a case study in Malaysia, Penang. Int J Acad Res Bus Soc Sci. 2013; 3(2):380–403.23. Dünnebeil S, Sunyaev A, Blohm I, Leimeister JM, Krcmar H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int J Med Inform. 2012; 81(11):746–60.
Article24. Aggelidis VP, Chatzoglou PD. Using a modified technology acceptance model in hospitals. Int J Med Inform. 2009; 78(2):115–26.
Article25. Lorenzi NM, Riley RT. Organizational issues = change. Int J Med Inform. 2003; 69(2–3):197–203.26. Bevan A, Patel N. An electronic prescription alerting system-improving the discharge medicines process. Arch Dis Child. 2016; 101(9):e2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Satisfaction with Paper-Based Dental Records and Perception of Electronic Dental Records among Dental Professionals in Myanmar
- Factors affecting the users'satisfaction on the electronic medical record system
- Comparison of Nursing Records of Open Heart Surgery Patients before and after Implementation of Electronic Nursing Record
- User's Satisfaction on the Electronic Medical Record System in Seoul National University Bundang Hospital
- Adaptation Trends of Emergency Medical Personnel after Implementation of the Electronic Medical Record System into Emergency Care