Lab Med Online.
2020 Jul;10(3):250-254. 10.3343/lmo.2020.10.3.250.
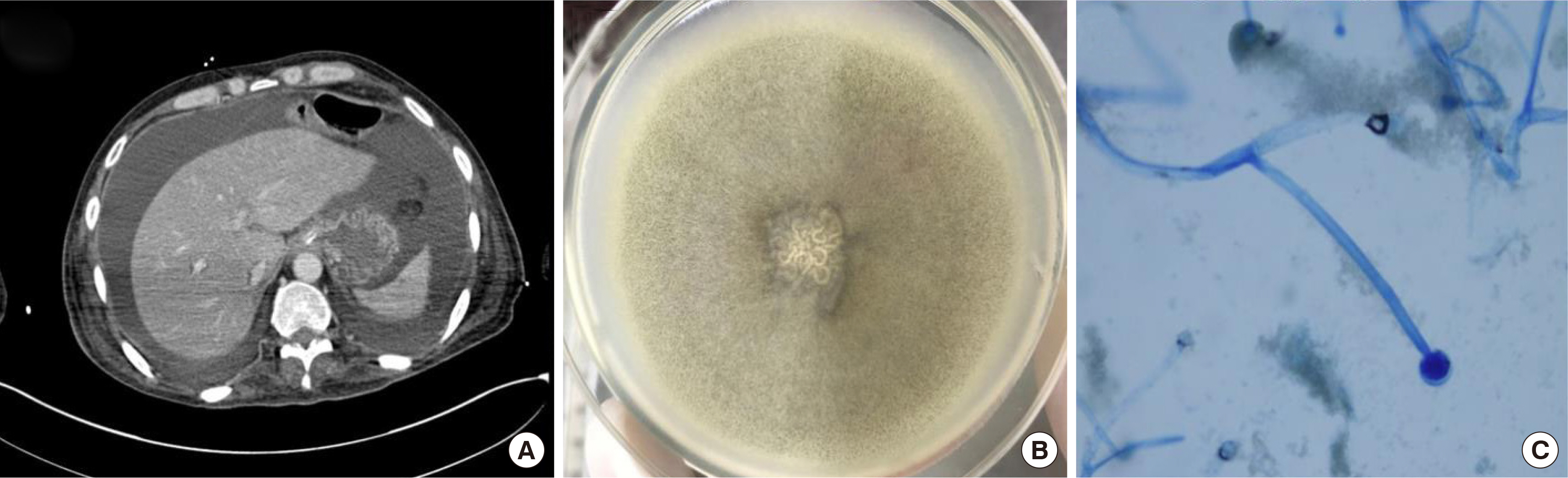
A Case of Peritonitis and Disseminated Mucormycosis Caused by Mucor circinelloides in a Patient with Nodal Marginal Zone B-cell Lymphoma
- Affiliations
-
- 1Department of Laboratory Medicine, Konkuk University School of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2504137
- DOI: http://doi.org/10.3343/lmo.2020.10.3.250
Abstract
- Mucormycosis is a fungal infection, which is difficult to treat due to its rapid dissemination and low susceptibility to anti-fungal agents. Peritonitis preceded by gastrointestinal mucormycosis is very rare, and only a few cases have been reported. We present a case of peritonitis and disseminated mucormycosis caused by Mucor circinelloides in an immunocompromised patient. A 59-year-old man, diagnosed with nodal marginal zone B-cell lymphoma, was diagnosed with liver failure due to severe septic shock. A white, woolly cotton-like growth, which was consistent with that of Mucor species, was isolated from ascites and sputum specimens. Targeted DNA sequencing confirmed the isolate as M. circinelloides with 100% identity. Despite anti-fungal treatment, the patient died after four days. This is a rare case of peritonitis and disseminated mucormycosis that was probably preceded by gastrointestinal mucormycosis caused by M. circinelloides, as determined by molecular methods. Accurate and rapid identification of mold using molecular methods might be necessary for early treatment in critical cases, and more cases should be clinically evaluated further.
Figure
Reference
-
1. Spellberg B, Edwards J, Ibrahim A. 2005; Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 18:556–69. DOI: 10.1128/CMR.18.3.556-569.2005. PMID: 16020690. PMCID: PMC1195964.
Article2. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. 2005; Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 41:634–53. DOI: 10.1086/432579. PMID: 16080086.
Article3. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. 2012; Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 54:S23–34. DOI: 10.1093/cid/cir866. PMID: 22247442.
Article4. Katragkou A, Walsh TJ, Roilides E. 2014; Why is mucormycosis more difficult to cure than more common mycoses? Clin Microbiol Infect. 20:74–81. DOI: 10.1111/1469-0691.12466. PMID: 24279587.
Article5. Monecke S, Hochauf K, Gottschlich B, Ehricht R. 2006; A case of peritonitis caused by Rhizopus microsporus. Mycoses. 49:139–42. DOI: 10.1111/j.1439-0507.2006.01190.x. PMID: 16466449.6. Hyvernat H, Dunais B, Burel-Vandenbos F, Guidicelli S, Bernardin G, Gari-Toussaint M. 2010; Fatal peritonitis caused by Rhizopus microsporus. Med Mycol. 48:1096–8. DOI: 10.3109/13693786.2010.485281. PMID: 20465520.7. Kumar C, Jain P, Wadhwa N, Diwaker P, Nirupma Panikar K. 2017; Nosocomial jejunal mucormycosis - an unusual cause of perforation peritonitis. Iran J Pathol. 12:295–300. PMID: 29531558. PMCID: PMC5835381.
Article8. Clinical and Laboratory Standards Institute. 2008; Interpretive criteria for identification of bacteria and fungi by DNA target sequencing: Approved guideline. CLSI document MM18-A. Clinical and Laboratory Standards Institute;Wayne, PA:9. Hartnett KP, Jackson BR, Perkins KM, Glowicz J, Kerins JL, Black SR, et al. 2019; A guide to investigating suspected outbreaks of mucormycosis in healthcare. J Fungi (Basel). 5:E69. DOI: 10.3390/jof5030069. PMID: 31344775. PMCID: PMC6787571.
Article10. Polo JR, Luño J, Menarguez C, Gallego E, Robles R, Hernandez P. 1989; Peritoneal mucormycosis in a patient receiving continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 13:237–9. DOI: 10.1016/S0272-6386(89)80058-7. PMID: 2919604.
Article11. Nannini EC, Paphitou NI, Ostrosky-Zeichner L. 2003; Peritonitis due to Aspergillus and zygomycetes in patients undergoing peritoneal dialysis: report of 2 cases and review of the literature. Diagn Microbiol Infect Dis. 46:49–54. DOI: 10.1016/S0732-8893(02)00554-0. PMID: 12742319.12. Serna JH, Wanger A, Dosekun AK. 2003; Successful treatment of mucormycosis peritonitis with liposomal amphotericin B in a patient on long-term peritoneal dialysis. Am J Kidney Dis. 42:E14–7. DOI: 10.1016/S0272-6386(03)00797-2. PMID: 12955706.
Article13. Pimentel JD, Dreyer G, Lum GD. 2006; Peritonitis due to Cunninghamella bertholletiae in a patient undergoing continuous ambulatory peritoneal dialysis. J Med Microbiol. 55:115–8. DOI: 10.1099/jmm.0.46202-0. PMID: 16388039.14. Bhutada K, Borkar SS, Mendiratta DK, Shende VR. 2012; Successful treatment of peritonitis by C. bertholletiae in a chronic kidney failure patient on continuous ambulatory peritoneal dialysis after kidney rejection. Singapore Med J. 53:e106–9. PMID: 22584986.15. Lee SC, Billmyre RB, Li A, Carson S, Sykes SM, Huh EY, et al. 2014; Analysis of a food-borne fungal pathogen outbreak: virulence and genome of a Mucor circinelloides isolate from yogurt. mBio. 5:e01390–14. DOI: 10.1128/mBio.01390-14. PMID: 25006230. PMCID: PMC4161253.
Article16. Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Cha-krabarti A, et al. 2014; ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect. 20(Suppl 3):5–26. DOI: 10.1111/1469-0691.12371. PMID: 24479848.
Article17. Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, Skiada A, et al. 2017; ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica. 102:433–44. DOI: 10.3324/haematol.2016.152900. PMID: 28011902. PMCID: PMC5394968.
Article18. Yang M, Lee JH, Kim YK, Ki CS, Huh HJ, Lee NY. 2016; Identification of Mucorales from clinical specimens: a 4-year experience in a single institution. Ann Lab Med. 36:60–3. DOI: 10.3343/alm.2016.36.1.60. PMID: 26522761. PMCID: PMC4697345.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of nodal marginal zone B-cell lymphoma of the lower eyelid
- A Case of Primary Nodal Type Marginal Zone B-Cell Lymphoma of the Intra-Parotid Lymph Node Mistaken to Primary Benign Parotid Mass
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- A Case of Mucosa-Associated Lymphoid Tissue Lymphoma in Nasopharynx and Thyroid Gland