Ann Surg Treat Res.
2020 Jul;99(1):8-17. 10.4174/astr.2020.99.1.8.
18F-fluorodeoxyglucose PET/CT as an independent predictor for patients with hepatocellular carcinoma combined with major portal vein tumor thrombus
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Intervention, Department of Surgery, Jiangxi Cancer Hospital, Nan Chang, China
- 2Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- 3Department of Clinical Medicine, Jiangxi Health Career College of China, Nan Chang, China
- 4Health Insurance Review and Assessment Service, Seoul, Korea
- 5Department of Nuclear Medicine and Molecular Imaging, Ajou University School of Medicine, Suwon, Korea
- KMID: 2503455
- DOI: http://doi.org/10.4174/astr.2020.99.1.8
Abstract
- Purpose
Hepatocellular carcinoma (HCC) patients with major portal vein tumor thrombosis (mPVTT) complications were generally characterized by extremely poor prognoses. The aim of this study was to explore the role of 18F-fluorodeoxyglucose (18F-FDG) PET/CT imaging in predicting HCC complicated by mPVTT.
Methods
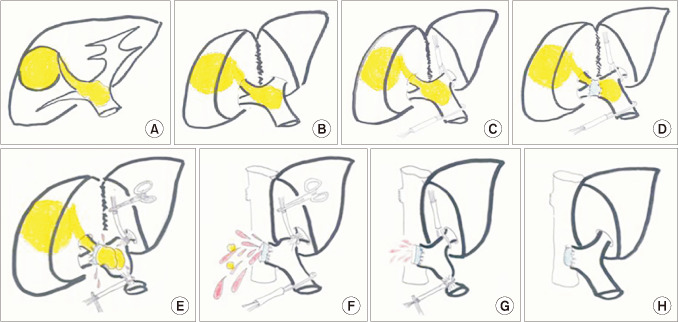
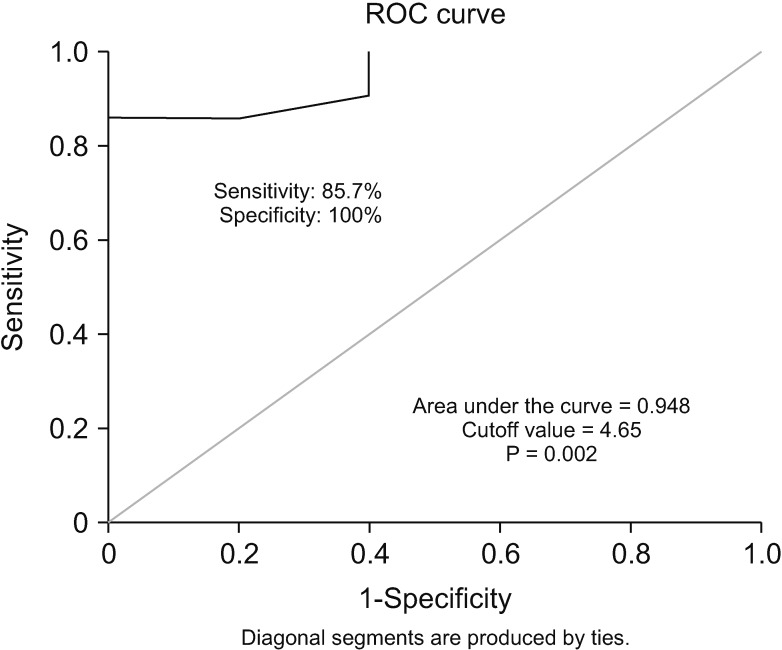
Five hundred one HCC patients received surgery in our hospital during November 2008 to December 2014, among which 32 patients (6.4%) were diagnosed as HCC complicated by mPVTT. Six cases were excluded for reasons of complex medical conditions, including 2 cases of salvage liver transplantation, 2 cases of re-resection, 1 case of mPVTT combined with inferior vina cava tumor thrombosis, and 1 case of residual portal vein tumor thrombosis. Ultimately, 26 cases were enrolled in this study. The maximal tumor standardized uptake value (SUVmax) was identified as a predictive factor and detected. The univariate and multivariate regression analyses were performed to identify the prognostic factors for recurrence-free survival (RFS) and overall survival (OS) of HCC patients complicated by mPVTT.
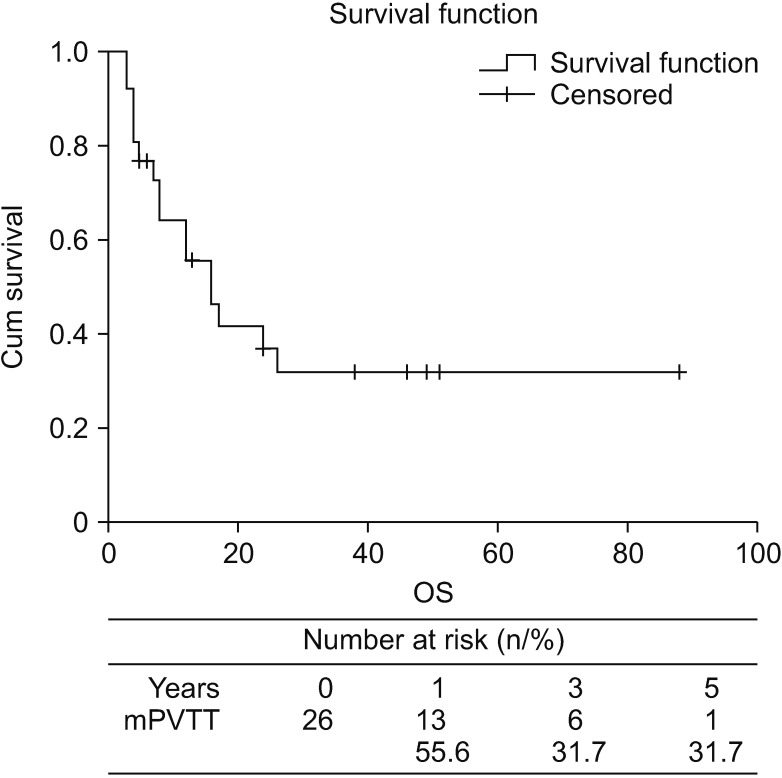
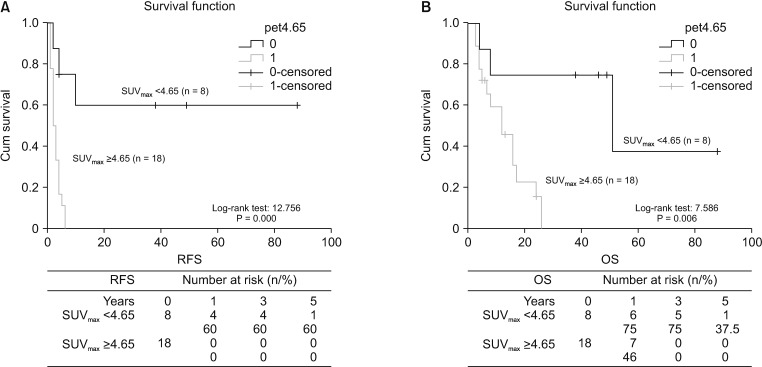
Results
Our results showed that the median OS was 16 months. The 1-, 3-, and 5-year cumulative OS was 55.6%, 31.7%, and 31.7%, respectively. The multivariate regression analysis revealed that SUVmax ≥ 4.65 was the only independent risk factor for RFS and OS.
Conclusion
SUVmax was an independent predictor for RFS and OS of patients suffering from both HCC and mPVTT. L ow SUVmax could serve as an effective factor for selecting candidates with low recurrence risks and for helping with improving patient survival after surgical resection.
Keyword
Figure
Reference
-
1. Ikai I, Yamamoto Y, Yamamoto N, Terajima H, Hatano E, Shimahara Y, et al. Results of hepatic resection for hepatocellular carcinoma invading major portal and/or hepatic veins. Surg Oncol Clin N Am. 2003; 12:65–75. PMID: 12735130.2. Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999; 29:62–67. PMID: 9862851.3. Villa E, Moles A, Ferretti I, Buttafoco P, Grottola A, Del Buono M, et al. Natural history of inoperable hepatocellular carcinoma: estrogen receptors' status in the tumor is the strongest prognostic factor for survival. Hepatology. 2000; 32:233–238. PMID: 10915729.4. Iwao I, Masatoshi K, Shigeki A, Masao O, Masamichi K, Michiie S, et al. Report of the 18th follow-up survey of primary liver cancer in Japan. Hepatol Res. 2010; 40:1043–1059.5. Kokudo T, Hasegawa K, Matsuyama Y, Takayama T, Izumi N, Kadoya M, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 2016; 65:938–943. PMID: 27266618.6. Poon RT, Fan ST, Ng IO, Wong J. Prognosis after hepatic resection for stage IVA hepatocellular carcinoma: a need for reclassification. Ann Surg. 2003; 237:376–383. PMID: 12616122.7. Ikai I, Hatano E, Hasegawa S, Fujii H, Taura K, Uyama N, et al. Prognostic index for patients with hepatocellular carcinoma combined with tumor thrombosis in the major portal vein. J Am Coll Surg. 2006; 202:431–438. PMID: 16500247.8. Ban D, Shimada K, Yamamoto Y, Nara S, Esaki M, Sakamoto Y, et al. Efficacy of a hepatectomy and a tumor thrombectomy for hepatocellular carcinoma with tumor thrombus extending to the main portal vein. J Gastrointest Surg. 2009; 13:1921–1928. PMID: 19727969.9. Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003; 138:1198–1206. PMID: 14609867.10. Kenjo A, Miyata H, Gotoh M, Kitagawa Y, Shimada M, Baba H, et al. Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg. 2014; 218:412–422. PMID: 24468222.11. Choi KK, Kim SH, Choi SB, Lim JH, Choi GH, Choi JS, et al. Portal venous invasion: the single most independent risk factor for immediate postoperative recurrence of hepatocellular carcinoma. J Gastroenterol Hepatol. 2011; 26:1646–1651. PMID: 21592228.12. Torizuka T, Tamaki N, Inokuma T, Magata Y, Yonekura Y, Tanaka A, et al. Value of fluorine-18-FDG-PET to monitor hepatocellular carcinoma after interventional therapy. J Nucl Med. 1994; 35:1965–1969. PMID: 7989978.13. Hatano E, Ikai I, Higashi T, Teramukai S, Torizuka T, Saga T, et al. Preoperative positron emission tomography with fluorine-18-fluorodeoxyglucose is predictive of prognosis in patients with hepatocellular carcinoma after resection. World J Surg. 2006; 30:1736–1741. PMID: 16850145.14. Seo S, Hatano E, Higashi T, Hara T, Tada M, Tamaki N, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography predicts tumor differentiation, P-glycoprotein expression, and outcome after resection in hepatocellular carcinoma. Clin Cancer Res. 2007; 13:427–433. PMID: 17255262.15. Shiomi S, Nishiguchi S, Ishizu H, Iwata Y, Sasaki N, Tamori A, et al. Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose for predicting outcome in patients with hepatocellular carcinoma. Am J Gastroenterol. 2001; 96:1877–1880. PMID: 11419843.16. Matono R, Yoshiya S, Motomura T, Toshima T, Kayashima H, Masuda T, et al. Factors linked to longterm survival of patients with hepatocellular carcinoma accompanied by tumour thrombus in the major portal vein after surgical resection. HPB (Oxford). 2012; 14:247–253. PMID: 22404263.17. Pawlik TM, Poon RT, Abdalla EK, Ikai I, Nagorney DM, Belghiti J, et al. Hepatectomy for hepatocellular carcinoma with major portal or hepatic vein invasion: results of a multicenter study. Surgery. 2005; 137:403–410. PMID: 15800485.18. Kondo K, Chijiiwa K, Kai M, Otani K, Nagaike K, Ohuchida J, et al. Surgical strategy for hepatocellular carcinoma patients with portal vein tumor thrombus based on prognostic factors. J Gastrointest Surg. 2009; 13:1078–1083. PMID: 19296182.19. Trojan J, Schroeder O, Raedle J, Baum RP, Herrmann G, Jacobi V, et al. Fluorine-18 FDG positron emission tomography for imaging of hepatocellular carcinoma. Am J Gastroenterol. 1999; 94:3314–3319. PMID: 10566736.20. Khan MA, Combs CS, Brunt EM, Lowe VJ, Wolverson MK, Solomon H, et al. Positron emission tomography scanning in the evaluation of hepatocellular carcinoma. J Hepatol. 2000; 32:792–797. PMID: 10845666.21. Kim JM, Kwon CHD, Joh JW, Sinn DH, Choi GS, Paik SW. Prognosis of preoperative positron emission tomography uptake in hepatectomy patients. Ann Surg Treat Res. 2018; 94:183–189. PMID: 29629352.22. Inoue Y, Hasegawa K, Ishizawa T, Aoki T, Sano K, Beck Y, et al. Is there any difference in survival according to the portal tumor thrombectomy method in patients with hepatocellular carcinoma? Surgery. 2009; 145:9–19. PMID: 19081470.23. Chok KS, Cheung TT, Chan SC, Poon RT, Fan ST, Lo CM. Surgical outcomes in hepatocellular carcinoma patients with portal vein tumor thrombosis. World J Surg. 2014; 38:490–496. PMID: 24132826.24. Mano Y, Aishima S, Kubo Y, Tanaka Y, Motomura T, Toshima T, et al. Correlation between biological marker expression and fluorine-18 fluorodeoxyglucose uptake in hepatocellular carcinoma. Am J Clin Pathol. 2014; 142:391–397. PMID: 25125631.25. Kitamura K, Hatano E, Higashi T, Narita M, Seo S, Nakamoto Y, et al. Proliferative activity in hepatocellular carcinoma is closely correlated with glucose metabolism but not angiogenesis. J Hepatol. 2011; 55:846–857. PMID: 21334407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonographic features of portal vein thrombosis
- Hemodynamic Change by Portal Tumor Thrombus in Hepatocellular Carcinoma: Evaluation by Combined Spiral CT Hepatic Arteriography and CT Arterial Portography
- A Case of Gastric Adenocarcinoma Presenting as Portal Hypertension
- Hepatic Resection in Patients with Hepatocellular Carcinoma Accompanied by Portal Vein Thrombus
- 3 Cases of Portal Vein Thrombosis in Hepatocellular Carcinoma and Liver Cirrhosis Treated with Anticoagulation