Korean J Gastroenterol.
2012 Jul;60(1):42-46. 10.4166/kjg.2012.60.1.42.
A Case of Gastric Adenocarcinoma Presenting as Portal Hypertension
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University College of Medicine, Seoul, Korea. jwchulkr@yahoo.co.kr
- 2Department of Surgery, The Catholic University College of Medicine, Seoul, Korea.
- KMID: 1718465
- DOI: http://doi.org/10.4166/kjg.2012.60.1.42
Abstract
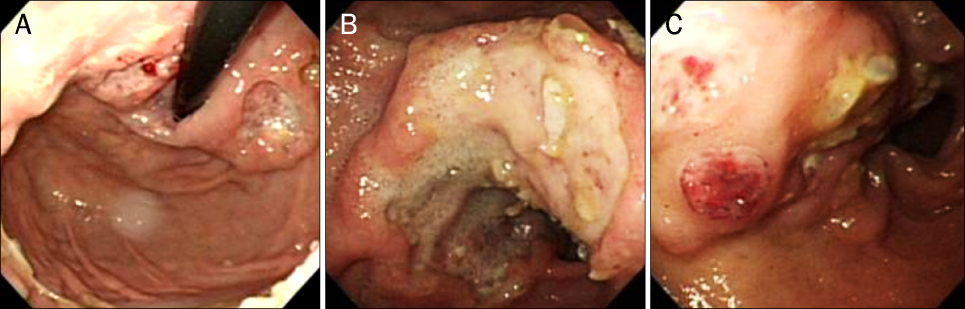
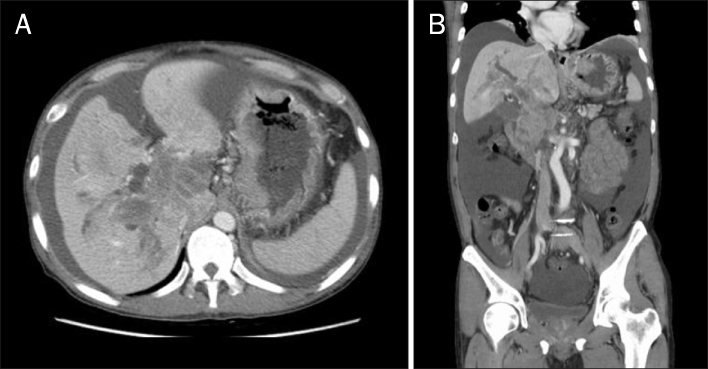
- Portal vein thrombus has been detected in patients with liver cirrhosis, pancreatitis, ulcerative colitis, septicemia, myeloproliferative disorder, and neoplasm. The formation of portal tumor thrombus by hepatocellular carcinoma is well recognized, because of its high incidence, and subsequent development of portal hypertension such as rupture of varices, ascites and liver failure indicates the poor prognosis. In gastric cancer, portal hypertension as an initial presentation is extremely rare. Herein we report a case presenting as portal hypertension caused by tumor thrombus without invasion of liver parenchyma. It is presumed to be intraluminal tumor thrombus originating from primary foci of gastric adenocarcinoma. Tumor thrombus in the portal vein is demonstrated on the PET-CT.
Keyword
MeSH Terms
Figure
Reference
-
1. Ishikawa M, Koyama S, Ikegami T, et al. Venous tumor thrombosis and cavernous transformation of the portal vein in a patient with gastric carcinoma. J Gastroenterol. 1995. 30:529–533.2. Tanaka A, Takeda R, Mukaihara S, et al. Tumor thrombi in the portal vein system originating from gastrointestinal tract cancer. J Gastroenterol. 2002. 37:220–228.3. Ghosh P, Miyai K, Chojkier M. Gastric adenocarcinoma inducing portal hypertension: a rare presentation. World J Gastroenterol. 2007. 13:960–963.4. Lee TH. Recent advances in diagnosis of portal hypertension. Korean J Gastroenterol. 2010. 56:135–143.5. Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Portal Hypertension Collaborative Group. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005. 353:2254–2261.6. Ripoll C, Groszmann R, Garcia-Tsao G, et al. Portal Hypertension Collaborative Group. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 2007. 133:481–488.7. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med. 1983. 102:260–273.8. Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000. 32:689–692.9. Kim YS. Ascites, hepatorenal syndrome and spontaneous bacterial peritonitis in patients with portal hypertension. Korean J Gastroenterol. 2010. 56:168–185.10. Cohen J, Edelman RR, Chopra S. Portal vein thrombosis: a review. Am J Med. 1992. 92:173–182.11. Valla DC, Condat B. Portal vein thrombosis in adults: pathophysiology, pathogenesis and management. J Hepatol. 2000. 32:865–871.12. Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH. Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows. Hepatology. 1992. 16:715–718.13. Ohnishi K, Okuda K, Ohtsuki T, et al. Formation of hilar collaterals or cavernous transformation after portal vein obstruction by hepatocellular carcinoma. Observations in ten patients. Gastroenterology. 1984. 87:1150–1153.14. Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006. 12:2115–2119.15. Araki T, Suda K, Sekikawa T, Ishii Y, Hihara T, Kachi K. Portal venous tumor thrombosis associated with gastric adenocarcinoma. Radiology. 1990. 174:811–814.16. Liu X, Cheng Y, Sheng W, et al. Analysis of clinicopathologic features and prognostic factors in hepatoid adenocarcinoma of the stomach. Am J Surg Pathol. 2010. 34:1465–1471.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Klippel-Trenaunay-Weber Syndrome Presenting with Esophageal and Gastric Varices Bleeding
- Congenital Absence of the Portal Vein Presenting as Pulmonary Hypertension
- A Case of Esophageal Variceal Bleeding in a Child Secondary to Portal Hypertension Associated with Cavernous Transformation of the Portal Vein Suggesting Extrahepatic Portal Obstruction
- Distal pancreatectomy with splenorenal shunt to preserve spleen in a cirrhotic patient
- Diagnosis and Management of Esophageal and Gastric Variceal Bleeding: Focused on 2019 KASL Clinical Practice Guidelines for Liver Cirrhosis