J Neurocrit Care.
2020 Jun;13(1):41-48. 10.18700/jnc.190114.
Safety and feasibility of ultrasound-guided insertion of peripherally inserted central catheter performed by an intensive care trainee
- Affiliations
-
- 1Department of Neurology, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Republic of Korea
- 2Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 3Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 4Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- KMID: 2503384
- DOI: http://doi.org/10.18700/jnc.190114
Abstract
- Background
We investigated the safety and feasibility of ultrasound-guided peripherally inserted central venous catheter (PICC) placements performed by intensive care medical trainees in comparison to PICC placements performed by intensivists.
Methods
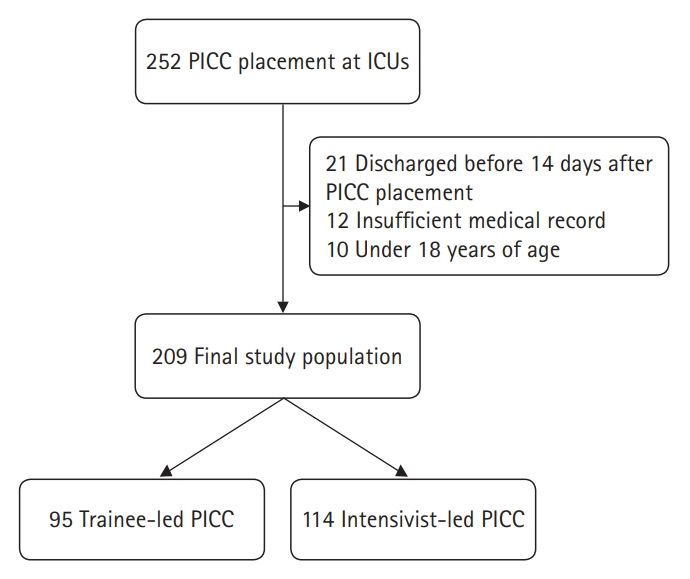
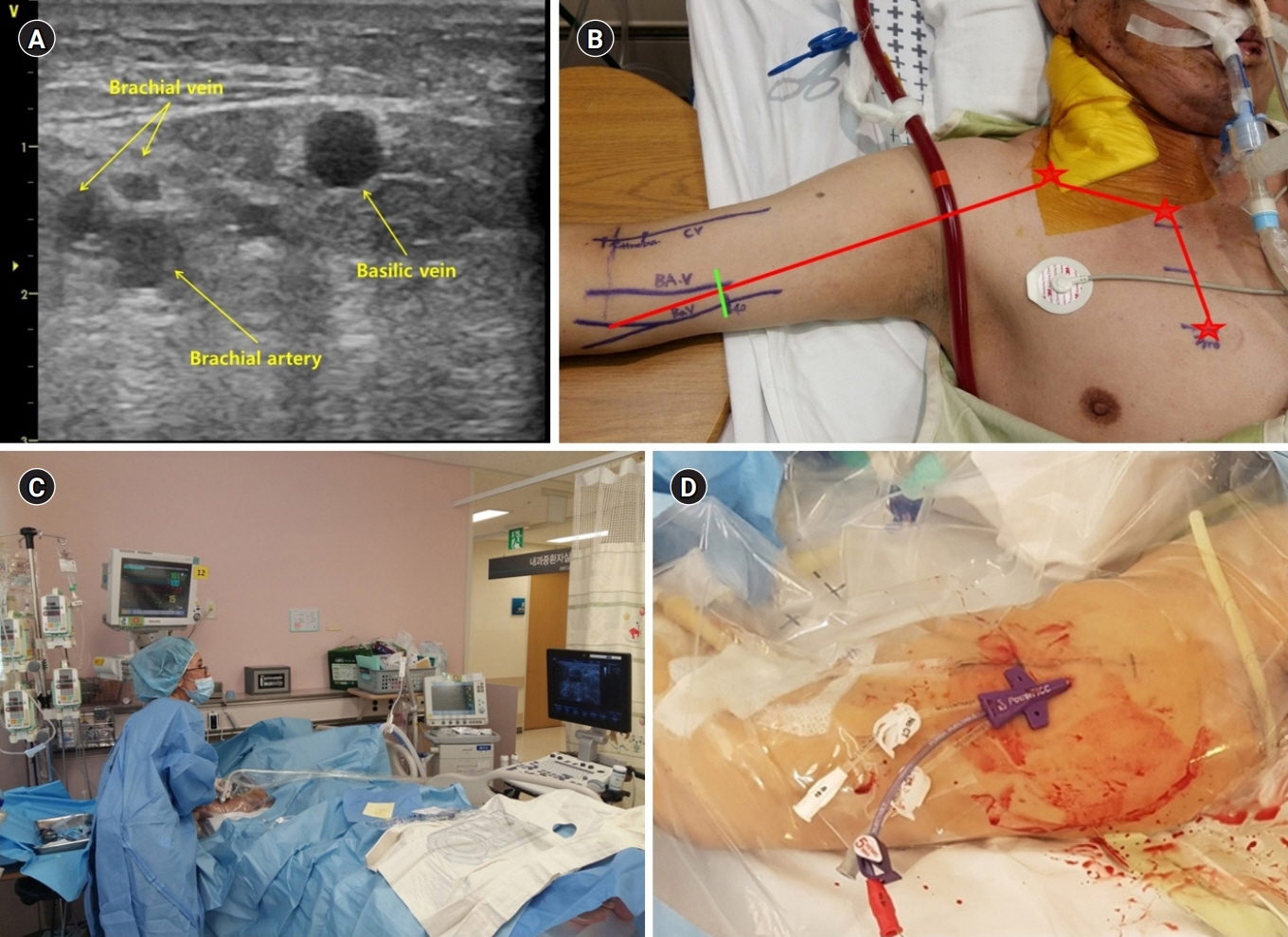
This was a retrospective and observational study of adult patients who underwent PICC placement and were admitted to the intensive care unit (ICU) between July 2013 and March 2018. Ultrasound-guided PICC was performed at the bedside by an intensivist or intensive care medical trainee if intrahospital transport was inappropriate. The primary endpoint was PICC-induced complications. The secondary endpoint was initial success of PICC.
Results
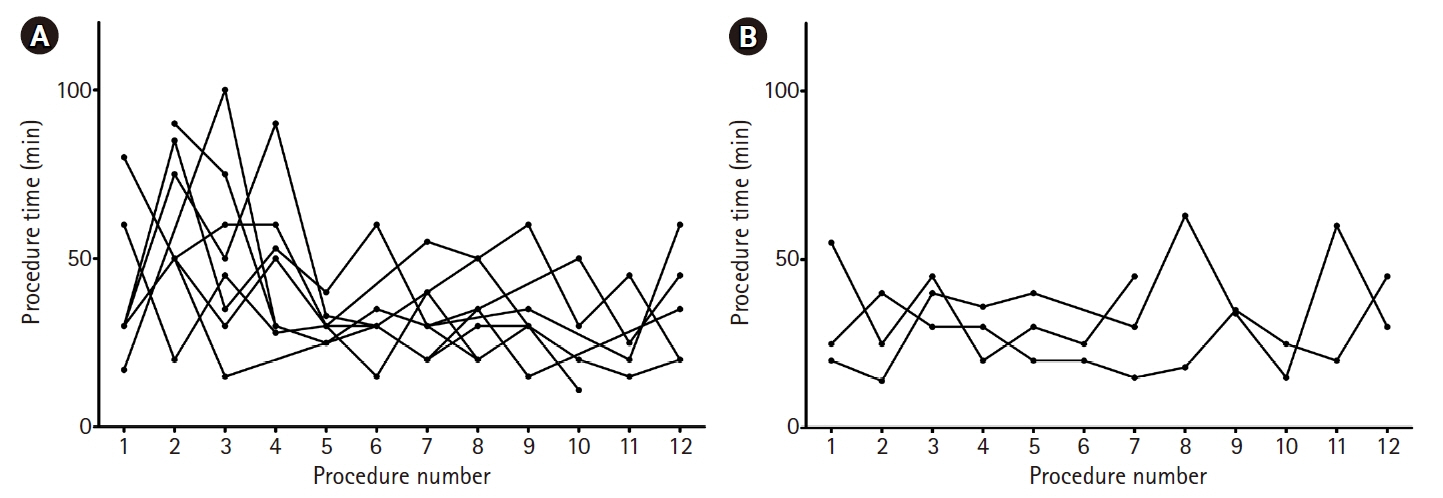
A total of 209 patients underwent PICC placement during the study period. There were no significant differences in age, sex, body mass index, comorbidities, causes of ICU admission, or severity scores between the trainee-led PICC and intensivist-led PICC groups. Difficult venous access (42.6%) and requirement for central line infusion (39.2%) were the most common reasons for PICC placement. The basilic vein (62.2%) was the most common target vein among patients who underwent PICC. There were no significant differences in complications between the two groups (P=0.473). In addition, the initial success rate and procedural time were similar between the two groups (P=0.108 and P=0.076, respectively). There were no insertional injuries and moderate or severe bleeding in patients with PICC.
Conclusion
Ultrasound-guided PICC placement by an intensive care medical trainee may be safer and more feasible compared to PICC placement by an intensivist.
Keyword
Figure
Reference
-
1. Pittiruti M, Brutti A, Celentano D, Pomponi M, Biasucci DG, Annetta MG, et al. Clinical experience with power-injectable PICCs in intensive care patients. Crit Care. 2012; 16:R21.
Article2. Potet J, Arnaud FX, Thome A, Weber-Donat G, Konopacki J, Bouzad C, et al. Peripherally inserted central catheter placement in patients with coagulation disorders: a retrospective analysis. Diagn Interv Imaging. 2015; 96:1147–51.
Article3. Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M; ESPEN. ESPEN guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009; 28:365–77.
Article4. Wilson TJ, Stetler WR Jr, Fletcher JJ. Comparison of catheter-related large vein thrombosis in centrally inserted versus peripherally inserted central venous lines in the neurological intensive care unit. Clin Neurol Neurosurg. 2013; 115:879–82.
Article5. Wilson TJ, Brown DL, Meurer WJ, Stetler WR Jr, Wilkinson DA, Fletcher JJ. Risk factors associated with peripherally inserted central venous catheter-related large vein thrombosis in neurological intensive care patients. Intensive Care Med. 2012; 38:272–8.
Article6. Donovan MS, Thomas KD, Davis DC, Hawkins K, Harris DS. Peripherally inserted central catheters: placement and use in a family practice hospital. J Am Board Fam Pract. 1996; 9:235–40.7. Andrews JC, Marx MV, Williams DM, Sproat I, Walker-Andrews SC. The upper arm approach for placement of peripherally inserted central catheters for protracted venous access. AJR Am J Roentgenol. 1992; 158:427–9.
Article8. Lee DS, Park CM. Clinical feasibility of ultrasound guided placement of peripherally inserted central catheters by intensivist: preliminary report. J Acute Care Surg. 2014; 4:13–7.
Article9. Parmentier-Decrucq E, Poissy J, Favory R, Nseir S, Onimus T, Guerry MJ, et al. Adverse events during intrahospital transport of critically ill patients: incidence and risk factors. Ann Intensive Care. 2013; 3:10.
Article10. Schwebel C, Clec'h C, Magne S, Minet C, Garrouste-Orgeas M, Bonadona A, et al. Safety of intrahospital transport in ventilated critically ill patients: a multicenter cohort study. Crit Care Med. 2013; 41:1919–28.11. Kim YO, Chung CR, Gil E, Park CM, Suh GY, Ryu JA. Safety and feasibility of ultrasound-guided placement of peripherally inserted central catheter performed by neurointensivist in neurosurgery intensive care unit. PLoS One. 2019; 14:e0217641.
Article12. Lee D, Chung CR, Park SB, Ryu JA, Cho J, Yang JH, et al. Safety and feasibility of percutaneous dilatational tracheostomy performed by intensive care trainee. Korean J Crit Care Med. 2014; 29:64–9.
Article13. Maki DG, Stolz SM, Wheeler S, Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter. A randomized, controlled trial. Ann Intern Med. 1997; 127:257–66.14. Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest. 2005; 128:489–95.
Article15. Ryder MA. Peripherally inserted central venous catheters. Nurs Clin North Am. 1993; 28:937–71.16. Griffiths VR, Philpot P. Peripherally inserted central catheters (PICCs): do they have a role in the care of the critically ill patient? Intensive Crit Care Nurs. 2002; 18:37–47.
Article17. DeLemos C, Abi-Nader J, Akins PT. Use of peripherally inserted central catheters as an alternative to central catheters in neurocritical care units. Crit Care Nurse. 2011; 31:70–5.
Article18. Rotzinger R, Gebauer B, Schnapauff D, Streitparth F, Wieners G, Grieser C, et al. Placement of central venous port catheters and peripherally inserted central catheters in the routine clinical setting of a radiology department: analysis of costs and intervention duration learning curve. Acta Radiol. 2017; 58:1468–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peripherally inserted central catheter procedure at the bedside by a nephrologist is safe and successful
- Bedside Ultrasound-Guided Peripherally Inserted Central Catheter Placement by Critical Care Fellows in Critically Ill Patients: A Feasibility and Safety Study
- Safety and Feasibility of Ultrasound-guided Peripherally Inserted Central Catheterization for Chemo-Delivery
- Safety and Efficacy of Peripherally Inserted Central Catheter Placement by Surgical Intensivist–Led Vascular Access Team
- Clinical Characteristics of Peripherally Inserted Central Catheter in Critically Ill Patients