J Educ Eval Health Prof.
2019;16:11. 10.3352/jeehp.2019.16.11.
Analysis of the Clinical Education Situation framework: a tool for identifying the root cause of student failure in the United States
- Affiliations
-
- 1Doctor of Physical Therapy Division, Duke University School of Medicine, Durham, NC, USA
- KMID: 2502156
- DOI: http://doi.org/10.3352/jeehp.2019.16.11
Abstract
- Doctor of physical therapy preparation requires extensive time in precepted clinical education, which involves multiple stakeholders. Student outcomes in clinical education are impacted by many factors, and, in the case of failure, it can be challenging to determine which factors played a primary role in the poor result. Using existing root-cause analysis processes, the authors developed and implemented a framework designed to identify the causes of student failure in clinical education. This framework, when applied to a specific student failure event, can be used to identify the factors that contributed to the situation and to reveal opportunities for improvement in both the clinical and academic environments. A root-cause analysis framework can help to drive change at the programmatic level, and future studies should focus on the framework’s application to a variety of clinical and didactic settings.
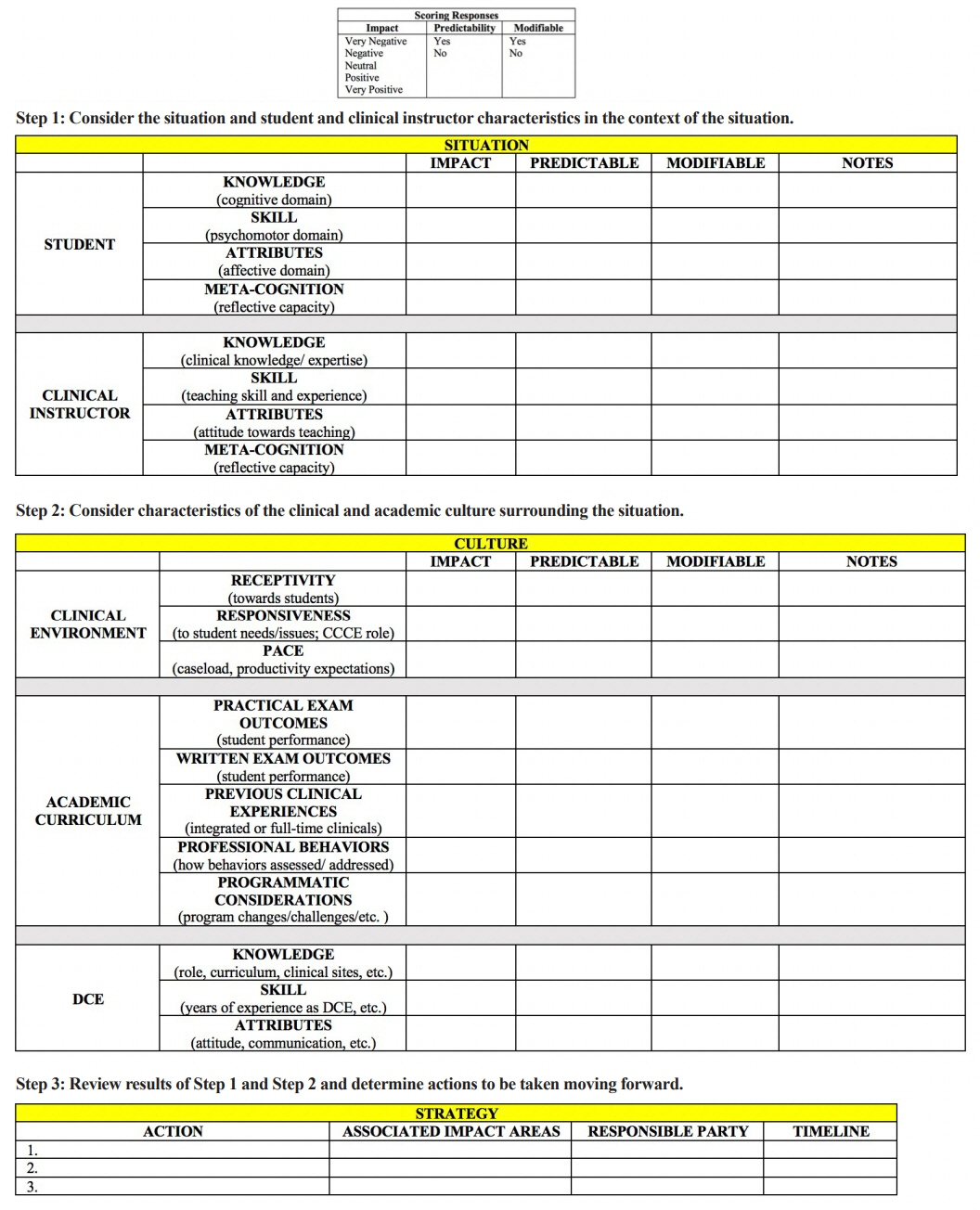
Figure
Reference
-
References
1. Commission on Accreditation in Physical Therapy Education. Aggregate program data: 2018-2019 physical therapist education programs fact sheets [Internet]. Alexandria (VA): American Physical Therapy Association;2019. [cited 2018 Apr 20]. Available from: http://www.capteonline.org/uploadedFiles/CAPTEorg/About_CAPTE/Resources/Aggregate_Program_Data/AggregateProgramData_PTPrograms.pdf#search=%22fact.2. Commission on Accreditation of Physical Therapy Education. Evaluative criteria for accreditation of education programs for the preparation of physical therapists. Alexandria (VA): American Physical Therapy Association;2015.3. Recker-Hughes C, Wetherbee E, Buccieri KM, FitzpatrickTimmerberg J, Stolfi AM. Essential characteristics of quality clinical education experiences: standards to facilitate student learning. J Phys Ther Educ. 2014; 28:48–55. https://doi.org/10.1097/00001416-201400001-00009.
Article4. National Patient Safety Foundation. RCA2: improving root cause analyses and actions to prevent harm. Boston (MA): National Patient Safety Foundation;2016.5. Swamy L, Worsham C, Bialas MJ, Wertz C, Thornton D, Breu A, Ronan M. The 60-minute root cause analysis: a workshop to engage interdisciplinary clinicians in quality improvement. MedEdPORTAL. 2018; 14:10685. https://doi.org/10.15766/mep_2374-8265.10685.
Article6. Cohen DM, Clinchot DM, Werman HA. A framework for analysis of sentinel events in medical student education. Acad Med. 2013; 88:1680–1684. https://doi.org/10.1097/ACM.0b013e3182a82266.
Article7. Deis JM, Smith KM, Warren MD, Throop P, Hickson G, Joers B. Transforming the morbidity and mortality conference into an instrument for systemwide improvement. In : Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in patient safety: new directions and alternative approaches. Rockville (MD): Agency for Healthcare Research and Quality;2008.8. Ohrn A, Ericsson C, Andersson C, Elfstrom J. High rate of implementation of proposed actions for improvement with the healthcare failure mode effect analysis method: evaluation of 117 analyses. J Patient Saf. 2018; 14:17–20. https://doi.org/10.1097/PTS.0000000000000159.
Article9. Jensen GM, Nordstrom T, Mostrom E, Hack LM, Gwyer J. National study of excellence and innovation in physical therapist education: part 1-design, method, and results. Phys Ther. 2017; 97:857–874. https://doi.org/10.1093/ptj/pzx061.
Article10. Patton N, Higgs J, Smith M. Clinical learning spaces: crucibles for practice development in physiotherapy clinical education. Physiother Theory Pract. 2018; 34:589–599. https://doi.org/10.1080/09593985.2017.1423144.
Article11. VA National Center for Patient Safety. Root cause analysis tools. Washington (DC): VA National Center for Patient Safety;2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Geriatrics Education and Training Experience in the United States
- Impact of individualized learning plans on United States senior medical students advanced clinical rotations
- Current Situation of Medical Ethics Education in the United States of America
- Nursing Education Systems in Korea, China and the United States of America and its Future Directions
- Self-care perspective taking and empathy in a student-faculty book club in the United States