Effects of a Mobile-App-Based Self-Management Support Program For Elderly Hemodialysis Patients
- Affiliations
-
- 1Hemodialysis Unit, Chungnam National University Hospital, Daejeon,
- 2College of Nursing, Chungnam National University, Daejeon,
- KMID: 2501334
- DOI: http://doi.org/10.4258/hir.2020.26.2.93
Abstract
Objectives To identify the effects of a mobile-app-based self-management program for elderly hemodialysis patients on their sick-role behavior, basic psychological needs, and self-efficacy.
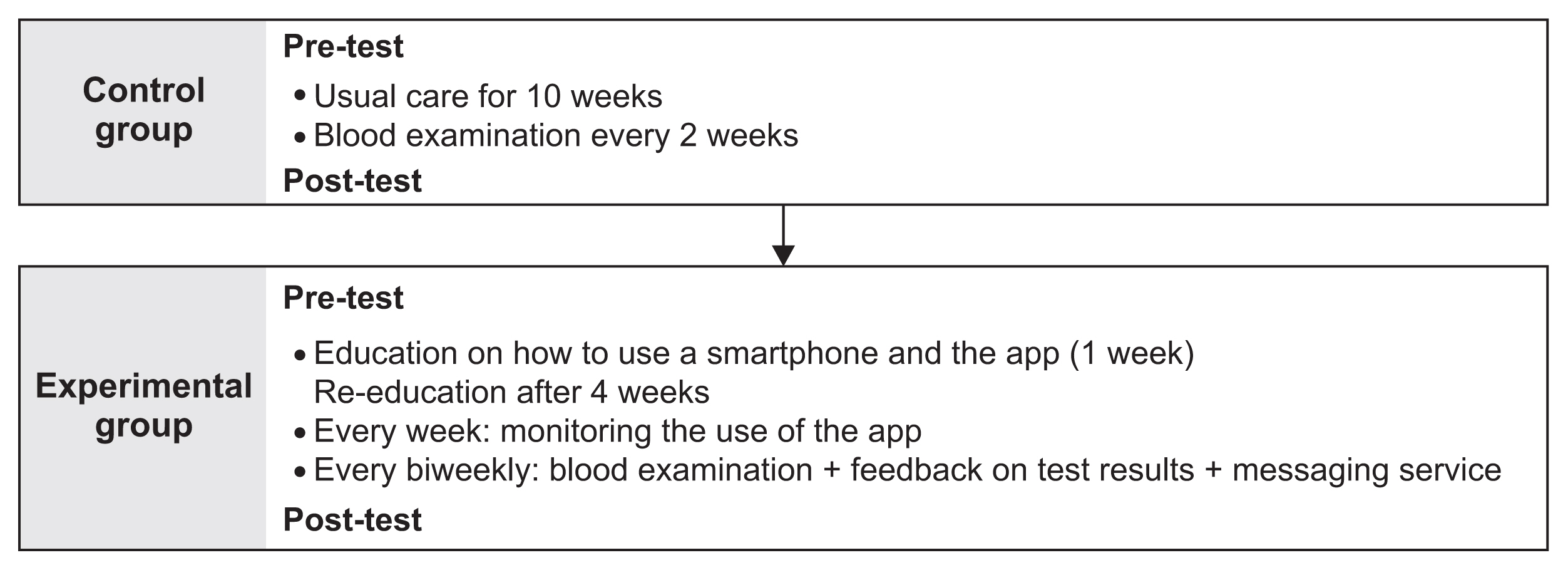
Methods A nonequivalent control group with a non-synchronized design was utilized, and 60 participants (30 in each of the experimental and control groups) were recruited from Chungnam National University Hospital from March to August 2018. The program consisted of continuous training on how to use the mobile-app, self-checking via the app, message transfer through Electronic Medical Records, and feedback. The control group received the usual care. Data were analyzed using the χ2-test, the
t -test, the repeated-measures ANOVA, and the McNemar test. A formalized messaging program was developed, and the app was developed with consideration of the specific physical and cognitive limitations of the elderly.Results Comparisons were conducted between the experimental (n = 28) and control (n = 28) groups. Statistically significant increases in sick-role behavior, basic psychological needs, and self-efficacy were found in the experimental group (
p < 0.001). Physiological parameters were maintained within the normal ranges in the experimental group, and the number of non-adherent patients decreased, although the change was not statistically significant.Conclusions The mobile-app-based self-management program developed in this study increased the sick-role behavior, basic psychological needs, and self-efficacy of elderly hemodialysis patients, while physiological parameters were maintained within the normal range. Future studies are needed to develop management systems for high-risk hemodialysis patients and family-sharing apps to manage non-adherent patients.
Figure
Reference
-
References
1. Jin DC, Shin Y, Kim M, Kang M, Won E, Yang K. Analysis of hemodialysis therapy variation associated with periodic hemodialysis quality assessment by government in Korea. Korean J Med. 2018; 93(2):194–205.
Article2. Kalantar-Zadeh K, Regidor DL, Kovesdy CP, Van Wyck D, Bunnapradist S, Horwich TB, et al. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009; 119(5):671–9.
Article3. Cupisti A, Gallieni M, Rizzo MA, Caria S, Meola M, Bolasco P. Phosphate control in dialysis. Int J Nephrol Renovasc Dis. 2013; 6:193–205.
Article4. Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, et al. Executive summary of the 2017 KDI-GO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney Int. 2017; 92(1):26–36.5. Brunelli SM, Du Mond C, Oestreicher N, Rakov V, Spiegel DM. Serum potassium and short-term clinical outcomes among hemodialysis patients: impact of the long interdialytic interval. Am J Kidney Dis. 2017; 70(1):21–9.
Article6. Karaboyas A, Zee J, Brunelli SM, Usvyat LA, Weiner DE, Maddux FW, et al. Dialysate potassium, serum potassium, mortality, and arrhythmia events in hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2017; 69(2):266–77.
Article7. Lopez-Gomez JM, Villaverde M, Jofre R, Rodriguez-Benitez P, Perez-Garcia R. Interdialytic weight gain as a marker of blood pressure, nutrition, and survival in hemodialysis patients. Kidney Int Suppl. 2005; (93):S63–8.8. Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, et al. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003; 64(1):254–62.
Article9. Akner G, Cederholm T. Treatment of protein-energy malnutrition in chronic nonmalignant disorders. Am J Clin Nutr. 2001; 74(1):6–24.
Article10. Becker MH. The health belief model and sick role behavior. Health Educ Monogr. 1974; 2(4):409–19.
Article11. Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behaviour change and its maintenance: interventions based on self-determination theory. Eur Health Psychol. 2008; 10(1):2–5.12. Cho YM, Sung KW. The association of compliance with sick role behavior with satisfaction of basic psychological needs among hemodialysis patients. Korean J Health Promot. 2012; 12(1):58–65.13. Song MR. The development and test of self-efficacy promotion program on self-care of hemodialysis patients. J Korean Acad Nurs. 2000; 30(4):1066–77.
Article14. Yun KS, Choi JY. Effects of dietary program based on self-efficacy theory on dietary adherence, physical indices and quality of life for hemodialysis patients. J Korean Acad Nurs. 2016; 46(4):598–609.
Article15. Griva K, Nandakumar M, Ng JH, Lam KF, McBain H, Newman SP. Hemodialysis Self-management Intervention Randomized Trial (HED-SMART): a practical low-intensity intervention to improve adherence and clinical markers in patients receiving hemodialysis. Am J Kidney Dis. 2018; 71(3):371–81.
Article16. Hayashi A, Yamaguchi S, Waki K, Fujiu K, Hanafusa N, Nishi T, et al. Testing the feasibility and usability of a novel smartphone-based self-management support system for dialysis patients: a pilot study. JMIR Res Protoc. 2017; 6(4):e63.
Article17. Lee J, Lee H. The effects of smart program for patients who underwent percutaneous coronary intervention (SP-PCI) on disease-related knowledge, health behavior, and quality of life: a non-randomized controlled trial. J Korean Acad Nurs. 2017; 47(6):756–69.
Article18. Kim MY, Kang YH, Jung DY, Lee GJ. Older adults’ smart phone use and access to health information. J Qual Res. 2013; 14(1):13–22.19. Choi YS. A study on the relationship between perceived social support, and compliance with Sick role behavior in elderly hemodialysis patients [dissertation]. Seoul, Korea: Hanyang University;2008.20. Jung YS. The relationships among basic psychological needs, sensation seeking, flow, and exercise addiction of leisure sports participants [dissertation]. Seoul, Korea: Sungkyunkwan University;2010.21. Kim JH, Kim MJ. The factors affecting quality of life of hemodialysis patients. Korean J Adult Nurs. 1995; 7(2):299–312.22. Hwang E, Choi BS, Oh KH, Kwon YJ, Kim GH. Management of chronic kidney disease-mineral and bone disorder: Korean working group recommendations. Kidney Res Clin Pract. 2015; 34(1):4–12.
Article23. Wong MM, McCullough KP, Bieber BA, Bommer J, Hecking M, Levin NW, et al. Interdialytic weight gain: trends, predictors, and associated outcomes in the International Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2017; 69(3):367–79.
Article24. Park JS, Lee HS, Lee SY, Im HB, Oh HS. Relationship between knowledge and adherence to self-management guidelines, and influencing factors of adherence for hemodialysis patients. Korean J Rehabil Nurs. 2011; 14(1):39–46.25. Silva MN, Markland D, Minderico CS, Vieira PN, Castro MM, Coutinho SR, et al. A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description. BMC Public Health. 2008; 8:234.
Article26. Song YB. The effect of application-based dietary self-management program on biochemical indicators, self-efficacy and quality of life in hemodialysis patients [dissertation]. Seoul, Korea: Kyung Hee University;2018.27. Chung S, Kahng KW, Hong TW, Lee CH, Kang CM, Park CH. Seasonal variation of interdialytic weight gain in Korean hemodialysis patients. Korean J Nephrol. 2003; 22(4):426–32.28. Kyung JB. The effects on interdialytic weight gain, self-efficacy and self-care behavior in hemodialysis patient by using mobile application for self-management [dissertation]. Seoul, Korea: Hanyang University;2016.29. Lee SJ, Park HS, Han JH, Kim HJ, Seo MW, Choi EA, et al. Effects of an individualized educational program on knowledge, compliance and physiologic parameters in non-compliant hemodialysis patients. J Korean Clin Nurs Res. 2009; 15(3):5–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development and Evaluation of a Self-management Mobile App for Adults with Osteoarthritis
- Comparison of the Effects of an App-based and Poster-based Self-managed Workplace Stretching Program on Musculoskeletal Symptoms of Workers in Small Manufacturing Businesses
- Family-based mobile application needs in childhood obesity management in South Korea: a qualitative study
- A Review of Mobile App-Based Psychosocial Intervention for Personal and Clinical Recovery for People With Psychosis
- Dietary Application for the Management of Patients with Hemodialysis: A Formative Development Study