Acute Crit Care.
2020 Feb;35(1):31-37. 10.4266/acc.2019.00731.
Outcomes of bedside peripherally inserted central catheter placement: a retrospective study at a single institution
- Affiliations
-
- 1Division of Vascular and Transplant Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Vascular and Transplant Surgery, Department of Nursing, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Vascular and Transplant Surgery, Department of Surgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- 4Division of Vascular and Transplant Surgery, Department of Surgery, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2500948
- DOI: http://doi.org/10.4266/acc.2019.00731
Abstract
- Background
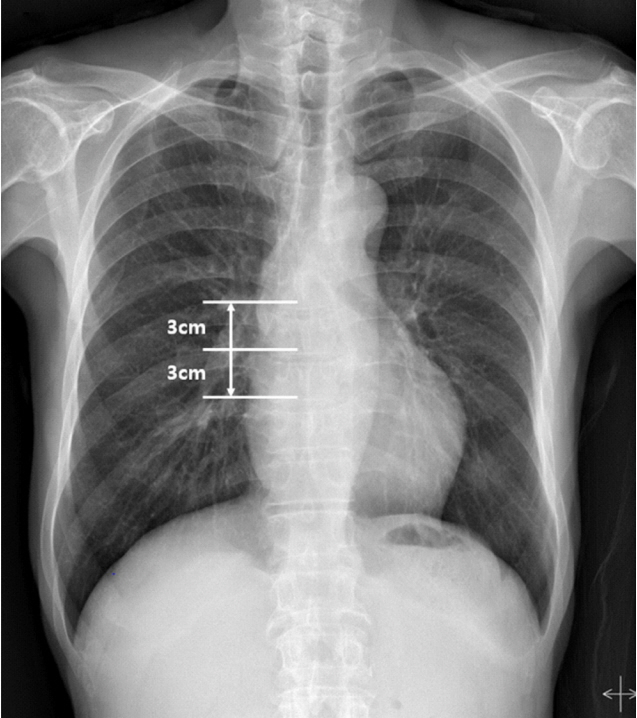
Bedside insertion of peripherally inserted central catheters (PICCs) has higher rates of malposition than fluoroscopic-guided PICC placement. This study evaluated the success rate of bedside PICC placement, variations in tip location, and risk factors for malposition. Methods: This retrospective study included patients who underwent bedside PICC placement from January 2013 to September 2014 in a single institution. The procedure was conducted under ultrasound guidance or by a blind method. After PICC placement, tip location was determined by chest X-ray. Results: The overall venous access success rate with bedside PICC placement was 98.1% (1,302/ 1,327). There was no significant difference in the venous access success rate between ultrasound-guided placement (868/880, 98.6%) and a blind approach placement (434/447, 97.1%). Optimal tip position was achieved on the first attempt in 1,192 cases (91.6%). Repositioning was attempted in 65 patients; 60 PICCs were repositioned at the bedside, two PICCs were repositioned under fluoroscopic guidance, and three PICCs moved to the desired position without intervention. Final optimal tip position after repositioning was achieved in 1,229 (94.4%). In logistic regression analysis, five factors associated with tip malposition included female sex (Exp(B), 1.687; 95% confidence interval [CI], 1.180 to 2.412; P=0.004), older age (Exp(B), 1.026; 95% CI, 1.012 to 1.039; P<0.001), cancer (Exp(B), 0.650; 95% CI, 0.455 to 0.929; P=0.018), lung disease (Exp(B), 2.416; 95% CI, 1.592 to 3.666; P<0.001), and previous catheter insertions (Exp(B), 1.262; 95% CI, 1.126 to 1.414; P<0.001). Conclusions: Bedside PICC placement without fluoroscopy is effective and safe in central venous catheters. Potential risk factors associated with catheter tip malposition include older age, female sex, cancer, pulmonary disease, and previous central vein catheterizations.
Figure
Cited by 1 articles
-
Catheter detection by transthoracic echocardiography during placement of peripherally inserted central catheters: a real-time method for eliminating misplacement
Yong Chae Jung, Man-shik Shim, Hee Sun Park, Min-Woong Kang
Acute Crit Care. 2024;39(2):266-274. doi: 10.4266/acc.2024.00150.
Reference
-
1. Parkinson R, Gandhi M, Harper J, Archibald C. Establishing an ultrasound guided peripherally inserted central catheter (PICC) insertion service. Clin Radiol. 1998; 53:33–6.
Article2. Botella-Carretero JI, Carrero C, Guerra E, Valbuena B, Arrieta F, Calañas A, et al. Role of peripherally inserted central catheters in home parenteral nutrition: a 5-year prospective study. JPEN J Parenter Enteral Nutr. 2013; 37:544–9.3. Spaziani S, Micheli T, Vincenzi B, Campisi C. Groshong PICC and home care: an opportunity: clinical experience after the first 200 implants. J Vasc Access. 2000; 1:108–11.
Article4. Todd J. Peripherally inserted central catheters and their use in i.v. therapy. Br J Nurs. 1999; 8:140–4.
Article5. Seckold T, Walker S, Dwyer T. A comparison of silicone and polyurethane PICC lines and postinsertion complication rates: a systematic review. J Vasc Access. 2015; 16:167–77.
Article6. Hoshal VL Jr. Total intravenous nutrition with peripherally inserted silicone elastomer central venous catheters. Arch Surg. 1975; 110:644–6.
Article7. Scrivens N, Sabri E, Bredeson C, McDiarmid S. Comparison of complication rates and incidences associated with different peripherally inserted central catheters (PICC) in patients with hematological malignancies: a retrospective cohort study. Leuk Lymphoma. 2020; 61:156–64.
Article8. Glauser F, Breault S, Rigamonti F, Sotiriadis C, Jouannic AM, Qanadli SD. Tip malposition of peripherally inserted central catheters: a prospective randomized controlled trial to compare bedside insertion to fluoroscopically guided placement. Eur Radiol. 2017; 27:2843–9.
Article9. Trerotola SO, Thompson S, Chittams J, Vierregger KS. Analysis of tip malposition and correction in peripherally inserted central catheters placed at bedside by a dedicated nursing team. J Vasc Interv Radiol. 2007; 18:513–8.
Article10. Racadio JM, Doellman DA, Johnson ND, Bean JA, Jacobs BR. Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics. 2001; 107:E28.
Article11. Petersen J, Delaney JH, Brakstad MT, Rowbotham RK, Bagley CM Jr. Silicone venous access devices positioned with their tips high in the superior vena cava are more likely to malfunction. Am J Surg. 1999; 178:38–41.
Article12. Luciani A, Clement O, Halimi P, Goudot D, Portier F, Bassot V, et al. Catheter-related upper extremity deep venous thrombosis in cancer patients: a prospective study based on Doppler US. Radiology. 2001; 220:655–60.
Article13. LaRue GD. Efficacy of ultrasonography in peripheral venous cannulation. J Intraven Nurs. 2000; 23:29–34.14. Mazzola JR, Schott-Baer D, Addy L. Clinical factors associated with the development of phlebitis after insertion of a peripherally inserted central catheter. J Intraven Nurs. 1999; 22:36–42.15. Jeon EY, Koh SH, Lee IJ, Ha HI, Park BJ. Useful equation for proper estimate of left side peripherally inserted central venous catheter length in relation to the height. J Vasc Access. 2015; 16:42–6.
Article16. Song L, Li X, Guo Y, Ye M, Ma Y, Guo M, et al. Malposition of peripherally inserted central catheter: experience from 3012 cancer patients. Int J Nurs Pract. 2014; 20:446–9.
Article17. Nakamuta S, Nishizawa T, Matsuhashi S, Shimizu A, Uraoka T, Yamamoto M. Real-time ultrasound-guided placement of peripherally inserted central venous catheter without fluoroscopy. J Vasc Access. 2018; 19:609–614.
Article18. Rasuli P, Hammond DI, Peterkin IR. Spontaneous intrajugular migration of long-term central venous access catheters. Radiology. 1992; 182:822–4.
Article19. Qiu XX, Guo Y, Fan HB, Shao J, Zhang XB. Incidence, risk factors and clinical outcomes of peripherally inserted central catheter spontaneous dislodgment in oncology patients: a prospective cohort study. Int J Nurs Stud. 2014; 51:955–63.
Article20. Muhm M, Sunder-Plassmann G, Apsner R, Pernerstorfer T, Rajek A, Lassnigg A, et al. Malposition of central venous catheters: incidence, management and preventive practices. Wien Klin Wochenschr. 1997; 109:400–5.21. Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular versus subclavian access: a systematic review. Crit Care Med. 2002; 30:454–60.22. Vesely TM. Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol. 2003; 14:527–34.
Article23. Weber E, Liberek T, Wołyniec W, Rutkowski B. Catheter tip malposition after percutaneous placement of tunneled hemodialysis catheters. Hemodial Int. 2015; 19:509–13.
Article24. Sharp R, Cummings M, Childs J, Fielder A, Mikocka-Walus A, Grech C, et al. Measurement of vein diameter for peripherally inserted central catheter (PICC) insertion: an observational study. J Infus Nurs. 2015; 38:351–7.25. Cho HH, Jeon EY, Lee HJ, Lee H, Koh SH, Choi SY, et al. A new formula to estimate the length of right upper extremity vein from elbow crease to carina calculated by peripherally inserted central catheter insertion through right basilic vein puncture. J Korean Soc Radiol. 2012; 66:229–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and Efficacy of Peripherally Inserted Central Catheter Placement by Surgical Intensivist–Led Vascular Access Team
- Peripherally inserted central catheter procedure at the bedside by a nephrologist is safe and successful
- Catheter detection by transthoracic echocardiography during placement of peripherally inserted central catheters: a real-time method for eliminating misplacement
- Bedside Ultrasound-Guided Peripherally Inserted Central Catheter Placement by Critical Care Fellows in Critically Ill Patients: A Feasibility and Safety Study
- Safety and feasibility of ultrasound-guided insertion of peripherally inserted central catheter performed by an intensive care trainee