Clin Endosc.
2020 Mar;53(2):213-220. 10.5946/ce.2019.068.
The Role of Endoscopic Ultrasound-Guided Ki67 in the Management of Non-Functioning Pancreatic Neuroendocrine Tumors
- Affiliations
-
- 1Department of Medicine, New York Presbyterian Columbia University Irving Medical Center, New York, NY, USA
- 2Division of Gastroenterology and Hepatology, Department of Medicine, New York University, New York, NY, USA
- 3Department of Pathology and Cell Biology, New York Presbyterian Columbia University Irving Medical Center, New York, NY, USA
- 4Division of Digestive and Liver Diseases, Department of Medicine, New York Presbyterian Columbia University Irving Medical Center, New York, NY, USA
- 5Department of Surgery, New York Presbyterian Columbia University Irving Medical Center, New York, NY, USA
- 6Department of Surgery, New York University Winthrop Hospital, Mineola, NY, USA
- KMID: 2500889
- DOI: http://doi.org/10.5946/ce.2019.068
Abstract
- Background/Aims
The management of small, incidentally discovered nonfunctioning pancreatic neuroendocrine tumors (NF-PNETs) has been a matter of debate. Endoscopic ultrasound with fine-needle aspiration (EUS-FNA) is a tool used to identify and risk-stratify PNETs. This study investigates the concordance rate of Ki67 grading between EUS-FNA and surgical pathology specimens in NFPNETs and whether certain NF-PNET characteristics are associated with disease recurrence and disease-related death.
Methods
We retrospectively reviewed the clinical history, imaging, endoscopic findings, and pathology records of 37 cases of NFPNETs that underwent pre-operative EUS-FNA and surgical resection at a single academic medical center.
Results
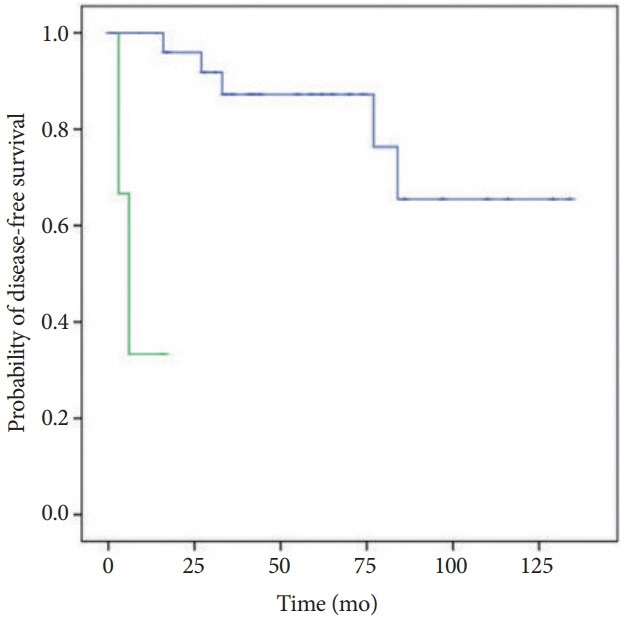
There was 73% concordance between Ki67 obtained from EUS-FNA cytology and surgical pathology specimens; concordance was the highest for low- and high-grade NF-PNETs. High-grade Ki67 NF-PNETs based on cytology (p=0.028) and histology (p=0.028) were associated with disease recurrence and disease-related death. Additionally, tumors with high-grade mitotic rate (p=0.005), tumor size >22.5 mm (p=0.104), and lymphovascular invasion (p=0.103) were more likely to have poor prognosis.
Conclusions
NF-PNETs with high-grade Ki67 on EUS-FNA have poor prognosis despite surgical resection. NF-PNETs with intermediate-grade Ki67 on EUS-FNA should be strongly considered for surgical resection. NF-PNETs with low-grade Ki67 on EUSFNA can be monitored without surgical intervention, up to tumor size 20 mm.
Keyword
Figure
Cited by 1 articles
-
Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clin Endosc. 2021;54(5):633-640. doi: 10.5946/ce.2021.216.
Reference
-
1. Halfdanarson TR, Rubin J, Farnell MB, Grant CS, Petersen GM. Pancreatic endocrine neoplasms: epidemiology and prognosis of pancreatic endocrine tumors. Endocr Relat Cancer. 2008; 15:409–427.
Article2. Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008; 135:1469–1492.
Article3. Grimelius L, Hultquist GT, Stenkvist B. Cytological differentiation of asymptomatic pancreatic islet cell tumours in autopsy material. Virchows Arch A Pathol Anat Histol. 1975; 365:275–288.4. Kimura W, Kuroda A, Morioka Y. Clinical pathology of endocrine tumors of the pancreas. Analysis of autopsy cases. Dig Dis Sci. 1991; 36:933–942.5. Halfdanarson TR, Rabe KG, Rubin J, Petersen GM. Pancreatic neuroendocrine tumors (PNETs): incidence, prognosis and recent trend toward improved survival. Ann Oncol. 2008; 19:1727–1733.
Article6. Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ. Changing incidence of pancreatic neoplasms: a 16-year review of statewide tumor registry. Pancreas. 2008; 37:134–138.7. Kuo EJ, Salem RR. Population-level analysis of pancreatic neuroendocrine tumors 2 cm or less in size. Ann Surg Oncol. 2013; 20:2815–2821.8. Hasegawa T, Yamao K, Hijioka S, et al. Evaluation of Ki-67 index in EUS-FNA specimens for the assessment of malignancy risk in pancreatic neuroendocrine tumors. Endoscopy. 2014; 46:32–38.
Article9. Gullo L, Migliori M, Falconi M, et al. Nonfunctioning pancreatic endocrine tumors: a multicenter clinical study. Am J Gastroenterol. 2003; 98:2435–2439.
Article10. Hill JS, McPhee JT, McDade TP, et al. Pancreatic neuroendocrine tumors: the impact of surgical resection on survival. Cancer. 2009; 115:741–751.11. Franko J, Feng W, Yip L, Genovese E, Moser AJ. Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. J Gastrointest Surg. 2010; 14:541–548.
Article12. Bettini R, Partelli S, Boninsegna L, et al. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery. 2011; 150:75–82.
Article13. Lee LC, Grant CS, Salomao DR, et al. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery. 2012; 152:965–974.
Article14. Kishi Y, Shimada K, Nara S, Esaki M, Hiraoka N, Kosuge T. Basing treatment strategy for non-functional pancreatic neuroendocrine tumors on tumor size. Ann Surg Oncol. 2014; 21:2882–2888.
Article15. Zhang IY, Zhao J, Fernandez-Del Castillo C, et al. Operative versus nonoperative management of nonfunctioning pancreatic neuroendocrine tumors. J Gastrointest Surg. 2016; 20:277–283.
Article16. Regenet N, Carrere N, Boulanger G, et al. Is the 2-cm size cutoff relevant for small nonfunctioning pancreatic neuroendocrine tumors: a French multicenter study. Surgery. 2016; 159:901–907.
Article17. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology neuroendocrine and adrenal tumors (United States) [Internet]. Plymouth Meeting (PA): NCCN; c2019 [updated 2019 Mar 5; cited 2019 Jul 7]. https://www.nccn.org/professionals/physician_gls/pdf/neuroendocrine.pdf.18. Falconi M, Eriksson B, Kaltsas G, et al. ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology. 2016; 103:153–171.
Article19. La Rosa S, Sessa F, Capella C, et al. Prognostic criteria in nonfunctioning pancreatic endocrine tumours. Virchows Arch. 1996; 429:323–333.
Article20. Bettini R, Boninsegna L, Mantovani W, et al. Prognostic factors at diagnosis and value of WHO classification in a mono-institutional series of 180 non-functioning pancreatic endocrine tumours. Ann Oncol. 2008; 19:903–908.
Article21. Alexiev BA, Darwin PE, Goloubeva O, Ioffe OB. Proliferative rate in endoscopic ultrasound fine-needle aspiration of pancreatic endocrine tumors: correlation with clinical behavior. Cancer. 2009; 117:40–45.22. Hamilton NA, Liu TC, Cavatiao A, et al. Ki-67 predicts disease recurrence and poor prognosis in pancreatic neuroendocrine neoplasms. Surgery. 2012; 152:107–113.
Article23. Unno J, Kanno A, Masamune A, et al. The usefulness of endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of pancreatic neuroendocrine tumors based on the World Health Organization classification. Scand J Gastroenterol. 2014; 49:1367–1374.
Article24. Cherenfant J, Talamonti MS, Hall CR, et al. Comparison of tumor markers for predicting outcomes after resection of nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2014; 156:1504–1510. discussion 1510-1511.
Article25. Díaz Del Arco C, Esteban López-Jamar JM, Ortega Medina L, Díaz Pérez JÁ, Fernández Aceñero MJ. Fine-needle aspiration biopsy of pancreatic neuroendocrine tumors: correlation between Ki-67 index in cytological samples and clinical behavior. Diagn Cytopathol. 2017; 45:29–35.
Article26. McLean AM, Fairclough PD. Endoscopic ultrasound in the localisation of pancreatic islet cell tumours. Best Pract Res Clin Endocrinol Metab. 2005; 19:177–193.
Article27. Fujimori N, Osoegawa T, Lee L, et al. Efficacy of endoscopic ultrasonography and endoscopic ultrasonography-guided fine-needle aspiration for the diagnosis and grading of pancreatic neuroendocrine tumors. Scand J Gastroenterol. 2016; 51:245–252.
Article28. Piani C, Franchi GM, Cappelletti C, et al. Cytological Ki-67 in pancreatic endocrine tumours: an opportunity for pre-operative grading. Endocr Relat Cancer. 2008; 15:175–181.
Article29. Larghi A, Capurso G, Carnuccio A, et al. Ki-67 grading of nonfunctioning pancreatic neuroendocrine tumors on histologic samples obtained by EUS-guided fine-needle tissue acquisition: a prospective study. Gastrointest Endosc. 2012; 76:570–577.
Article30. Carlinfante G, Baccarini P, Berretti D, et al. Ki-67 cytological index can distinguish well-differentiated from poorly differentiated pancreatic neuroendocrine tumors: a comparative cytohistological study of 53 cases. Virchows Arch. 2014; 465:49–55.
Article31. Farrell JM, Pang JC, Kim GE, Tabatabai ZL. Pancreatic neuroendocrine tumors: accurate grading with Ki-67 index on fine-needle aspiration specimens using the WHO 2010/ENETS criteria. Cancer Cytopathol. 2014; 122:770–778.
Article32. Weynand B, Borbath I, Bernard V, et al. Pancreatic neuroendocrine tumour grading on endoscopic ultrasound-guided fine needle aspiration: high reproducibility and inter-observer agreement of the Ki-67 labelling index. Cytopathology. 2014; 25:389–395.
Article33. Rebours V, Cordova J, Couvelard A, et al. Can pancreatic neuroendocrine tumour biopsy accurately determine pathological characteristics? Dig Liver Dis. 2015; 47:973–977.
Article34. Boutsen L, Jouret-Mourin A, Borbath I, van Maanen A, Weynand B. Accuracy of pancreatic neuroendocrine tumour grading by endoscopic ultrasound-guided fine needle aspiration: analysis of a large cohort and perspectives for improvement. Neuroendocrinology. 2018; 106:158–166.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of endoscopic ultrasound in the diagnosis and local ablative therapy of pancreatic neuroendocrine tumors
- Endoscopic Ultrasound-Guided Direct Intervention for Solid Pancreatic Tumors
- Therapy of Pancreatic Neuroendocrine Tumors: Fine Needle Intervention including Ethanol and Radiofrequency Ablation
- Diagnostic Role and Therapeutic Perspectives of Endoscopic Ultrasound for Pancreatic Neuroendocrine Tumor
- Endoscopic Ultrasound-Guided Drainage of Pancreatic Fluid Collections (with Video)