Anesth Pain Med.
2020 Jan;15(1):88-95. 10.17085/apm.2020.15.1.88.
Additional effect of magnesium sulfate and vitamin C in laparoscopic gynecologic surgery for postoperative pain management: a double-blind randomized controlled trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Busan Paik Hospital, Inje University College of Medicine, Korea
- 2Paik Institute for Clinical Research, Inje University College of Medicine, Busan, Korea
- KMID: 2500461
- DOI: http://doi.org/10.17085/apm.2020.15.1.88
Abstract
- Background
This clinical trial was conducted to determine whether combined use of magnesium sulfate and vitamin C more significantly reduced postoperative fentanyl consumption and pain than magnesium sulfate or vitamin C alone.
Methods
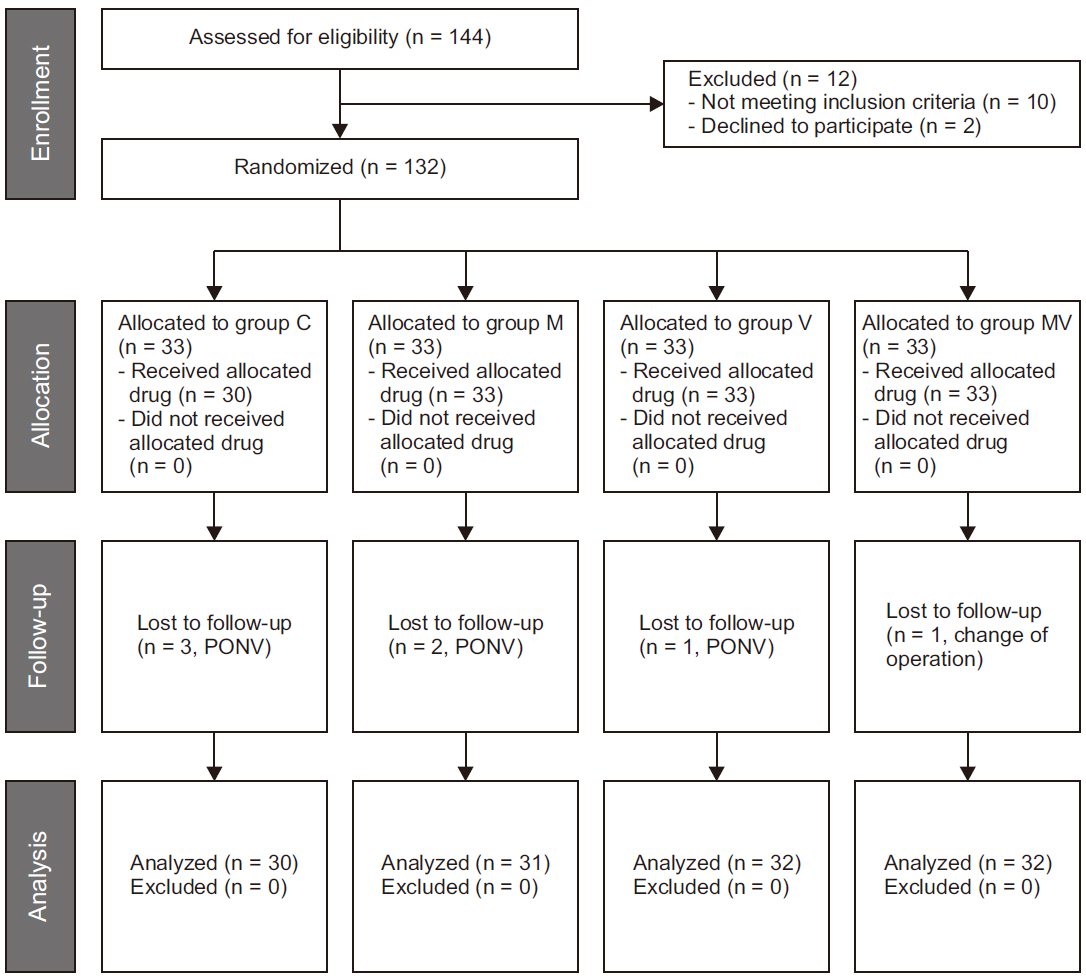
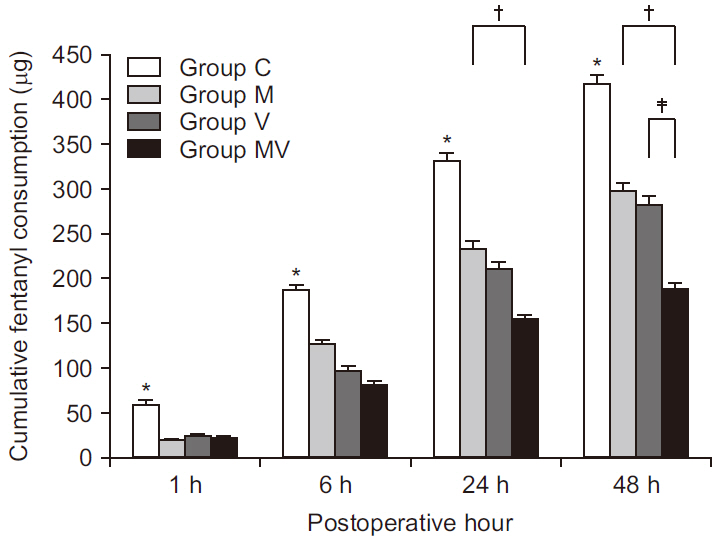
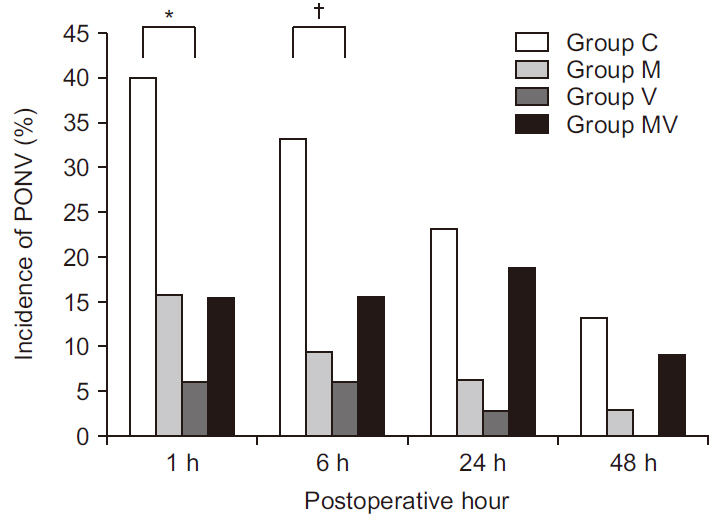
The prospective, double-blinded, randomized controlled study enrolled 132 patients scheduled for laparoscopic gynecologic surgery. The patients were randomly allocated to one of the four groups (n = 33 for each group; Group M [magnesium sulfate 40 mg/kg], Group V [vitamin C 50 mg/kg], Group MV [magnesium sulfate 40 mg/kg and vitamin C 50 mg/kg] and Group C [isotonic saline 40 ml]). Cumulative postoperative fentanyl consumption (primary endpoint measure), postoperative pain score by numeric rating scale, and postoperative nausea and vomiting were recorded at 1, 6, 24, and 48 h after discharge from the postanesthesia care unit.
Results
Cumulative postoperative fentanyl consumption was significantly less in Groups M, V, and MV than in Group C at all time points. Group MV showed significantly less cumulative postoperative fentanyl consumption than Group M at postoperative 24 h (mean ± standard deviation, 156.6 ± 67.5 vs. 235.6 ± 94.6 μg, P = 0.001), as well as significantly less consumption than Groups M and V at postoperative 48 h (190.8 ± 74.6 vs. 301.0 ± 114.8 or 284.1 ± 128.6 μg, P < 0.001, P = 0.003, respectively).
Conclusions
Combined use of magnesium sulfate and vitamin C provides an additional benefit in postoperative pain management after laparoscopic gynecologic surgery in comparison to single administration of magnesium sulfate or vitamin C.
Keyword
Figure
Cited by 1 articles
-
Effect of intravenous magnesium on postoperative pain control for major abdominal surgery: a randomized double-blinded study
Arash Peivandi Yazdi, Mehrdad Esmaeeli, Mehryar Taghavi Gilani
Anesth Pain Med. 2022;17(3):280-285. doi: 10.17085/apm.22156.
Reference
-
Lovich-Sapola J., Smith CE., Brandt CP. 2015. Postoperative pain control. Surg Clin North Am. 95:301–18. DOI: 10.1016/j.suc.2014.10.002. PMID: 25814108.Khan RS., Ahmed K., Blakeway E., Skapinakis P., Nihoyannopoulos L., Macleod K, et al. 2011. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 201:122–31. DOI: 10.1016/j.amjsurg.2010.02.007. PMID: 20832052.Gammaitoni AR., Fine P., Alvarez N., McPherson ML., Bergmark S. 2003. Clinical application of opioid equianalgesic data. Clin J Pain. 19:286–97. DOI: 10.1097/00002508-200309000-00002. PMID: 12966254.Schwenk ES., Mariano ER. 2018. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol. 71:345–52. DOI: 10.4097/kja.d.18.00217. PMID: 30139215. PMCID: PMC6193589.Albrecht E., Kirkham KR., Liu SS., Brull R. 2013. Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia. 68:79–90. DOI: 10.1111/j.1365-2044.2012.07335.x. PMID: 23121612.Herroeder S., Schönherr ME., De Hert SG SG., Hollmann MW. 2011. Magnesium--essentials for anesthesiologists. Anesthesiology. 114:971–93. DOI: 10.1097/ALN.0b013e318210483d. PMID: 21364460.Rebec GV., Pierce RC. 1994. A vitamin as neuromodulator: ascorbate release into the extracellular fluid of the brain regulates dopaminergic and glutamatergic transmission. Prog Neurobiol. 43:537–65. DOI: 10.1016/0301-0082(94)90052-3. PMID: 7816935.Fukushima R., Yamazaki E. 2010. Vitamin C requirement in surgical patients. Curr Opin Clin Nutr Metab Care. 13:669–76. DOI: 10.1097/MCO.0b013e32833e05bc. PMID: 20689415.Carr AC., McCall C. 2017. The role of vitamin C in the treatment of pain: new insights. J Transl Med. 15:77. DOI: 10.1186/s12967-017-1179-7. PMID: 28410599. PMCID: PMC5391567.Sousa AM., Rosado GM., Neto Jde S S., Guimarães GM., Ashmawi HA. 2016. Magnesium sulfate improves postoperative analgesia in laparoscopic gynecologic surgeries: a double-blind randomized controlled trial. J Clin Anesth. 34:379–84. DOI: 10.1016/j.jclinane.2016.05.006. PMID: 27687417.Koltka K., Koknel-Talu G., Asik M., Ozyalcin S. 2011. Comparison of efficacy of intraarticular application of magnesium, levobupivacaine and lornoxicam with placebo in arthroscopic surgery. Knee Surg Sports Traumatol Arthrosc. 19:1884–9. DOI: 10.1007/s00167-011-1497-x. PMID: 21468614.Bolcal C., Iyem H., Sargin M., Mataraci I., Yildirim V., Doganci S, et al. 2005. Comparison of magnesium sulfate with opioid and NSAIDs on postoperative pain management after coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 19:714–8. DOI: 10.1053/j.jvca.2005.08.010. PMID: 16326293.Chen S., Roffey DM., Dion CA., Arab A., Wai EK. 2016. Effect of perioperative vitamin C supplementation on postoperative pain and the incidence of chronic regional pain syndrome: a systematic review and meta-analysis. Clin J Pain. 32:179–85. DOI: 10.1097/AJP.0000000000000218. PMID: 25654537.Seyhan TO., Tugrul M., Sungur MO., Kayacan S., Telci L., Pembeci K, et al. 2006. Effects of three different dose regimens of magnesium on propofol requirements, haemodynamic variables and postoperative pain relief in gynaecological surgery. Br J Anaesth. 96:247–52. DOI: 10.1093/bja/aei291. PMID: 16311277.Jeon Y., Park JS., Moon S., Yeo J. 2016. Effect of intravenous high dose vitamin C on postoperative pain and morphine use after laparoscopic colectomy: a randomized controlled trial. Pain Res Manag. 2016:9147279. DOI: 10.1155/2016/9147279. PMID: 27872555. PMCID: PMC5107231.Turner JA., Turk DC. 2008. The significance of clinical significance. Pain. 137:467–8. DOI: 10.1016/j.pain.2008.03.029. PMID: 18455313.McCarthy RJ., Kroin JS., Tuman KJ., Penn RD., Ivankovich AD. 1998. Antinociceptive potentiation and attenuation of tolerance by intrathecal co-infusion of magnesium sulfate and morphine in rats. Anesth Analg. 86:830–6. DOI: 10.1213/00000539-199804000-00028. PMID: 9539610.Ma H., Tang J., White PF., Zaentz A., Wender RH., Sloninsky A, et al. 2004. Perioperative rofecoxib improves early recovery after outpatient herniorrhaphy. Anesth Analg. 98:970–5. DOI: 10.1213/01.ANE.0000111110.94186.55. PMID: 15041582.Kim HK., Park SK., Zhou JL., Taglialatela G., Chung K., Coggeshall RE, et al. 2004. Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain. 111:116–24. DOI: 10.1016/j.pain.2004.06.008. PMID: 15327815.Mikirova N., Casciari J., Rogers A., Taylor P. 2012. Effect of high-dose intravenous vitamin C on inflammation in cancer patients. J Transl Med. 10:189. DOI: 10.1186/1479-5876-10-189. PMID: 22963460. PMCID: PMC3480897.Rosa KA., Gadotti VM., Rosa AO., Rodrigues AL., Calixto JB., Santos AR. 2005. Evidence for the involvement of glutamatergic system in the antinociceptive effect of ascorbic acid. Neurosci Lett. 381:185–8. DOI: 10.1016/j.neulet.2005.02.032. PMID: 15882814.Harrison FE., May JM. 2009. Vitamin C function in the brain: vital role of the ascorbate transporter SVCT2. Free Radic Biol Med. 46:719–30. DOI: 10.1016/j.freeradbiomed.2008.12.018. PMID: 19162177. PMCID: PMC2649700.Kanazi GE., El-Khatib MF., Yazbeck-Karam VG., Hanna JE., Masri B., Aouad MT. 2012. Effect of vitamin C on morphine use after laparoscopic cholecystectomy: a randomized controlled trial. Can J Anaesth. 59:538–43. DOI: 10.1007/s12630-012-9692-x. PMID: 22402954.Ayatollahi V., Dehghanpour Farashah S S., Behdad S., Vaziribozorg S., Rabbani Anari M M. 2017. Effect of intravenous vitamin C on postoperative pain in uvulopalatopharyngoplasty with tonsillectomy. Clin Otolaryngol. 42:139–43. DOI: 10.1111/coa.12684. PMID: 27219124.Levine M., Conry-Cantilena C., Wang Y., Welch RW., Washko PW., Dhariwal KR, et al. 1996. Vitamin C pharmacokinetics in healthy volunteers: evidence for a recommended dietary allowance. Proc Natl Acad Sci U S A. 93:3704–9. DOI: 10.1073/pnas.93.8.3704. PMID: 8623000. PMCID: PMC39676.Graumlich JF., Ludden TM., Conry-Cantilena C., Cantilena LR Jr., Wang Y., Levine M. 1997. Pharmacokinetic model of ascorbic acid in healthy male volunteers during depletion and repletion. Pharm Res. 14:1133–9. DOI: 10.1023/A:1012186203165. PMID: 9327438.Fritz H., Flower G., Weeks L., Cooley K., Callachan M., McGowan J, et al. 2014. Intravenous vitamin C and cancer: a systematic review. Integr Cancer Ther. 13:280–300. DOI: 10.1177/1534735414534463. PMID: 24867961.Khezri MB., Yaghobi S., Hajikhani M., Asefzadeh S. 2012. Comparison of postoperative analgesic effect of intrathecal magnesium and fentanyl added to bupivacaine in patients undergoing lower limb orthopedic surgery. Acta Anaesthesiol Taiwan. 50:19–24. DOI: 10.1016/j.aat.2012.03.001. PMID: 22500909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The impact of magnesium sulfate as adjuvant to intrathecal bupivacaine on intra-operative surgeon satisfaction and postoperative analgesia during laparoscopic gynecological surgery: randomized clinical study
- Effect of intravenous magnesium on postoperative pain control for major abdominal surgery: a randomized double-blinded study
- Additional low-pressure pulmonary recruitment for reducing post-laparoscopic shoulder pain in gynecologic laparoscopy: a randomized controlled trial
- Preemptive Analgesic Effect of Magnesium Sulfate on Postoperative Pain in Patients Undergoing Gastrectomy
- Preemptive Analgesic Effect of Magnesium Sulfate on Postoperative Pain after Hysterectomy