Cancer Res Treat.
2020 Apr;52(2):426-437. 10.4143/crt.2018.382.
Outcomes of Pregnancy after Breast Cancer in Korean Women:A Large Cohort Study
- Affiliations
-
- 1Center for Breast Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- 2Division of Breast and Thyroid, Department of Surgery, Keimyung University School of Medicine, Daegu, Korea
- 3Cancer Survivorship Branch, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 4Health Insurance Policy Research Institute, National Health Insurance Service, Wonju, Korea
- 5Department of Laboratory Medicine, Center for Diagnostic Oncology, National Cancer Center, Goyang, Korea
- 6Graduate School of Cancer Science and Policy, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- KMID: 2500328
- DOI: http://doi.org/10.4143/crt.2018.382
Abstract
- Purpose
The purpose of this study was to determine the rate and outcomes of pregnancies subsequent to breast cancer in Korea, and the effect of such pregnancies on the prognosis of women who survived breast cancer and subsequently conceived.
Materials and Methods
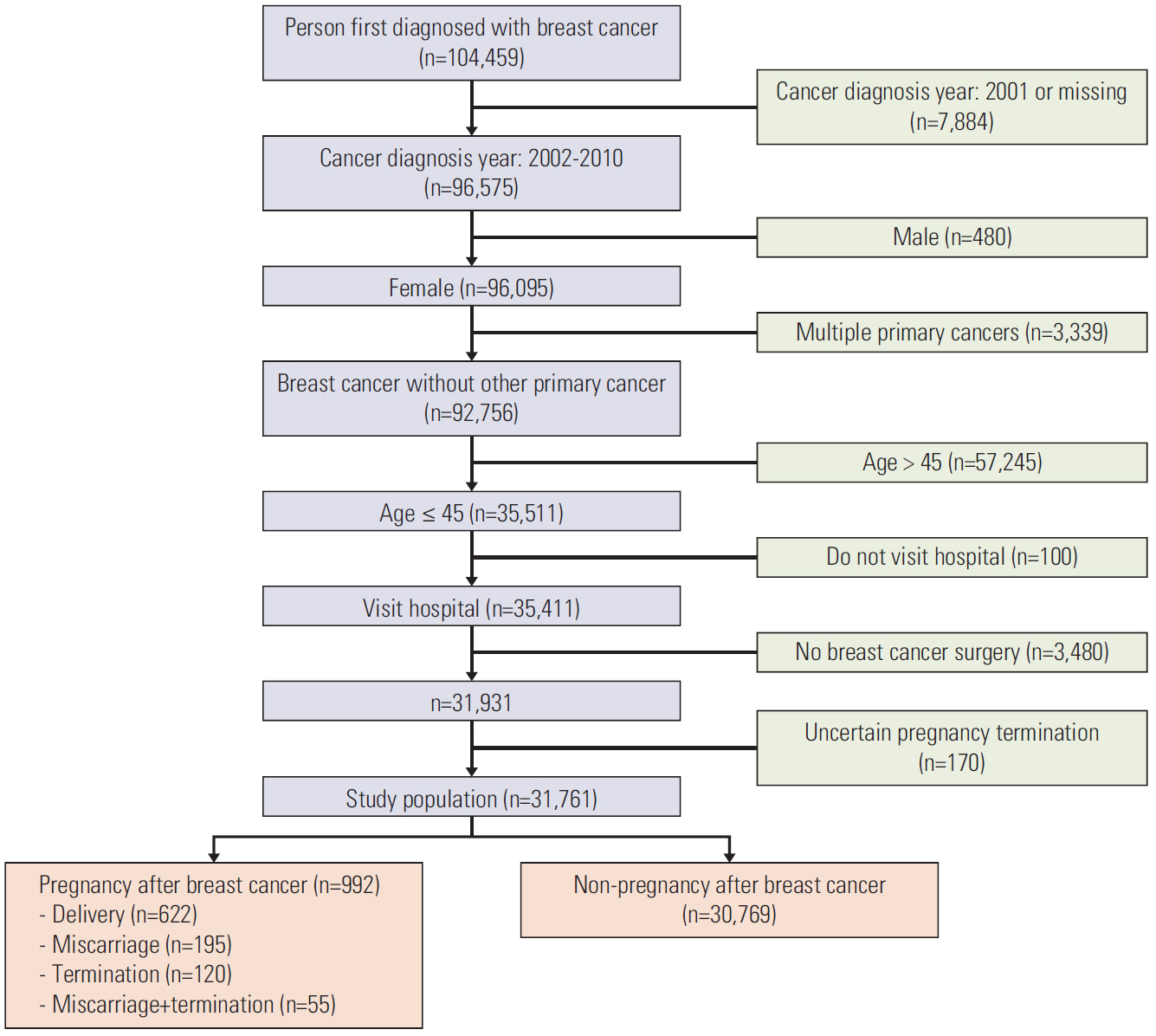
We followed a total of 31,761 Korean women 45 years of age or younger who were treated for primary breast cancer from 2002 to 2010. We also included follow-up surveys that were conducted through December 2011. We identified recurrence and mortality from breast cancer using data linked to the Korea National Health Insurance database. We used propensity score matching of the study cohort to analyze the risks of recurrence and mortality from breast cancer depending on pregnancy.
Results
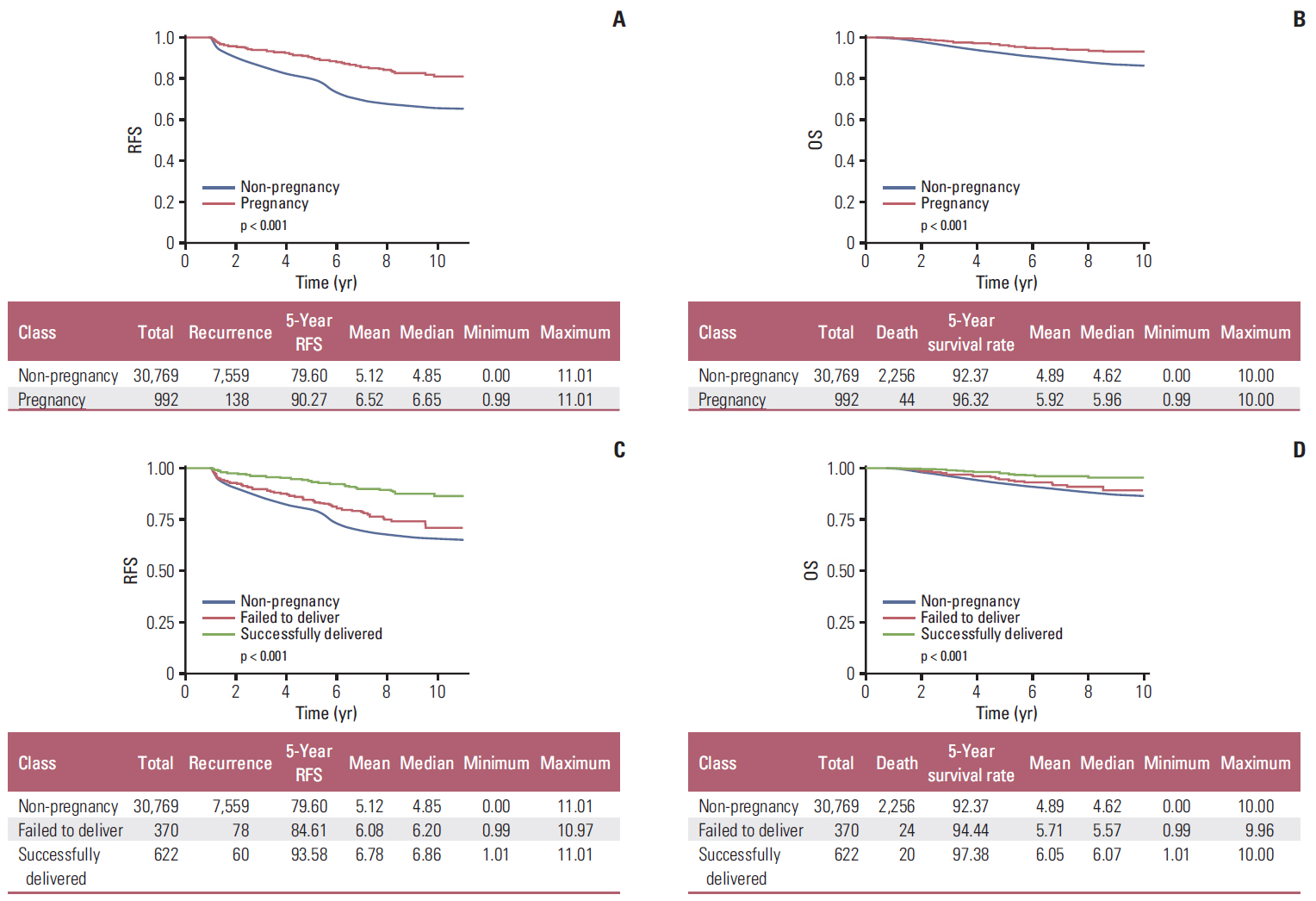
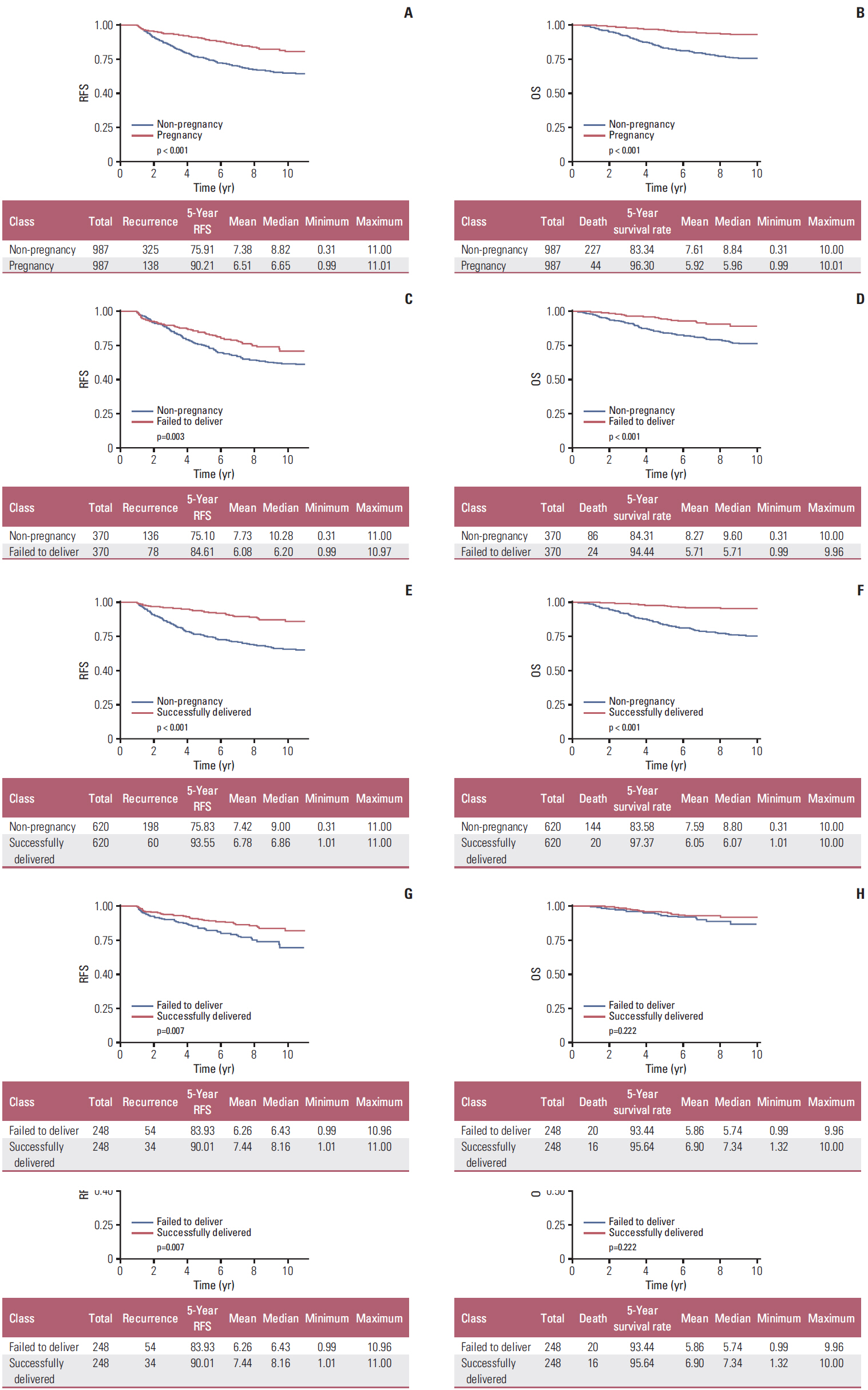
Within our sample, 992 women (3.1%) became pregnant after receiving treatment for breast cancer. Of those, 622 (67.5%) successfully delivered; the remaining 370 (32.5%) failed to deliver. After propensity score matching, we found that the women who became pregnant after breast cancer did not have a different risk of recurrence (hazard ratio [HR], 0.503; 95% confidence interval [CI], 0.434 to 0.584) and death (HR, 0.520; 95% CI, 0.397 to 0.681), compared with those who did not conceive after breast cancer treatment.
Conclusion
Our study is the first to report outcomes for Korean women who survived breast cancer and subsequently conceived. Women who survived breast cancer and subsequently became pregnant did not show a poorer survival outcome, compared with those who did not become pregnant.
Keyword
Figure
Reference
-
References
1. Partridge AH, Hughes ME, Warner ET, Ottesen RA, Wong YN, Edge SB, et al. Subtype-dependent relationship between young age at diagnosis and breast cancer survival. J Clin Oncol. 2016; 34:3308–14.
Article2. Chung M, Chang HR, Bland KI, Wanebo HJ. Younger women with breast carcinoma have a poorer prognosis than older women. Cancer. 1996; 77:97–103.
Article3. Winchester DP. Breast cancer in young women. Surg Clin North Am. 1996; 76:279–87.
Article4. Han W, Kim SW, Park IA, Kang D, Kim SW, Youn YK, et al. Young age: an independent risk factor for disease-free survival in women with operable breast cancer. BMC Cancer. 2004; 4:82.
Article5. Kataoka A, Tokunaga E, Masuda N, Shien T, Kawabata K, Miyashita M. Clinicopathological features of young patients (< 35 years of age) with breast cancer in a Japanese Breast Cancer Society supported study. Breast Cancer. 2014; 21:643–50.6. Schover LR, Rybicki LA, Martin BA, Bringelsen KA. Having children after cancer. A pilot survey of survivors' attitudes and experiences. Cancer. 1999; 86:697–709.7. Partridge AH, Ruddy KJ. Fertility and adjuvant treatment in young women with breast cancer. Breast. 2007; 16 Suppl 2:S175–81.
Article8. Ives A, Saunders C, Bulsara M, Semmens J. Pregnancy after breast cancer: population based study. BMJ. 2007; 334:194.
Article9. Kranick JA, Schaefer C, Rowell S, Desai M, Petrek JA, Hiatt RA, et al. Is pregnancy after breast cancer safe? Breast J. 2010; 16:404–11.
Article10. Sankila R, Heinavaara S, Hakulinen T. Survival of breast cancer patients after subsequent term pregnancy: "healthy mother effect". Am J Obstet Gynecol. 1994; 170:818–23.
Article11. von Schoultz E, Johansson H, Wilking N, Rutqvist LE. Influence of prior and subsequent pregnancy on breast cancer prognosis. J Clin Oncol. 1995; 13:430–4.
Article12. Lethaby AE, O'Neill MA, Mason BH, Holdaway IM, Harvey VJ. Overall survival from breast cancer in women pregnant or lactating at or after diagnosis. Auckland Breast Cancer Study Group. Int J Cancer. 1996; 67:751–5.13. Malamos NA, Stathopoulos GP, Keramopoulos A, Papadiamantis J, Vassilaros S. Pregnancy and offspring after the appearance of breast cancer. Oncology. 1996; 53:471–5.
Article14. Kroman N, Jensen MB, Melbye M, Wohlfahrt J, Mouridsen HT. Should women be advised against pregnancy after breast-cancer treatment? Lancet. 1997; 350:319–22.
Article15. Mueller BA, Simon MS, Deapen D, Kamineni A, Malone KE, Daling JR. Childbearing and survival after breast carcinoma in young women. Cancer. 2003; 98:1131–40.
Article16. Blakely LJ, Buzdar AU, Lozada JA, Shullaih SA, Hoy E, Smith TL, et al. Effects of pregnancy after treatment for breast carcinoma on survival and risk of recurrence. Cancer. 2004; 100:465–9.
Article17. Kroman N, Jensen MB, Wohlfahrt J, Ejlertsen B; Danish Breast Cancer Cooperative Group. Pregnancy after treatment of breast cancer: a population-based study on behalf of Danish Breast Cancer Cooperative Group. Acta Oncol. 2008; 47:545–9.18. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 2005; 37:325–31.
Article19. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–41.
Article20. Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 2005; 293:194–202.
Article21. Jee SH, Suh I, Kim IS, Appel LJ. Smoking and atherosclerotic cardiovascular disease in men with low levels of serum cholesterol: the Korea Medical Insurance Corporation Study. JAMA. 1999; 282:2149–55.22. Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Bodymass index and mortality in Korean men and women. N Engl J Med. 2006; 355:779–87.
Article23. Park SM, Lim MK, Jung KW, Shin SA, Yoo KY, Yun YH, et al. Prediagnosis smoking, obesity, insulin resistance, and second primary cancer risk in male cancer survivors: National Health Insurance Corporation Study. J Clin Oncol. 2007; 25:4835–43.24. Park SM, Yun YH, Kim YA, Jo M, Won YJ, Back JH, et al. Prediagnosis body mass index and risk of secondary primary cancer in male cancer survivors: a large cohort study. J Clin Oncol. 2016; 34:4116–24.
Article25. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article26. Pearce N. Analysis of matched case-control studies. BMJ. 2016; 352:i969.
Article27. Peccatori FA, Azim HA Jr, Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V, et al. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013; 24 Suppl 6:vi160–70.
Article28. Stensheim H, Cvancarova M, Moller B, Fossa SD. Pregnancy after adolescent and adult cancer: a population-based matched cohort study. Int J Cancer. 2011; 129:1225–36.
Article29. Luo M, Zeng J, Li F, He L, Li T. Safety of pregnancy after surgical treatment for breast cancer: a meta-analysis. Int J Gynecol Cancer. 2014; 24:1366–72.
Article30. Iqbal J, Amir E, Rochon PA, Giannakeas V, Sun P, Narod SA. Association of the timing of pregnancy with survival in women with breast cancer. JAMA Oncol. 2017; 3:659–65.
Article