J Korean Med Sci.
2020 Apr;35(17):e120. 10.3346/jkms.2020.35.e120.
Fecal Calprotectin as a Useful Non-Invasive Screening Marker for Eosinophilic Gastrointestinal Disorder in Korean Children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2500211
- DOI: http://doi.org/10.3346/jkms.2020.35.e120
Abstract
- Background
Eosinophilic gastrointestinal disorder (EoGID) is an emerging disease condition in Korean children, but its diagnosis requires invasive endoscopic biopsies. Fecal calprotectin (FCal) is a noninvasive biomarker for intestinal inflammation to differentiate organic gastrointestinal diseases from functional abdominal pain disorder. This study aimed to evaluate the diagnostic accuracy of FCal and to determine the optimal cutoff to differentiate EoGID from functional abdominal pain disorder.
Methods
A total of 253 children (122 boys, 131 girls; mean age 12.2 ± 3.6, range 2.9–17.8 years) who underwent endoscopy with biopsies for chronic gastrointestinal symptoms were recruited, except for 38 children diagnosed with inflammatory bowel disease, and divided into EoGID (n = 67) and functional abdominal pain disorder (n = 186). FCal, white blood cell (WBC) counts, eosinophil counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were measured in all subjects at initial diagnosis.
Results
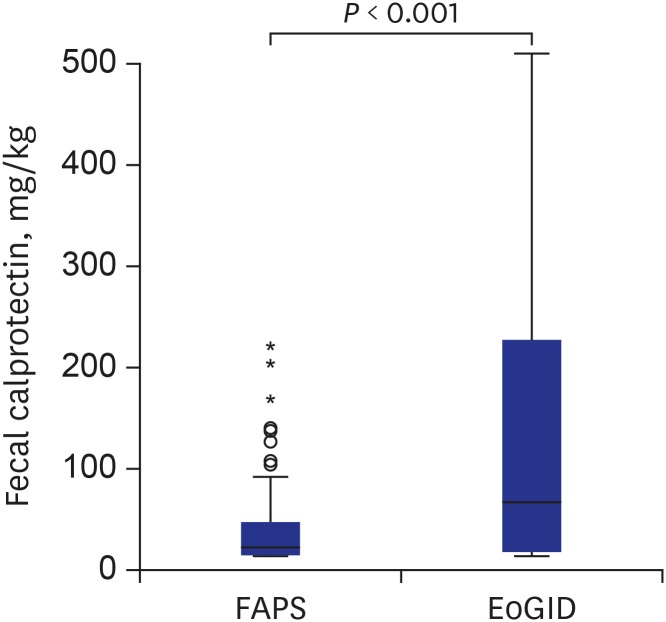
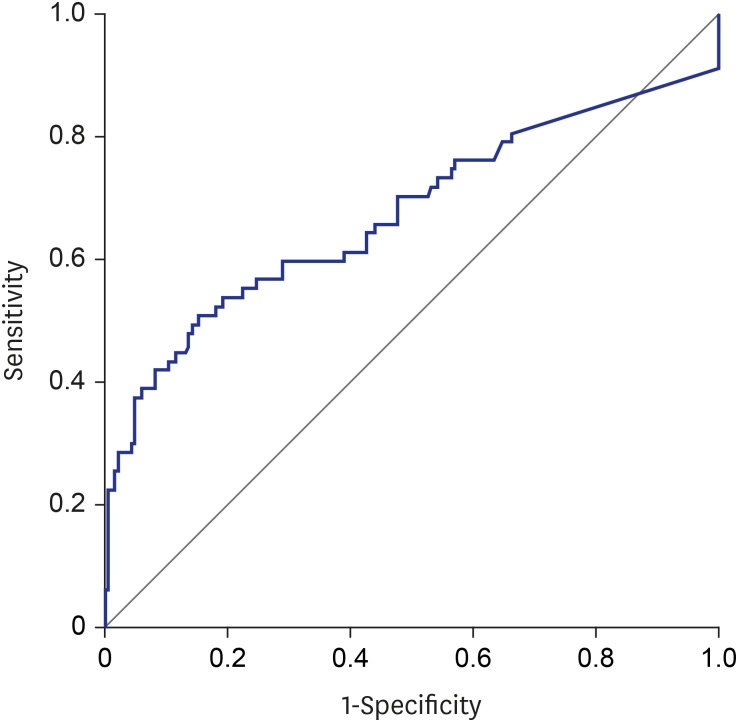
FCal levels weakly correlated with WBC (r = 0.127, P = 0.044) and CRP (r = 0.126, P = 0.040) but not with ESR and eosinophil count. FCal levels were significantly higher in the EoGID group than in the functional abdominal pain disorder group (mean 179.5 ± 242.9 mg/kg vs. 44.3 ± 68.1 mg/kg; P < 0.001), while WBC, ESR, CRP, and eosinophil count did not differ between the two groups (all P > 0.05). An optimal cutoff of FCal 73.2 mg/kg distinguished EoGID from functional abdominal pain disorder with a sensitivity of 50.7% and a specificity of 84.6%.
Conclusion
FCal is a useful and reliable noninvasive marker for differentiating EoGID from functional abdominal pain disorder in Korean children with chronic gastrointestinal symptoms when optimal cutoffs are applied.
Figure
Cited by 1 articles
-
Potential Utility of Fecal Calprotectin in Discriminating Colorectal Polyps From Other Major Etiologies in Children Presenting With Isolated Hematochezia
Yu Bin Kim, Ju Young Kim, Sujin Choi, Hyun Jin Kim, Yoo Min Lee, Yoon Lee, Hyo-Jeong Jang, Eun Hye Lee, Kyung Jae Lee, Soon Chul Kim, So Yoon Choi, Yunkoo Kang, Dae Yong Yi, You Jin Choi, Byung-Ho Choe, Ben Kang
J Korean Med Sci. 2022;37(9):e72. doi: 10.3346/jkms.2022.37.e72.
Reference
-
1. Hogan SP, Rothenberg ME. Review article: the eosinophil as a therapeutic target in gastrointestinal disease. Aliment Pharmacol Ther. 2004; 20(11-12):1231–1240. PMID: 15606385.
Article2. Ko HM, Morotti RA, Yershov O, Chehade M. Eosinophilic gastritis in children: clinicopathological correlation, disease course, and response to therapy. Am J Gastroenterol. 2014; 109(8):1277–1285. PMID: 24957155.
Article3. Spergel JM, Book WM, Mays E, Song L, Shah SS, Talley NJ, et al. Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States. J Pediatr Gastroenterol Nutr. 2011; 52(3):300–306. PMID: 21057327.
Article4. Uppal V, Kreiger P, Kutsch E. Eosinophilic gastroenteritis and colitis: a comprehensive review. Clin Rev Allergy Immunol. 2016; 50(2):175–188. PMID: 26054822.
Article5. Jensen ET, Martin CF, Kappelman MD, Dellon ES. Prevalence of eosinophilic gastritis, gastroenteritis, and colitis: estimates from a national administrative database. J Pediatr Gastroenterol Nutr. 2016; 62(1):36–42. PMID: 25988554.6. Kinoshita Y, Ishimura N, Oshima N, Ishihara S. Systematic review: eosinophilic esophagitis in Asian countries. World J Gastroenterol. 2015; 21(27):8433–8440. PMID: 26217096.
Article7. Choi BS, Hong SJ, Park SH, Kim HM, Choe BH. Differences in features and course of mucosal type eosinophilic gastroenteritis between Korean infants and children. J Korean Med Sci. 2015; 30(8):1129–1135. PMID: 26240491.
Article8. Kwon JY, Huh JS, Je BK, Hong KD, Lee JH. Eosinophilic gastrointestinal disorder presenting as intractable vomiting and ascites in a young girl. Pediatr Gastroenterol Hepatol Nutr. 2017; 20(3):198–203. PMID: 29026737.
Article9. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004; 113(1):11–28. PMID: 14713902.
Article10. Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker of intestinal inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12(6):524–534. PMID: 16775498.
Article11. Montalto M, Gallo A, Santoro L, D'Onofrio F, Landolfi R, Gasbarrini A. Role of fecal calprotectin in gastrointestinal disorders. Eur Rev Med Pharmacol Sci. 2013; 17(12):1569–1582. PMID: 23832721.12. Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006; 55(3):426–431. PMID: 16474109.
Article13. Olafsdottir I, Nemeth A, Lörinc E, Toth E, Agardh D. Value of fecal calprotectin as a biomarker for juvenile polyps in children investigated with colonoscopy. J Pediatr Gastroenterol Nutr. 2016; 62(1):43–46. PMID: 26147630.
Article14. Mahjoub FE, Zahedi N, Ashjai B, Ashtiani MT, Farahmand F, Monajemzadeh M, et al. Role of fecal calprotectin in differentiating between Hirschsprung's disease and functional constipation. Korean J Gastroenterol. 2013; 62(5):288–291. PMID: 24262594.
Article15. Degraeuwe PL, Beld MP, Ashorn M, Canani RB, Day AS, Diamanti A, et al. Faecal calprotectin in suspected paediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2015; 60(3):339–346. PMID: 25373864.
Article16. Trillo Belizón C, Ortega Páez E, Medina Claros AF, Rodríguez Sánchez I, Reina González A, Vera Medialdea R, et al. Faecal calprotectin as an aid to the diagnosis of non-IgE mediated cow's milk protein allergy. An Pediatr (Barc). 2016; 84(6):318–323. PMID: 26342278.
Article17. Biskou O, Gardner-Medwin J, Mackinder M, Bertz M, Clark C, Svolos V, et al. Faecal calprotectin in treated and untreated children with coeliac disease and juvenile idiopathic arthritis. J Pediatr Gastroenterol Nutr. 2016; 63(5):e112–e115. PMID: 27540707.
Article18. Olafsdottir I, Nemeth A, Lörinc E, Toth E, Agardh D. Value of fecal calprotectin as a biomarker for juvenile polyps in children investigated with colonoscopy. J Pediatr Gastroenterol Nutr. 2016; 62(1):43–46. PMID: 26147630.
Article19. Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional disorders: children and Adolescents. Gastroenterology. 2016; 150:1456–1468.20. Alhmoud T, Hanson JA, Parasher G. Eosinophilic gastroenteritis: an underdiagnosed condition. Dig Dis Sci. 2016; 61(9):2585–2592. PMID: 27234270.
Article21. Uppal V, Kreiger P, Kutsch E. Eosinophilic gastroenteritis and colitis: a comprehensive review. Clin Rev Allergy Immunol. 2016; 50(2):175–188. PMID: 26054822.
Article22. Chen MJ, Chu CH, Lin SC, Shih SC, Wang TE. Eosinophilic gastroenteritis: clinical experience with 15 patients. World J Gastroenterol. 2003; 9(12):2813–2816. PMID: 14669340.
Article23. Lee EH, Yang HR, Lee HS. Quantitative analysis of distribution of the gastrointestinal tract eosinophils in childhood functional abdominal pain disorders. J Neurogastroenterol Motil. 2018; 24(4):614–627. PMID: 30180307.
Article24. Spergel JM, Shuker M. Nutritional management of eosinophilic esophagitis. Gastrointest Endosc Clin N Am. 2008; 18(1):179–194. PMID: 18061111.
Article25. Shaheen NJ, Mukkada V, Eichinger CS, Schofield H, Todorova L, Falk GW. Natural history of eosinophilic esophagitis: a systematic review of epidemiology and disease course. Dis Esophagus. 2018; 31(8):doy015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update on eosinophilic gastrointestinal disease beyond eosinophilic esophagitis in children
- Fecal Calprotectin in Inflammatory Bowel Disease
- Clinical Utility of Fecal Neutrophil Gelatinase-Associated Lipocalin and Calprotectin as Biomarkers of Clostridioides (Clostridium) difficile Infection
- Usefulness of fecal immunochemical test and fecal calprotectin for detection of active ulcerative colitis
- Fecal immunochemical test as a biomarker for inflammatory bowel diseases: can it rival fecal calprotectin?