Brain Tumor Res Treat.
2020 Apr;8(1):1-10. 10.14791/btrt.2020.8.e5.
A National Consensus Survey for Current Practicein Brain Tumor Management I: Antiepileptic Drug andSteroid Usage
- Affiliations
-
- 1Department of Neurosurgery, Gyeongsang National University Changwon Hospital, Gyeongsang National University School of Medicine, Changwon, Korea
- 2Department of Neurology, Rare Disease Center, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, International St. Mary’s Hospital, Catholic Kwandong University, Incheon, Korea
- 4Department of Neurosurgery, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- 5Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Neurosurgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 7Division of Neurooncology and Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 8Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 9Department of Neurosurgery, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- 10Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 11Department of Neurosurgery, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea
- 12Department of Neurosurgery, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea
- 13Department of Radiation Oncology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 14Department of Radiation Oncology, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- 15Department of Neurosurgery, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 16Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea
- 17Division of Hematology/ Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 18Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 19Department of Radiation Oncology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 20Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 21Department of Neurosurgery, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 22Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 23Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 24Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 25Department of Hospital Pathology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 26Department of Cancer Control, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- KMID: 2500116
- DOI: http://doi.org/10.14791/btrt.2020.8.e5
Abstract
- Background
: The Guideline Working Group of the Korean Society for Neuro-Oncology (KSNO) conducted a nationwide questionnaire survey for diverse queries faced in the treatment of brain tumors. As part I of the survey, the aim of this study is to evaluate national patterns of clinical practice about antiepileptic drug (AED) and steroid usage for management of brain tumors.
Methods
: A web-based survey was sent to all members of the KSNO by email. The survey included 9 questions of AED usage and 5 questions of steroid usage for brain tumor patients. All questions were developed by consensus of the Guideline Working Group.
Results
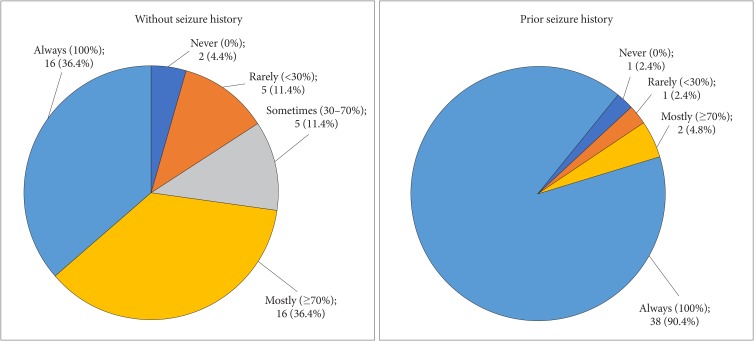
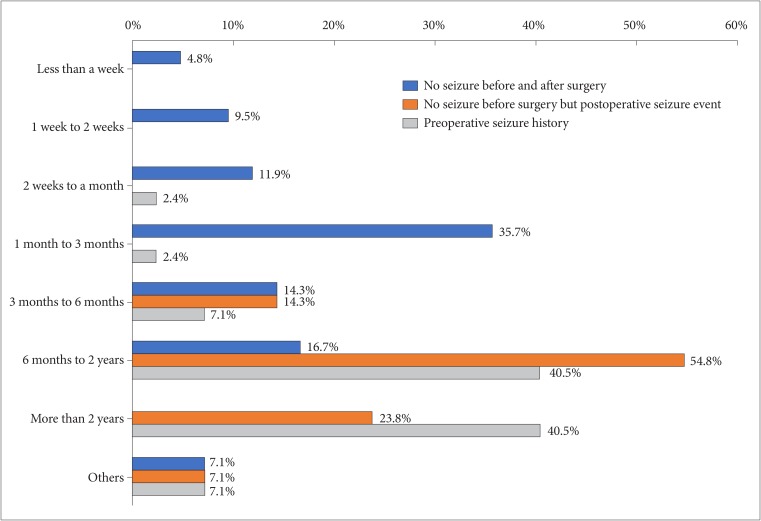
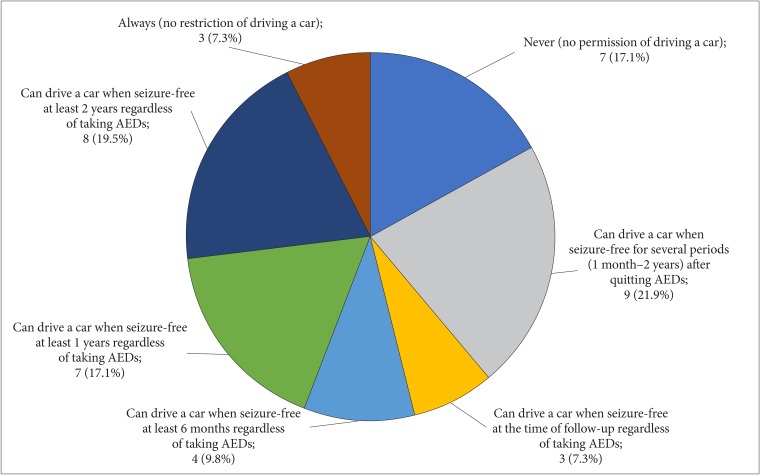
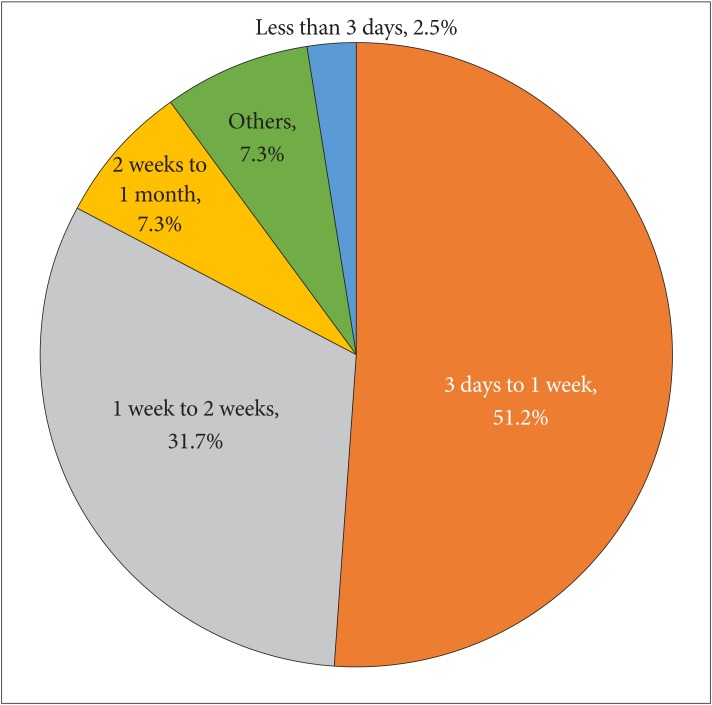
: The overall response rate was 12.8% (54/423). Regarding AED usage, the majority of respondents (95.2%) routinely prescribed prophylactic AEDs for patients with seizure at the peri/postoperative period. However, as many as 72.8% of respondents prescribed AED routinely for seizure-naïve patients, and others prescribed AED as the case may be. The duration of AED prophylaxis showed wide variance according to the epilepsy status and the location of tumor. Levetiracetam (82.9%) was the most preferred AED for epilepsy prophylaxis. Regarding steroid usage, 90.5% of respondents use steroids in perioperative period, including 34.2% of them as a routine manner. Presence of peritumoral edema (90.9%) was considered as the most important factor determining steroid usage followed by degree of clinical symptoms (60.6%). More than half of respondents (51.2%) replied to discontinue the steroids within a week after surgery if there are no specific medical conditions, while 7.3% preferred slow tapering up to a month after surgery.
Conclusion
: The survey demonstrated the prevailing practice patterns on AED and steroid usage in neuro-oncologic field among members of the KSNO. This information provides a point of reference for establishing a practical guideline in the management of brain tumor patients.
Keyword
Figure
Reference
-
1. Sayegh ET, Fakurnejad S, Oh T, Bloch O, Parsa AT. Anticonvulsant prophylaxis for brain tumor surgery: determining the current best available evidence. J Neurosurg. 2014; 121:1139–1147. PMID: 25170671.2. Klimek M, Dammers R. Antiepileptic drug therapy in the perioperative course of neurosurgical patients. Curr Opin Anaesthesiol. 2010; 23:564–567. PMID: 20689411.3. Sughrue ME, Rutkowski MJ, Chang EF, et al. Postoperative seizures following the resection of convexity meningiomas: are prophylactic anticonvulsants indicated? Clinical article. J Neurosurg. 2011; 114:705–709. PMID: 20578801.4. Gutin PH. Corticosteroid therapy in patients with cerebral tumors: benefits, mechanisms, problems, practicalities. Semin Oncol. 1975; 2:49–56. PMID: 795033.5. Weissman DE, Dufer D, Vogel V, Abeloff MD. Corticosteroid toxicity in neuro-oncology patients. J Neurooncol. 1987; 5:125–128. PMID: 3668609.6. Glantz MJ, Cole BF, Forsyth PA, et al. Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000; 54:1886–1893. PMID: 10822423.7. De Santis A, Villani R, Sinisi M, Stocchetti N, Perucca E. Add-on phenytoin fails to prevent early seizures after surgery for supratentorial brain tumors: a randomized controlled study. Epilepsia. 2002; 43:175–182. PMID: 11903465.8. Naito HK, Gatautis VJ, Popowniak KL. Letter: effect of mannitol (osmitrol) intoxication on serum “triglyceride” values. Clin Chem. 1976; 22:935–936. PMID: 1277494.9. Sirven JI, Wingerchuk DM, Drazkowski JF, Lyons MK, Zimmerman RS. Seizure prophylaxis in patients with brain tumors: a meta-analysis. Mayo Clin Proc. 2004; 79:1489–1494. PMID: 15595331.10. Tremont-Lukats IW, Ratilal BO, Armstrong T, Gilbert MR. Antiepileptic drugs for preventing seizures in people with brain tumors. Cochrane Database Syst Rev. 2008; (2):CD004424. PMID: 18425902.11. Bauer R, Ortler M, Seiz-Rosenhagen M, Maier R, Anton JV, Unterberger I. Treatment of epileptic seizures in brain tumors: a critical review. Neurosurg Rev. 2014; 37:381–388. discussion 388. PMID: 24760366.12. Vecht CJ, Wagner GL, Wilms EB. Interactions between antiepileptic and chemotherapeutic drugs. Lancet Neurol. 2003; 2:404–409. PMID: 12849118.13. Bénit CP, Vecht CJ. Seizures and cancer: drug interactions of anticonvulsants with chemotherapeutic agents, tyrosine kinase inhibitors and glucocorticoids. Neurooncol Pract. 2016; 3:245–260. PMID: 31385988.14. Kerrigan S, Grant R. Antiepileptic drugs for treating seizures in adults with brain tumours. Cochrane Database Syst Rev. 2011; (8):CD008586. PMID: 21833969.15. Chen Y, Tsai YH, Tseng SH. Valproic acid affected the survival and invasiveness of human glioma cells through diverse mechanisms. J Neurooncol. 2012; 109:23–33. PMID: 22528797.16. Scicchitano BM, Sorrentino S, Proietti G, et al. Levetiracetam enhances the temozolomide effect on glioblastoma stem cell proliferation and apoptosis. Cancer Cell Int. 2018; 18:136. PMID: 30214378.17. Nozawa A, Ozeki M, Matsuoka M, et al. Perampanel inhibits neuroblastoma cell proliferation through down-regulation of AKT and ERK pathways. Anticancer Res. 2019; 39:3595–3599. PMID: 31262884.18. Dietrich J, Rao K, Pastorino S, Kesari S. Corticosteroids in brain cancer patients: benefits and pitfalls. Expert Rev Clin Pharmacol. 2011; 4:233–242. PMID: 21666852.19. Chang SM, Messersmith H, Ahluwalia M, et al. Anticonvulsant prophylaxis and steroid use in adults with metastatic brain tumors: summary of SNO and ASCO endorsement of the Congress of Neurological Surgeons guidelines. Neuro Oncol. 2019; 21:424–427. PMID: 30883663.20. Vecht CJ, Hovestadt A, Verbiest HB, van Vliet JJ, van Putten WL. Dose-effect relationship of dexamethasone on Karnofsky performance in metastatic brain tumors: a randomized study of doses of 4, 8, and 16 mg per day. Neurology. 1994; 44:675–680. PMID: 8164824.21. Kostaras X, Cusano F, Kline GA, Roa W, Easaw J. Use of dexamethasone in patients with high-grade glioma: a clinical practice guideline. Curr Oncol. 2014; 21:e493–e503. PMID: 24940109.22. Aulakh R, Singh S. Strategies for minimizing corticosteroid toxicity: a review. Indian J Pediatr. 2008; 75:1067–1073. PMID: 19023531.23. Maricic M. Update on glucocorticoid-induced osteoporosis. Rheum Dis Clin North Am. 2011; 37:415–431. PMID: 22023900.24. Pruitt AA. Medical management of patients with brain tumors. Continuum (Minneap Minn). 2015; 21:314–331. PMID: 25837898.