Korean J Radiol.
2020 Apr;21(4):462-470. 10.3348/kjr.2019.0449.
Perceived Dark Rim Artifact in First-Pass Myocardial Perfusion Magnetic Resonance Imaging Due to Visual Illusion
- Affiliations
-
- 1Division of Mechanical and Biomedical Engineering, Ewha Womans University, Seoul, Korea. shinage@gmail.com
- 2Department of Medicine, Case Western Reserve University, Cleveland, OH, USA.
- 3Ming Hsieh Department of Electrical Engineering, University of Southern California, Los Angeles, CA, USA.
- 4Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
- KMID: 2471812
- DOI: http://doi.org/10.3348/kjr.2019.0449
Abstract
OBJECTIVE
To demonstrate that human visual illusion can contribute to sub-endocardial dark rim artifact in contrast-enhanced myocardial perfusion magnetic resonance images.
MATERIALS AND METHODS
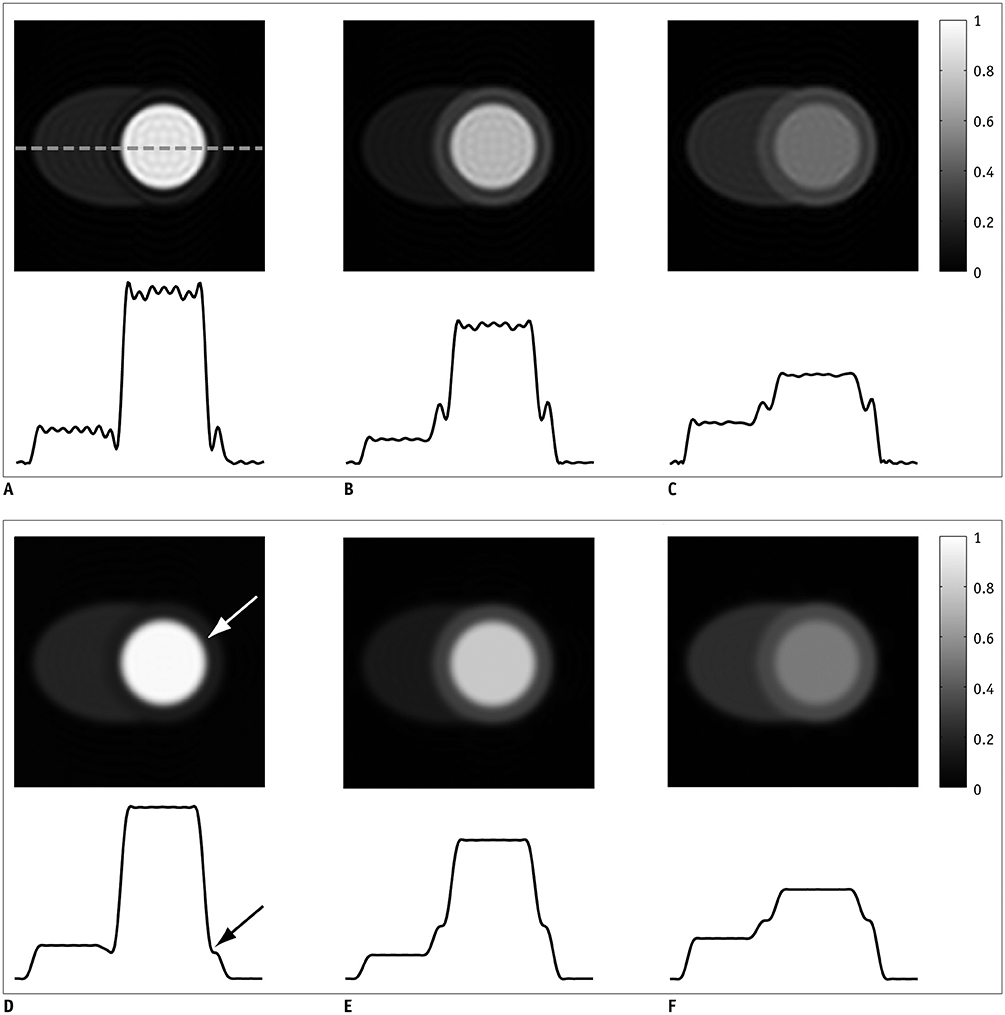
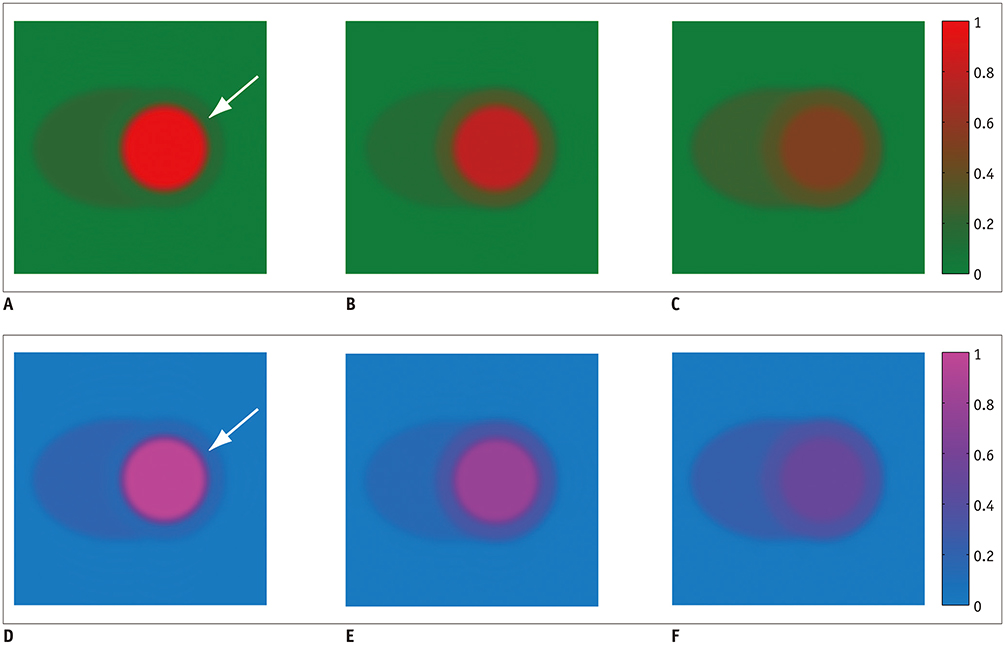
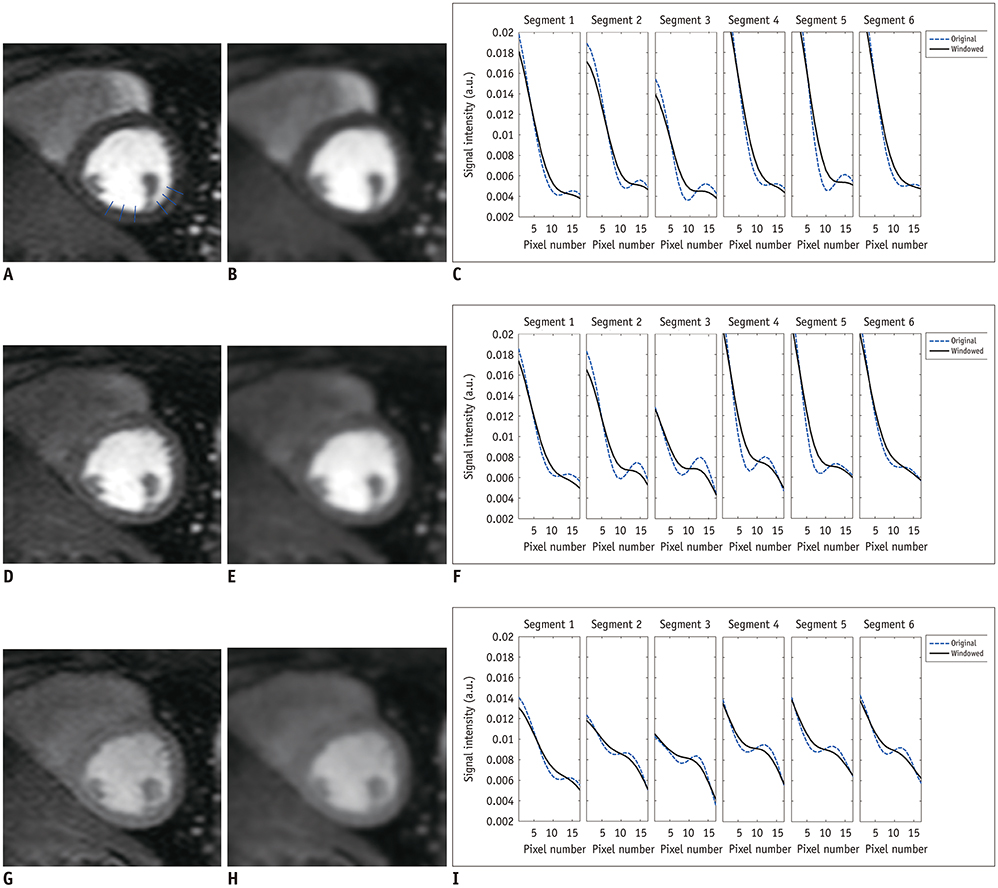
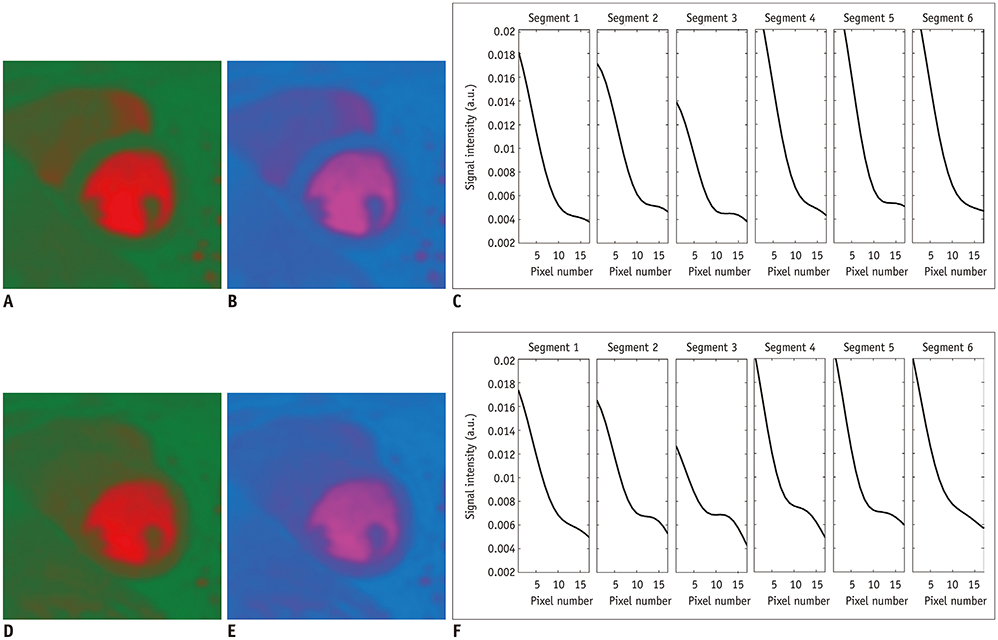
Numerical phantoms were generated to simulate the first-passage of contrast agent in the heart, and rendered in conventional gray scale as well as in color scale with reduced luminance variation. Cardiac perfusion images were acquired from two healthy volunteers, and were displayed by the same gray and color scales used in the numerical study. Before and after k-space windowing, the left ventricle (LV)-myocardium boarders were analyzed visually and quantitatively through intensity profiles perpendicular the boarders.
RESULTS
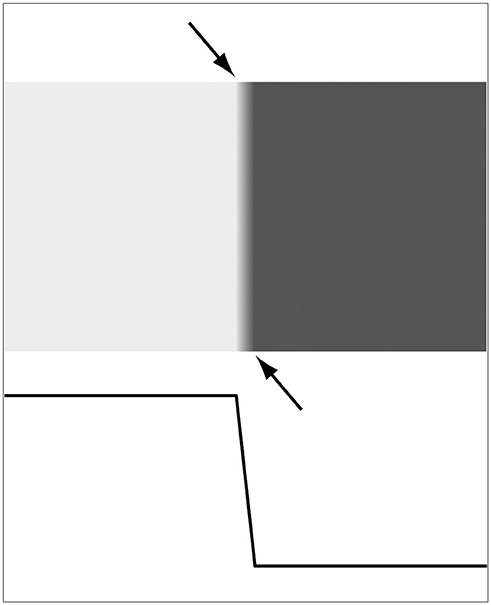
k-space windowing yielded monotonically decreasing signal intensity near the LV-myocardium boarder in the phantom images, as confirmed by negative finite difference values near the board ranging −1.07 to −0.14. However, the dark band still appears, which is perceived by visual illusion. Dark rim is perceived in the in-vivo images after k-space windowing that removed the quantitative signal dip, suggesting that the perceived dark rim is a visual illusion. The perceived dark rim is stronger at peak LV enhancement than the peak myocardial enhancement, due to the larger intensity difference between LV and myocardium. In both numerical phantom and in-vivo images, the illusory dark band is not visible in the color map due to reduced luminance variation.
CONCLUSION
Visual illusion is another potential cause of dark rim artifact in contrast-enhanced myocardial perfusion MRI as demonstrated by illusory rim perceived in the absence of quantitative intensity undershoot.
MeSH Terms
Figure
Reference
-
1. Gerber BL, Raman SV, Nayak K, Epstein FH, Ferreira P, Axel L, et al. Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art. J Cardiovasc Magn Reson. 2008; 10:18.
Article2. Jo Y, Kim J, Park CH, Lee JW, Hur JH, Yang DH, et al. Guideline for cardiovascular magnetic resonance imaging from the Korean Society of Cardiovascular Imaging-Part 1: standardized protocol. Korean J Radiol. 2019; 20:1313–1333.
Article3. Lee JW, Hur JH, Yang DH, Lee BY, Im DJ, Hong SJ, et al. Guidelines for cardiovascular magnetic resonance imaging from the Korean Society of Cardiovascular Imaging-Part 2: interpretation of cine, flow, and angiography data. Korean J Radiol. 2019; 20:1477–1490.
Article4. Wolff SD, Schwitter J, Coulden R, Friedrich MG, Bluemke DA, Biederman RW, et al. Myocardial first-pass perfusion magnetic resonance imaging: a multicenter dose-ranging study. Circulation. 2004; 110:732–737.5. Plein S, Radjenovic A, Ridgway JP, Barmby D, Greenwood JP, Ball SG, et al. Coronary artery disease: myocardial perfusion MR imaging with sensitivity encoding versus conventional angiography. Radiology. 2005; 235:423–430.
Article6. Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, et al. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol. 2007; 49:2440–2244.7. Meyer C, Strach K, Thomas D, Litt H, Nähle CP, Tiemann K, et al. High-resolution myocardial stress perfusion at 3 T in patients with suspected coronary artery disease. Eur Radiol. 2008; 18:226–233.
Article8. Gebker R, Jahnke C, Paetsch I, Kelle S, Schnackenburg B, Fleck E, et al. Diagnostic performance of myocardial perfusion MR at 3 T in patients with coronary artery disease. Radiology. 2008; 247:57–63.
Article9. Di Bella EV, Parker DL, Sinusas AJ. On the dark rim artifact in dynamic contrast-enhanced MRI myocardial perfusion studies. Magn Reson Med. 2005; 54:1295–1299.
Article10. Arai AE. Magnetic resonance first-pass myocardial perfusion imaging. Top Magn Reson Imaging. 2000; 11:383–398.
Article11. Plein S, Ryf S, Schwitter J, Radjenovic A, Boesiger P, Kozerke S. Dynamic contrast-enhanced myocardial perfusion MRI accelerated with k-t SENSE. Magn Reson Med. 2007; 58:777–785.12. Storey P, Chen Q, Li W, Edelman RR, Prasad PV. Band artifacts due to bulk motion. Magn Reson Med. 2002; 48:1028–1036.
Article13. Zhao L, Saleno M, Kramer CM, Meyer CM. The contribution of cardiac motion to dark rim artifacts in myocardial perfusion scans. In : Proceeding of International Society for Magnetic Resonance in Medicine, 18th Annual Meeting; 2010 May 1–7; Stockholm, Sweden:14. Albert MS, Huang W, Lee JH, Patlak CS, Springer CS Jr. Susceptibility changes following bolus injections. Magn Reson Med. 1993; 29:700–708.
Article15. Schreiber WG, Schmitt M, Kalden P, Mohrs OK, Kreitner KF, Thelen M. Dynamic contrast-enhanced myocardial perfusion imaging using saturation-prepared TrueFISP. J Magn Reson Imaging. 2002; 16:641–652.
Article16. Ferreira P, Gatehouse P, Bucciarelli-Ducci C, Wage R, Firmin D. Measurement of myocardial frequency offsets during first pass of a gadolinium-based contrast agent in perfusion studies. Magn Reson Med. 2008; 60:860–870.
Article17. Rodieck RW, Stone J. Analysis of receptive fields of cat retinal ganglion cells. J Neurophysiol. 1965; 28:833–849.
Article18. Fiorentini A. Mach band phenomena. In : Alpern M, Aulhorn E, Barlow HB, Baumgardt E, Blackwell HR, Blough DS, editors. Handbook of sensory physiology, vol VII-4. Berlin: Springer;1972. p. 188–201.19. Pessoa L. Mach bands: how many models are possible? Recent experimental findings and modeling attempts. Vision Res. 1996; 36:3205–3322.
Article20. Pease PL. On color mach bands. Vision Res. 1978; 18:751–755.
Article21. Ferreira P, Gatehouse P, Kellman P, Bucciarelli-Ducci C, Firmin D. Variability of myocardial perfusion dark rim Gibbs artifacts due to sub-pixel shifts. J Cardiovasc Magn Reson. 2009; 11:17.
Article22. Strickland RN, Kim CS, McDonnell WF. Luminance, hue, and saturation processing of digital color images. In : SPIE conference on applications of digital image processing; 1986 August 17; San Diego, CA, USA:23. Kellman P, Epstein FH, McVeigh ER. Adaptive sensitivity encoding incorporating temporal filtering (TSENSE). Magn Reson Med. 2001; 45:846–852.
Article24. Williams D, Sekiguchi N, Brainard D. Color, contrast sensitivity, and the cone mosaic. Proc Natl Acad Sci U S A. 1993; 90:9770–9777.
Article25. Palmer SE. Vision science: photons to phenomenology. Cambridge, MA: MIT Press;1999.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac MRI
- Assessment of Myocardial Ischemia Using Stress Perfusion Cardiovascular Magnetic Resonance
- Stress Testing and Imaging Protocols for Myocardial Perfusion Studies
- Viable myocardium in reperfused acute myocardial infarction: rest and stress first-pass mr imaging
- Myocardial Contractility, Perfusion, and Viability Analysis Using Multidetector CT in Patients with Ischemic Heart Disease