J Korean Ophthalmol Soc.
2020 Mar;61(3):307-312. 10.3341/jkos.2020.61.3.307.
Regression of Neovascularization after Using Only Intraocular Pressure-lowering Medications in Neovascular Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, Nowon Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea. csckek@gmail.com
- KMID: 2471774
- DOI: http://doi.org/10.3341/jkos.2020.61.3.307
Abstract
- PURPOSE
To report a case of neovascular glaucoma after intraocular lens iris fixation, in which the neovascularization of the iris and the anterior chamber improved with only intraocular pressure (IOP) lowering agents, without treatment of the underlying cause.
CASE SUMMARY
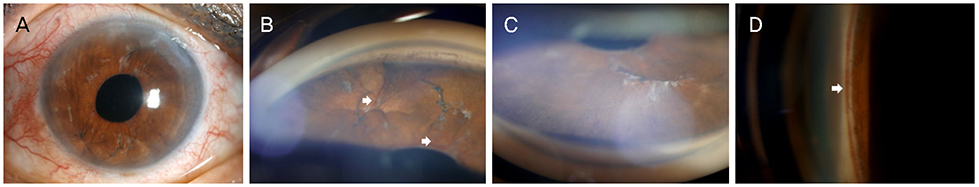
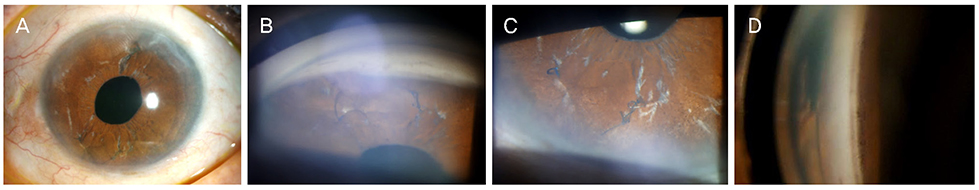
A 74-year-old woman who had undergone bilateral cataract surgery presented with left ocular pain and headache that started 3 days previously. At the initial examination, the best-corrected visual acuity was 0.9, and the IOP was 38 mmHg in the left eye. Slit-lamp examination of the left eye revealed diffuse iris neovascularization and several polypropylene suture knots fixated in the superior and inferior iris. Gonioscopic examination revealed angle neovascularization in all quadrants, with focal peripheral anterior synechia in the inferior quadrant. Fundus examination presented inferior neuroretinal rim thinning and an inferior retinal nerve fiber layer defect in the left eye. Fluorescent angiography showed no ischemic retinal lesions, with the exception of several retinal microaneurysms. Six months after topical IOP-lowering treatment in the left eye, the IOP was 10 mmHg, and neovascularization of the iris and angle had regressed completely.
CONCLUSIONS
In the case of early-stage neovascular glaucoma with partial angle closure not associated with retinal ischemia, IOP-lowering treatment can be effective without other invasive procedures.
Keyword
MeSH Terms
Figure
Reference
-
1. Sivak-Callcott JA, O'Day DM, Gass JD, Tsai JC. Evidence-based recommendations for the diagnosis and treatment of neovascular glaucoma. Ophthalmology. 2001; 108:1767–1776.2. Shazly TA, Latina MA. Neovascular glaucoma: etiology, diagnosis and prognosis. Semin Ophthalmol. 2009; 24:113–121.
Article3. Hayreh SS. Neovascular glaucoma. Prog Retin Eye Res. 2007; 26:470–485.
Article4. Jeong YC, Hwang YH. Etiology and features of eyes with rubeosis iridis among Korean patients: A Population-Based Single Center Study. PLoS One. 2016; 11:e0160662.
Article5. Cohen S, Kremer I, Yassur Y, Ben-Sira I. Peripheral retinal neovascularization and rubeosis iridis after a bilateral circular buckling operation. Ann Ophthalmol. 1988; 20:153–156.6. Barile GR, Chang S, Horowitz JD, et al. Neovascular complications associated with rubeosis iridis and peripheral retinal detachment after retinal detachment surgery. Am J Ophthalmol. 1998; 126:379–389.
Article7. Aref AA. Current management of glaucoma and vascular occlusive disease. Curr Opin Ophthalmol. 2016; 27:140–145.
Article8. Wakabayashi T, Oshima Y, Sakaguchi H, et al. Intravitreal bevacizumab to treat iris neovascularization and neovascular glaucoma secondary to ischemic retinal diseases in 41 consecutive cases. Ophthalmology. 2008; 115:1571–1580. 80.e1–80.e3.
Article9. Wand M, Dueker DK, Aiello LM, Grant WM. Effects of panretinal photocoagulation on rubeosis iridis, angle neovascularization, and neovascular glaucoma. Am J Ophthalmol. 1978; 86:332–339.
Article10. Iliev ME, Domig D, Wolf-Schnurrbursch U, et al. Intravitreal bevacizumab (Avastin) in the treatment of neovascular glaucoma. Am J Ophthalmol. 2006; 142:1054–1056.
Article11. Batman C, Ozdamar Y. The effect of bevacizumab for anterior segment neovascularization after silicone oil removal in eyes with previous vitreoretinal surgery. Eye (Lond). 2010; 24:1243–1246.
Article12. Mason JO 3rd, Albert MA Jr, Mays A, Vail R. Regression of neovascular iris vessels by intravitreal injection of bevacizumab. Retina. 2006; 26:839–841.
Article13. Costa VP, Harris A, Anderson D, et al. Ocular perfusion pressure in glaucoma. Acta Ophthalmol. 2014; 92:e252–e266.
Article14. Rolle T, Tofani F, Brogliatti B, Grignolo FM. The effects of dorzolamide 2% and dorzolamide/timolol fixed combination on retinal and optic nerve head blood flow in primary open-angle glaucoma patients. Eye (Lond). 2008; 22:1172–1179.
Article15. Siesky B, Harris A, Cantor LB, et al. A comparative study of the effects of brinzolamide and dorzolamide on retinal oxygen saturation and ocular microcirculation in patients with primary open-angle glaucoma. Br J Ophthalmol. 2008; 92:500–504.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraviteal Bevacizumab (Avastin(R)) Injection for the Treatment of Early-Stage Neovascular Glaucoma
- Molteno Implantation for Neovascular Glaucoma with a Laser-Releasable Intracameral Ligature to Limit Postoperative Pressure Fluctuations
- Photodynamic Therapy with Verteporfin for Anterior Segment Neovascularization in Neovascualr Galucoma
- Intravitreal Bevacizumab for the Treatment of Neovascular Glaucoma Associated With Central Retinal Artery Occlusion
- Effect of Simultaneous Intravitreal Bevacizumab and Retrobulbar Triamcinolone Injection in Refractory Neovascular Glaucoma