Ann Dermatol.
2020 Apr;32(2):164-167. 10.5021/ad.2020.32.2.164.
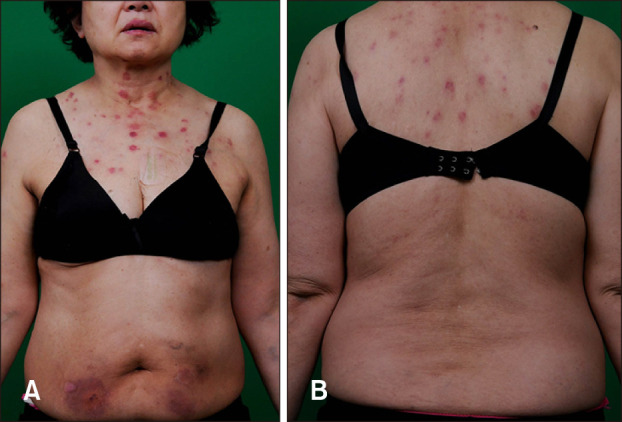
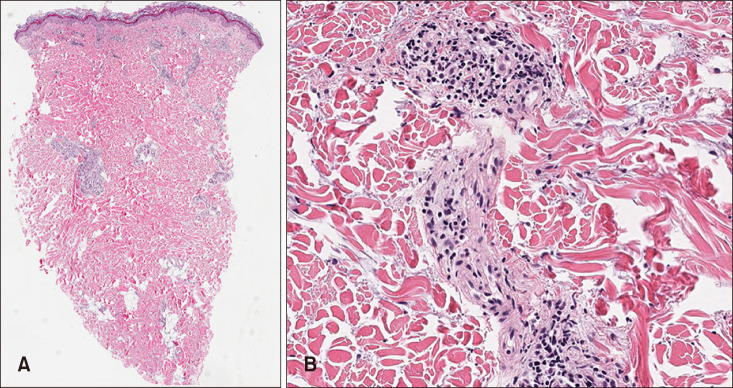
A Case of Cutaneous Leukocytoclastic Vasculitis Associated with Granulocyte Colony-Stimulating Factor: An Unusual Presentation
- Affiliations
-
- 1Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jh1204.park@samsung.com
- KMID: 2471345
- DOI: http://doi.org/10.5021/ad.2020.32.2.164
Abstract
- Drug-induced vasculitis is an inflammation of small-sized blood vessel caused by the use of drugs. It accounts for approximately 10% of acute cutaneous vasculitis. Propylthiouracil, hydralazine, and allopurinol have been widely known as causative agents. The most common clinical feature of drug-induced vasculitis is palpable purpura on lower extremities. A 66-year-old Korean female presented with erythematous nodules on upper chest and back. She had been on medication for multiple myeloma. Laboratory results showed neutropenia. After a single injection of filgrastim (recombinant granulocyte colony-stimulating factor), she developed cutaneous lesions with concurrent increase in absolute neutrophil count. A skin biopsy revealed leukocytoclastic vasculitis. After discontinuation of filgrastim injection, her skin lesions disappeared spontaneously.
MeSH Terms
-
Aged
Allopurinol
Biopsy
Blood Vessels
Female
Filgrastim
Granulocyte Colony-Stimulating Factor*
Granulocytes*
Humans
Hydralazine
Inflammation
Lower Extremity
Multiple Myeloma
Neutropenia
Neutrophils
Propylthiouracil
Purpura
Skin
Thorax
Vasculitis
Vasculitis, Leukocytoclastic, Cutaneous*
Allopurinol
Filgrastim
Granulocyte Colony-Stimulating Factor
Hydralazine
Propylthiouracil
Figure
Reference
-
1. White JM, Mufti GJ, Salisbury JR, du Vivier AW. Cutaneous manifestations of granulocyte colony-stimulating factor. Clin Exp Dermatol. 2006; 31:206–207. PMID: 16487091.
Article2. Ross HJ, Moy LA, Kaplan R, Figlin RA. Bullous pyoderma gangrenosum after granulocyte colony-stimulating factor treatment. Cancer. 1991; 68:441–443. PMID: 1712666.
Article3. Cottle TE, Fier CJ, Donadieu J, Kinsey SE. Risk and benefit of treatment of severe chronic neutropenia with granulocyte colony-stimulating factor. Semin Hematol. 2002; 39:134–140. PMID: 11957197.
Article4. Ippoliti G, Paulli M, Lucioni M, Lauriola M, D'Armini AM. Leukocytoclastic vasculitis as a complication of recombinant granulocyte colony-stimulating factor therapy in a heart transplant patient. Case Rep Transplant. 2014; 2014:160407. PMID: 24600524.
Article5. El Husseiny NM, Mattar MM. Aggressive cutaneous vasculitis in a patient with chronic lymphatic leukemia following granulocyte colony stimulating factor injection: a case report. J Med Case Rep. 2011; 5:88. PMID: 21362198.
Article6. Kilic SS, Mustafayeva S, Ipek K, Adim SB. Leukocytoclastic vasculitis in patients with severe congenital neutropenia. J Trop Pediatr. 2010; 56:359–362. PMID: 20100783.
Article7. Andavolu MV, Logan LJ. Leukocytoclastic vasculitis as a complication of granulocyte colony-stimulating factor (G-CSF) -- a case study. Ann Hematol. 1999; 78:79–81. PMID: 10089022.
Article8. Jain KK. Cutaneous vasculitis associated with granulocyte colony-stimulating factor. J Am Acad Dermatol. 1994; 31(2 Pt 1):213–215. PMID: 7518847.
Article9. Ito Y, Noda K, Aiba K, Yano S, Fujii T. [Diffuse large B-cell lymphoma complicated with drug-induced vasculitis during administration of pegfilgrastim]. Rinsho Ketsueki. 2017; 58:2238–2242. Japanese. PMID: 29212975.10. Elsner J, Roesler J, Emmendörffer A, Zeidler C, Lohmann-Matthes ML, Welte K. Altered function and surface marker expression of neutrophils induced by rhG-CSF treatment in severe congenital neutropenia. Eur J Haematol. 1992; 48:10–19. PMID: 1370419.
Article11. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw Hill;2012. p. 456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Granulocyte Colony-stimulating Factor InducedVasculitis with Atypical Myeloid Cells
- Sweet Syndrome in a Child with Aplastic Anemia after Receiving Recombinant Granulocyte Colony-stimulating Factor
- Two cases of congenital agranulocytosis treated with recombinant human granulocyte colony-stimulating factor
- The effect of granulocyte colony-stimulating factor in chemotherapy of acute myelogenous leukemia
- The effects on the production of platelet activating factor in the cultured human endothelial cells by interleukin-6 and granulocyte macrophage colony stimulating factor