Ann Dermatol.
2020 Apr;32(2):159-163. 10.5021/ad.2020.32.2.159.
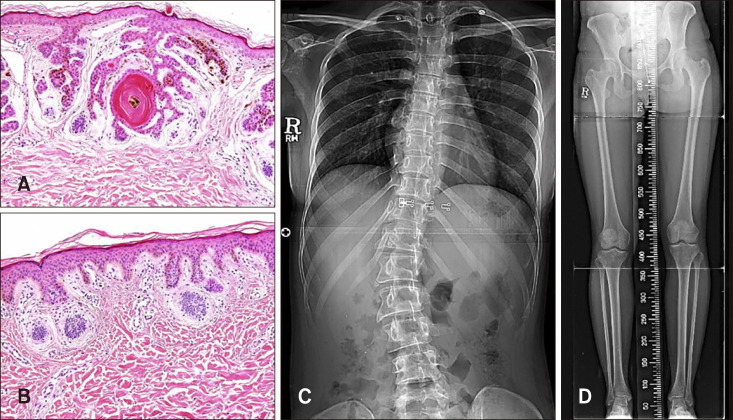
Happle-Tinschert Syndrome: A Case Report of Unilateral Segmentally Arranged Basaloid Follicular Hamartoma with Scoliosis and Review of Literature
- Affiliations
-
- 1Department of Dermatology, Gangnam Severance Hospital, Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea. kimsc@yuhs.ac
- KMID: 2471344
- DOI: http://doi.org/10.5021/ad.2020.32.2.159
Abstract
- Happle-Tinschert syndrome is a rare disease characterized by unilateral, segmentally arranged basaloid follicular hamartoma (BFH) with osseous, dental, and cerebral anomalies. Although BFH has been demonstrated to be associated with mutations in the patched gene, the genetic basis for Happle-Tinschert syndrome is still unknown. We describe a case of Happle-Tinschert syndrome in a 26-year-old female. The patient presented with unilateral skin color change to brownish papules and atrophoderma following the development of Blaschko's lines, plantar pitting, and nail dystrophy on the right side of the body. She also had scoliosis, hemihypotrophy, and dental anomalies. The skin lesions were histologically confirmed as BFHs. Next-generation sequencing of the patient's genomic DNA obtained from a peripheral blood sample identified no pathogenic mutation. This case illustrates the characteristic clinical features of Happle-Tinschert syndrome. Thus far, 14 cases of Happle-Tinschert syndrome have been reported, and we report another case of this syndrome.
Figure
Reference
-
1. El-Darouti MA, Marzouk SA, Abdel-Halim MR, Zidan AZ, Fawzy MM. Basaloid follicular hamartoma. Int J Dermatol. 2005; 44:361–365. PMID: 15869532.
Article2. Saxena A, Shapiro M, Kasper DA, Fitzpatrick JE, Mellette JR Jr. Basaloid follicular hamartoma: a cautionary tale and review of the literature. Dermatol Surg. 2007; 33:1130–1135. PMID: 17760608.
Article3. Happle R, Tinschert S. Segmentally arranged basaloid follicular hamartomas with osseous, dental and cerebral anomalies: a distinct syndrome. Acta Derm Venereol. 2008; 88:382–387. PMID: 18709310.4. Itin PH. Happle-Tinschert syndrome. Segmentally arranged basaloid follicular hamartomas, linear atrophoderma with hypo- and hyperpigmentation, enamel defects, ipsilateral hypertrichosis, and skeletal and cerebral anomalies. Dermatology. 2009; 218:221–225. PMID: 19005246.5. Lo CS, Wu YF, Hsiao YW, Chung WH, Yang CH. Unilateral segmentally arranged basaloid follicular hamartomas with osteoma cutis and hypodontia: a case of Happle-Tinschert syndrome. Clin Exp Dermatol. 2013; 38:862–865. PMID: 24252078.
Article6. Haneef NS, Ramachandra S, Metta AK, Sushmalatha B, Bellam SS, Ohatkar N. Happle-Tinschert syndrome: report of a newly delineated entity. Indian J Dermatol Venereol Leprol. 2014; 80:71–73. PMID: 24448134.
Article7. Özgur A, Çabuk G, Arpacı R, Baz K, Katar D. Happle-Tinschert syndrome: report of a case with hemimegalencephaly. Korean J Radiol. 2014; 15:534–537. PMID: 25053915.
Article8. Boccaletti V, Accorsi P, Pinelli L, Ungari M, Giordano L, Neri I, et al. Congenital systematized basaloid follicular hamartoma with microphthalmia and hemimegalencephaly. Pediatr Dermatol. 2011; 28:555–560. PMID: 21062348.
Article9. Carney RG. Linear unilateral basal-cell nevus with comedones; report of a case. AMA Arch Derm Syphilol. 1952; 65:471–476. PMID: 14902117.10. Lausecker H. Beitrag zu den Naevo-Epitheliomen. Arch Dermatol Syph. 1952; 194:639–662. German. PMID: 12997006.
Article11. Kraus Z, Vortel V. Tardive unilateral basal cell naevus with comedones (in Czech). Sborn Ved Praci Lek Fak Karlovy Univ Hradec Kralove. 1960; 3:58–65.12. Bleiberg J, Brodkin RH. Linear unilateral basal cell nevus with comedones. Arch Dermatol. 1969; 100:187–190. PMID: 5797959.
Article13. Burck U, Arnold H, Siebert J. Unilateral skin lesions associated with multiple neoplasms. Dermatologica. 1984; 168:78–81. PMID: 6698267.
Article14. Aloi FG, Tomasini CF, Isaia G, Grazia Bernengo M. Unilateral linear basal cell nevus associated with diffuse osteoma cutis, unilateral anodontia, and abnormal bone mineralization. J Am Acad Dermatol. 1989; 20(5 Pt 2):973–978. PMID: 2715453.
Article15. Zarour H, Grob JJ, Choux R, Collet-Villette AM, Bonerandi JJ. Hamartome baso-cellulaire et annexiel unilatéral linéaire (ou nævus baso-cellulaire unilateral linéaire). Ann Dermatol Venereol. 1992; 119:901–903. PMID: 1301717.16. Alpsoy E, Durusoy C, Ozbilim G, Karpuzoğlu G, Yilmaz E. Nevus comedonicus syndrome: a case associated with multiple basal cell carcinomas and a rudimentary toe. Int J Dermatol. 2005; 44:499–501. PMID: 15941441.
Article17. Zenker M, Tinschert S, Wieland I, Schanze D, Happle R. A postzygotic SMO mutation caused the original case of Happle-Tinschert syndrome. Acta Derm Venereol. 2018; 98:534–535. PMID: 29335739.
Article18. Khamaysi Z, Bochner R, Indelman M, Magal L, Avitan-Hersh E, Sarig O, et al. Segmental basal cell naevus syndrome caused by an activating mutation in smoothened. Br J Dermatol. 2016; 175:178–181. PMID: 26822128.19. Happle R, Tinschert S. Happle-Tinschert syndrome can be caused by a mosaic SMO mutation and is suggested to be a variant of Curry-Jones syndrome. Br J Dermatol. 2016; 175:1108. PMID: 27484736.
Article20. Khamaysi Z, Sprecher E, Bergman R. Happle-Tinschert syndrome can be caused by a mosaic SMO mutation and is suggested to be a variant of Curry-Jones syndrome: reply from the authors. Br J Dermatol. 2016; 175:1109.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Happle-Tinschert Syndrome: Report of a Case with Hemimegalencephaly
- A Case of Familial Basaloid Follicular Hamartoma Syndrome
- A Case of Basaloid Follicular Hamartoma Combined with Basal Cell Epithelioma
- A Case of Multiple Basaloid Follicular Harmatoma
- Segmentally Arranged Hyperpigmented Basaloid Follicular Hamartoma