Korean J Radiol.
2020 Mar;21(3):377-383. 10.3348/kjr.2019.0724.
Feasibility of Adjustable Electrodes for Radiofrequency Ablation of Benign Thyroid Nodules
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jhshin11@skku.edu
- KMID: 2470762
- DOI: http://doi.org/10.3348/kjr.2019.0724
Abstract
OBJECTIVE
The purpose of this study was to evaluate a novel radiofrequency ablation (RFA) application utilizing an adjustable electrode for treatment of benign thyroid nodules.
MATERIALS AND METHODS
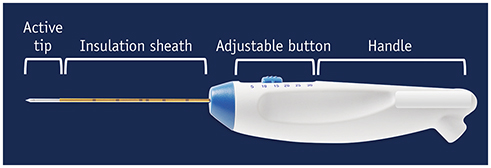
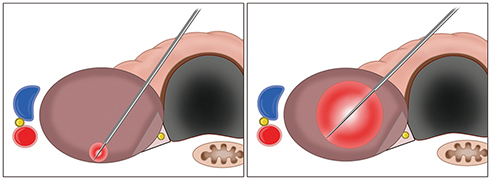
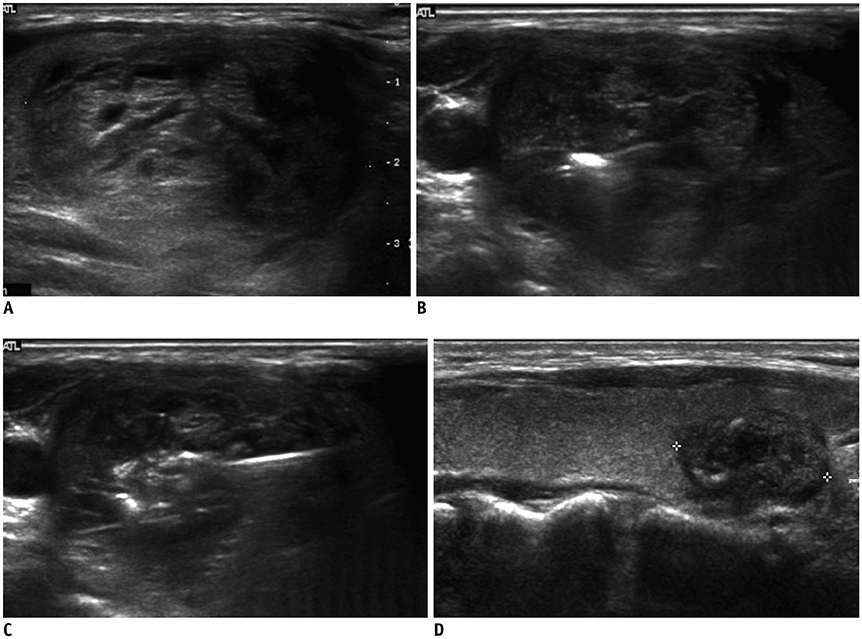
From April 2011 to December 2018, 21 patients underwent RFA treatment on 21 thyroid nodules, utilizing an 18-gauge internally cooled electrode equipped with a size adjustable active tip. The peripheral nodule portions were ablated with the moving-shot technique and a shorter active tip, and the nodule centers were ablated with the fixed technique and a longer active tip. We assessed parameters including characteristics of the treated nodules, use of variablesized active tips, volume reduction rate, therapeutic success rate, and post-procedural complications. The therapeutic success rate was defined as a > 50% volume reduction of the initial nodule volume at the 6- or 12-month follow-up.
RESULTS
The treated thyroid nodules were large enough to cause symptoms (mean volume, 29.6 mL). Two types of active tips per session were used for all nodules. The mean volume reduction rate at the last follow-up was 68.3 ± 4.4% and our therapeutic success rate was 90.5%. Both symptoms and cosmetic scores decreased significantly. Minor complications in three patients were recorded during and after the procedure.
CONCLUSION
This initial study demonstrated that an adjustable electrode for RFA of benign thyroid nodules effectively and safely resulted in volume reduction.
MeSH Terms
Figure
Reference
-
1. Ha EJ, Lim HK, Yoon JH, Baek JH, Do KH, Choi M, et al. Primary imaging test and appropriate biopsy methods for thyroid nodules: guidelines by Korean Society of Radiology and National Evidence-Based Healthcare Collaborating Agency. Korean J Radiol. 2018; 19:623–631.
Article2. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011; 12:1–14.
Article3. Bandeira-Echtler E, Bergerhoff K, Richter B. Levothyroxine or minimally invasive therapies for benign thyroid nodules. Cochrane Database Syst Rev. 2014; (6):CD004098.
Article4. Mauri G, Cova L, Monaco CG, Sconfienza LM, Corbetta S, Benedini S, et al. Benign thyroid nodules treatment using percutaneous laser ablation (PLA) and radiofrequency ablation (RFA). Int J Hyperthermia. 2017; 33:295–299.
Article5. Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, et al. 2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018; 19:632–655.
Article6. Jeong WK, Baek JH, Rhim H, Kim YS, Kwak MS, Jeong HJ, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008; 18:1244–1250.
Article7. Spiezia S, Garberoglio R, Milone F, Ramundo V, Caiazzo C, Assanti AP, et al. Thyroid nodules and related symptoms are stably controlled two years after radiofrequency thermal ablation. Thyroid. 2009; 19:219–225.
Article8. Baek JH, Moon WJ, Kim YS, Lee JH, Lee D. Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg. 2009; 33:1971–1977.
Article9. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol. 2011; 197:W331–W336.
Article10. Cha J, Kim YS, Rhim H, Lim HK, Choi D, Lee MW. Radiofrequency ablation using a new type of internally cooled electrode with an adjustable active tip: an experimental study in ex vivo bovine and in vivo porcine livers. Eur J Radiol. 2011; 77:516–521.
Article11. Kim JH, Baek JH, Lim HK, Na DG. Summary of the 2017 thyroid radiofrequency ablation guideline and comparison with the 2012 guideline. Ultrasonography. 2019; 38:125–134.
Article12. Mauri G, Pacella CM, Papini E, Solbiati L, Goldberg SN, Ahmed M, et al. Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid. 2019; 29:611–618.
Article13. Sung JY, Baek JH, Kim KS, Lee D, Yoo H, Kim JK, et al. Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective randomized study. Radiology. 2013; 269:293–300.
Article14. Ha EJ, Baek JH, Lee JH. Moving-shot versus fixed electrode techniques for radiofrequency ablation: comparison in an ex-vivo bovine liver tissue model. Korean J Radiol. 2014; 15:836–843.15. Baek JH, Ha EJ, Choi YJ, Sung JY, Kim JK, Shong YK. Radiofrequency versus ethanol ablation for treating predominantly cystic thyroid nodules: a randomized clinical trial. Korean J Radiol. 2015; 16:1332–1340.
Article16. Lim HK, Lee JH, Ha EJ, Sung JY, Kim JK, Baek JH. Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol. 2013; 23:1044–1049.
Article17. Jung SL, Baek JH, Lee JH, Shong YK, Sung JY, Kim KS, et al. Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 2018; 19:167–174.
Article18. Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010; 194:1137–1142.
Article19. Ha EJ, Baek JH, Kim KW, Pyo J, Lee JH, Baek SH, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and bayesian network meta-analysis. J Clin Endocrinol Metab. 2015; 100:1903–1911.
Article20. Burke DR, Lewis CA, Cardella JF, Citron SJ, Drooz AT, Haskal ZJ, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. J Vasc Interv Radiol. 2003; 14:S243–S246.
Article21. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
- Non-surgical, Image-guided Management of Benign Thyroid Nodules
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Radiofrequency Ablation of Benign Thyroid Nodule
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules