J Korean Ophthalmol Soc.
2020 Feb;61(2):200-204. 10.3341/jkos.2020.61.2.200.
Corneal Collagen Cross-linking for Corneal Ulcer from Moraxella Group
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. sieh12@schmc.ac.kr
- KMID: 2470743
- DOI: http://doi.org/10.3341/jkos.2020.61.2.200
Abstract
- PURPOSE
To report a case of corneal collagen cross-linking for corneal ulcer caused by the Moraxella group.
CASE SUMMARY
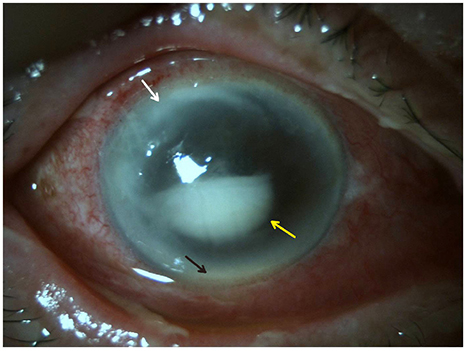
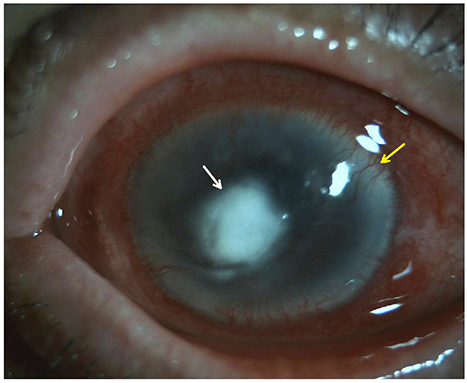
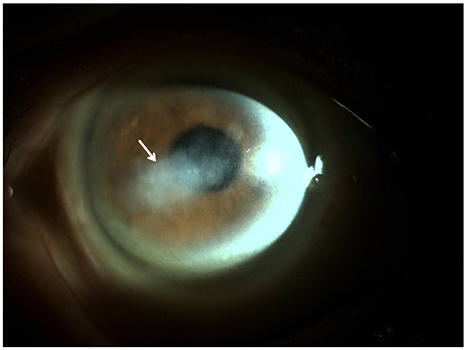
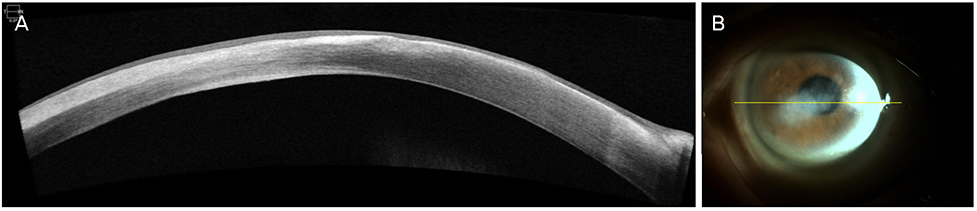
A 77-year-old male had decreased visual acuity for several days in his right eye. The patient showed severe stromal ring infiltrates with a corneal epithelial defect measuring (5.0 × 7.0 mm), a corneal endothelial plaque, and a hypopyon measuring less than 1.0 mm in height in the anterior chamber of the right eye. There was no abnormal finding in the right eye using B-scan ultrasonography. Before starting treatment, a corneal culture was conducted. The culture tests showed the presence of the Moraxella group. Because the patient was diagnosed with a corneal ulcer caused by the Moraxella group, corneal collagen cross-linking (CXL) was performed. The antimicrobial susceptibility test confirmed that this Moraxella group was sensitive to ceftazidime, so the patient was treated with 5% ceftazidime eye drops and 0.5% moxifloxacin eye drops every 2 hours for 9 months after corneal collagen CXL. The uncorrected visual acuity was 0.1 in the right eye, and there was almost no corneal stromal melting on anterior segment optical coherence tomography.
CONCLUSIONS
This is the first known case of a corneal ulcer, in the Republic of Korea, caused by the Moraxella group and treated with corneal collagen CXL. Corneal collagen CXL should be considered as a surgical treatment for patients who have an impending corneal perforation due to a corneal ulcer because it is a simple procedure and causes fewer serious complications than other treatments.
Keyword
MeSH Terms
Figure
Reference
-
1. Song YY, Bang S, Lee TE, et al. Clinical aspects and treatment outcomes of Moraxella keratitis. J Korean Ophthalmol Soc. 2018; 59:209–216.
Article2. Das S, Constantinou M, Daniell M, Taylor HR. Moraxella keratitis: predisposing factors and clinical review of 95 cases. Br J Ophthalmol. 2006; 90:1236–1238.
Article3. Baum J, Fedukowicz HB, Jordan A. A survey of Moraxella corneal ulcers in a derelict population. Am J Ophthalmol. 1980; 90:476–480.
Article4. Mian SI, Malta JB. Moraxella keratitis: risk factors, presentation, and management. Acta Ophthalmol. 2011; 89:e208–e209.
Article5. Park JY, Suh ES. A case of tectonic lamellar corneal patch graft using acellular cornea in corneal ulcer perforation. J Korean Ophthalmol Soc. 2015; 56:1278–1283.
Article6. Makdoumi K, Mortensen J, Crafoord S. Infectious keratitis treated with corneal crosslinking. Cornea. 2010; 29:1353–1358.
Article7. Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006; 17:356–360.
Article8. Spoerl E, Wollensak G, Seiler T. Increased resistance of crosslinked cornea against enzymatic digestion. Curr Eye Res. 2004; 29:35–40.
Article9. Schilde T, Kohlhaas M, Spoerl E, Pillunat LE. Enzymatic evidence of the depth dependence of stiffening on riboflavin/UVA treated corneas. Ophthalmologe. 2008; 105:165–169.10. Iseli HP, Thiel MA, Hafezi F, et al. Ultraviolet A/riboflavin corneal cross-linking for infectious keratitis associated with corneal melts. Cornea. 2008; 27:590–594.
Article11. Inoue H, Suzuki T, Inoue T, et al. Clinical characteristics and bacteriological profile of Moraxella keratitis. Cornea. 2015; 34:1105–1109.
Article12. Martins SA, Combs JC, Noguera G, et al. Antimicrobial efficacy of riboflavin/UVA combination (365 nm) in vitro for bacterial and fungal isolates: a potential new treatment for infectious keratitis. Invest Ophthalmol Vis Sci. 2008; 49:3402–3408.
Article13. Corbin F 3rd. Pathogen inactivation of blood components: current status and introduction of an approach using riboflavin as a photosensitizer. Int J Hematol. 2002; 76 Suppl 2:253–257.
Article14. Xie L, Zhai H, Shi W. Penetrating keratoplasty for corneal perforations in fungal keratitis. Cornea. 2007; 26:158–162.
Article15. Green M, Chow A, Apel A. Outcomes of combined penetrating keratoplasty and cataract extraction compared with penetrating keratoplasty alone. Clin Exp Ophthalmol. 2007; 35:324–329.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multilayer Collagen Sheet Graft for Corneal Perforation with a Corneal Ulcer
- A supplemental treatment for the corneal ulcer or the other corneal diseases
- Changes in Corneal Keratometry Readings after Corneal Collagen Cross-Linking Using Alcohol in Keratoconus Patients
- Treatment of Chronic Corneal Ulcer with Nd-YAG Laser
- The Effect of Early Amniotic Membrane Transplantation in the Rabbits' Corneal Ulcer by Staphylococcus Epidermidis