Clin Orthop Surg.
2020 Mar;12(1):120-129. 10.4055/cios.2020.12.1.120.
Proteomic Classification and Identification of Proteins Related to Tissue Healing of Platelet-Rich Plasma
- Affiliations
-
- 1Department of Orthopaedic Surgery, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. happynoh@gmail.com
- 2Gachon Medical Research Institute, Gil Medical Center, Gachon University, Incheon, Korea.
- 3Department of Orthopaedic Surgery, The Second Hospital of Jilin University, Changchun, China.
- 4Department of Radiology, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2470060
- DOI: http://doi.org/10.4055/cios.2020.12.1.120
Abstract
- BACKGROUND
Platelet-rich plasma (PRP) is a plasma component of autologous blood containing a high concentration of platelets. PRP is used to promote healing of damaged tissues. However, there are not many studies on the composition and expression patterns of active proteins in PRP. The purpose of this study was to identify unknown factors that contribute to tissue healing by proteomic analysis of proteins in PRP.
METHODS
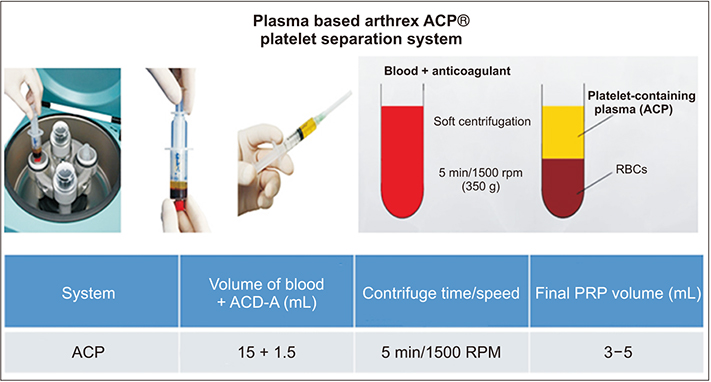
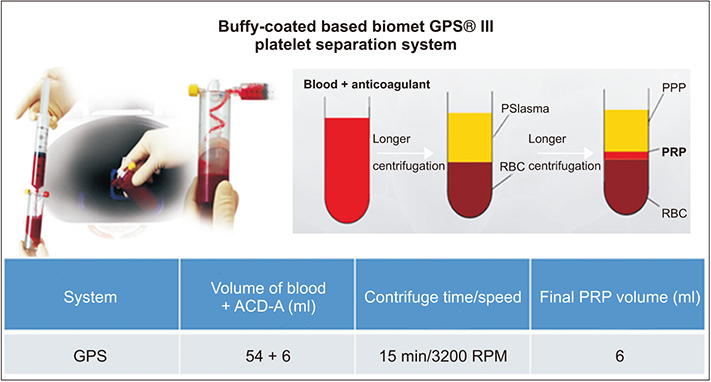
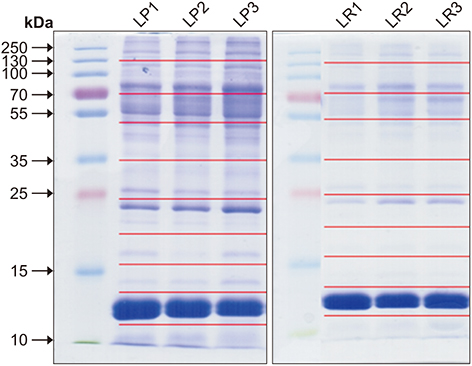
Three men in their 30s with no basal disease participated in this study. All identified proteins were classified for tissue healing-related functions on the basis of the gene ontology analysis of adhesion molecule with Ig-like domain 2 (AmiGO2). PRP was prepared by using the ACP kit and GPS III kit.
RESULTS
We identified a total of 125 proteins related to wound healing, along with three proteins for angiogenesis involved in wound healing, two proteins for fibroblast migration, four proteins for collagen biosynthesis process, two proteins for glycosaminoglycan biosynthesis process, and 13 proteins for glycosaminoglycan binding. So, in addition to the growth factors that have been already known to be involved in tissue healing, 25 new proteins were identified.
CONCLUSIONS
We identified the unknown proteins associated with tissue healing in PRP. Our findings may serve as a foundation for the establishment of basic medical evidence for PRP applications.
Keyword
MeSH Terms
Figure
Reference
-
1. Ferrari M, Zia S, Valbonesi M, et al. A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Organs. 1987; 10(1):47–50.
Article2. Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014; 4(1):3–9.
Article3. de Vos RJ, Weir A, van Schie HT, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA. 2010; 303(2):144–149.
Article4. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009; 37(11):2259–2272.5. Mehta S, Watson JT. Platelet rich concentrate: basic science and current clinical applications. J Orthop Trauma. 2008; 22(6):432–438.
Article6. Harrison P, Cramer EM. Platelet alpha-granules. Blood Rev. 1993; 7(1):52–62.7. Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002; 36(1):39–44.
Article8. Frechette JP, Martineau I, Gagnon G. Platelet-rich plasmas: growth factor content and roles in wound healing. J Dent Res. 2005; 84(5):434–439.
Article9. Marx RE, Armentano L, Olavarria A, Samaniego J. rhBMP-2/ACS grafts versus autogenous cancellous marrow grafts in large vertical defects of the maxilla: an unsponsored randomized open-label clinical trial. Int J Oral Maxillofac Implants. 2013; 28(5):e243–e251.
Article10. Sanchez M, Anitua E, Orive G, Mujika I, Andia I. Platelet-rich therapies in the treatment of orthopaedic sport injuries. Sports Med. 2009; 39(5):345–354.
Article11. Anitua E, Sanchez M, Orive G, Andia I. The potential impact of the preparation rich in growth factors (PRGF) in different medical fields. Biomaterials. 2007; 28(31):4551–4560.
Article12. Schultz G, Rotatori DS, Clark W. EGF and TGF-alpha in wound healing and repair. J Cell Biochem. 1991; 45(4):346–352.13. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004; 91(1):4–15.
Article14. Nissen NN, Polverini PJ, Koch AE, Volin MV, Gamelli RL, DiPietro LA. Vascular endothelial growth factor mediates angiogenic activity during the proliferative phase of wound healing. Am J Pathol. 1998; 152(6):1445–1452.15. Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A. Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991; 45(4):319–326.
Article16. Maynard DM, Heijnen HF, Horne MK, White JG, Gahl WA. Proteomic analysis of platelet alpha-granules using mass spectrometry. J Thromb Haemost. 2007; 5(9):1945–1955.17. Maguire PB, Wynne KJ, Harney DF, O'Donoghue NM, Stephens G, Fitzgerald DJ. Identification of the phosphotyrosine proteome from thrombin activated platelets. Proteomics. 2002; 2(6):642–648.
Article18. Garcia A, Prabhakar S, Hughan S, et al. Differential proteome analysis of TRAP-activated platelets: involvement of DOK-2 and phosphorylation of RGS proteins. Blood. 2004; 103(6):2088–2095.
Article19. Dhurat R, Sukesh M. Principles and methods of preparation of platelet-rich plasma: a review and author's perspective. J Cutan Aesthet Surg. 2014; 7(4):189–197.
Article20. DeLong JM, Russell RP, Mazzocca AD. Platelet-rich plasma: the PAW classification system. Arthroscopy. 2012; 28(7):998–1009.
Article21. McCarrel TM, Minas T, Fortier LA. Optimization of leukocyte concentration in platelet-rich plasma for the treatment of tendinopathy. J Bone Joint Surg Am. 2012; 94(19):e143.
Article22. Harmon KG, Rao AL. The use of platelet-rich plasma in the nonsurgical management of sports injuries: hype or hope? Hematology Am Soc Hematol Educ Program. 2013; 2013:620–626.
Article23. Fitzpatrick J, Bulsara MK, McCrory PR, Richardson MD, Zheng MH. Analysis of platelet-rich plasma extraction: variations in platelet and blood components between 4 common commercial kits. Orthop J Sports Med. 2017; 5(1):2325967116675272.24. Noh KC, Liu XN, Zhuan Z, et al. Leukocyte-poor platelet-rich plasma-derived growth factors enhance human fibroblast proliferation in vitro. Clin Orthop Surg. 2018; 10(2):240–247.
Article25. Carbon S, Ireland A, Mungall CJ, et al. AmiGO: online access to ontology and annotation data. Bioinformatics. 2009; 25(2):288–289.
Article26. Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res. 2006; 17(2):212–219.
Article27. O'Neill EE, Brock CJ, von Kriegsheim AF, et al. Towards complete analysis of the platelet proteome. Proteomics. 2002; 2(3):288–305.28. Moebius J, Zahedi RP, Lewandrowski U, Berger C, Walter U, Sickmann A. The human platelet membrane proteome reveals several new potential membrane proteins. Mol Cell Proteomics. 2005; 4(11):1754–1761.
Article29. Domon B, Aebersold R. Mass spectrometry and protein analysis. Science. 2006; 312(5771):212–217.
Article30. Tabb DL, McDonald WH, Yates JR 3rd. DTASelect and Contrast: tools for assembling and comparing protein identifications from shotgun proteomics. J Proteome Res. 2002; 1(1):21–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats
- Platelet-rich plasma: a healing virtuoso
- Platelet-rich plasma, platelet derivatives, and their therapeutic importance in veterinary medicine
- Platelet-Rich Plasma Injection
- Acceleration of Wound Healing Using Adipose-derived Stem Cell Therapy with Platelet Concentrates: Platelet-rich Plasma (PRP) vs. Platelet-rich Fibrin (PRF)