Is renal replacement therapy necessary in deceased donor liver transplantation candidates with hepatorenal syndrome?: a 2-year experience at a high-volume center
- Affiliations
-
- 1Division of Liver Transplantation and Hepatobiliary Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2469110
- DOI: http://doi.org/10.4174/astr.2020.98.2.102
Abstract
- PURPOSE
Hepatorenal syndrome (HRS) is a fatal complication in patients with end-stage liver disease awaiting liver transplantation (LT). HRS often develops in patients with high model for end-stage liver disease (MELD) score. This study investigated the outcomes of peritransplant management of HRS in a high-volume LT center in Korea for 2 years.
METHODS
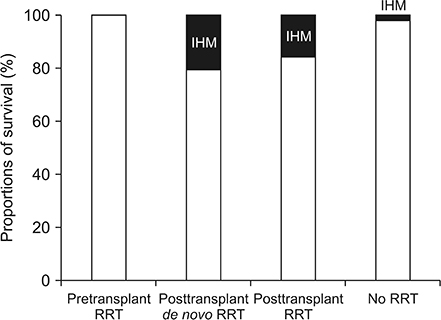
A total of 157 recipients that deceased donor liver transplantation (DDLT) from January 2017 to December 2018 were included. In-hospital mortality (IHM) was analyzed in relation to pre- and posttransplant application of renal replacement therapy (RRT).
RESULTS
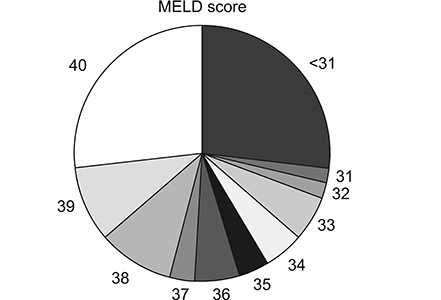
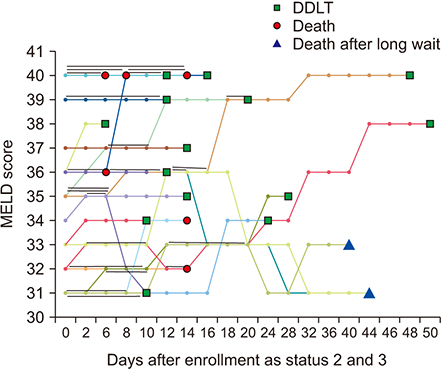
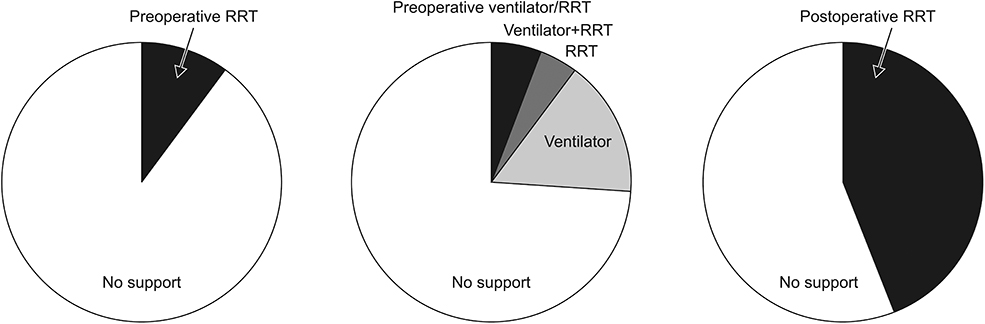
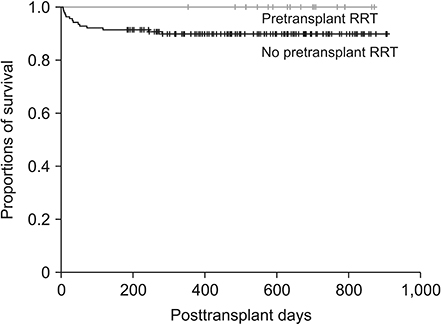
Primary diagnoses for DDLT were alcoholic liver disease (n = 61), HBV-associated liver cirrhosis (n = 48), retransplantation for chronic graft failure (n = 24), and others (n = 24). Mean MELD score was 34.6 ± 6.2 with 72 patients at Korean Network for Organ Sharing MELD status 2 (45.9%), 43 at status 3 (27.4%), 36 at status 4 (22.9%), and 6 at status 5 (3.8%). Pretransplant RRT was performed in 16 patients (10.2%) that did not show IHM. Posttransplant RRT was performed in 69 patients (44.0%), for whom IHM incidence was 15.9%. In 53 patients that had undergone de novo posttransplant RRT, IHM incidence increased to 20.8%. IHM in the 88 patients not requiring RRT was 2.3%.
CONCLUSION
The majority of adult DDLT recipients in Korean MELD score-based allocation system have very high MELD scores, which is often associated with HRS. Pretransplant RRT appears to improve posttransplant survival outcomes. We thereby recommend that, if indicated, pretransplant RRT be performed while awaiting DDLT.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Prognosis of Split Liver Transplantation Compared with Whole Liver Transplantation in Adult Patients: Single-center Results under the Korean MELD Score-based Allocation Policy
Gil-Chun Park, Shin Hwang, Gi-Won Song, Dong-Hwan Jung, Tae-Yong Ha, Chul-Soo Ahn, Deok-Bog Moon, Ki-Hun Kim, Young-In Yoon, Woo-Hyoung Kang, Hwui-Dong Cho, Jin Uk Choi, Minjae Kim, Byeong-Gon Na, Sang Hoon Kim, Sung-Gyu Lee
J Korean Med Sci. 2020;35(37):e304. doi: 10.3346/jkms.2020.35.e304.The impact of Model for End-Stage Liver Disease score on deceased donor liver transplant outcomes in low volume liver transplantation center: a retrospective and single-center study
Doo-Ho Lee, Yeon Ho Park, Seok Won Choi, Kug Hyun Nam, Sang Tae Choi, Doojin Kim
Ann Surg Treat Res. 2021;101(6):360-367. doi: 10.4174/astr.2021.101.6.360.
Reference
-
1. Bollinger RR, Cho WH. Organ allocation for transplantation in the USA and Korea: the changing roles of equity and utility. Yonsei Med J. 2004; 45:1035–1042.
Article2. Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, Song GW, et al. Survival rates among patients awaiting deceased donor liver transplants at a single high-volume Korean center. Transplant Proc. 2013; 45:2995–2996.
Article3. Min SI, Ahn C, Han DJ, Kim SI, Chung SY, Lee SK, et al. To achieve national self-sufficiency: recent progresses in deceased donation in Korea. Transplantation. 2015; 99:765–770.4. Lee SG, Moon DB, Hwang S, Ahn CS, Kim KH, Song GW, et al. Liver transplantation in Korea: past, present, and future. Transplant Proc. 2015; 47:705–708.
Article5. Jung BH, Hwang S, Song GW, Jung DH, Ha TY, Park GC, et al. Updated status of deceased-donor liver graft allocation for high-urgency adult patients in a Korean high-volume liver transplantation center. Transplant Proc. 2015; 47:580–583.
Article6. Ha SM, Hwang S, Song GW, Ahn CS, Moon DB, Ha TY, et al. Successful introduction of Model for End-stage Liver Disease scoring in deceased donor liver transplantation in Korea: analysis of first 1 year experience at a high-volume transplantation center. Ann Hepatobiliary Pancreat Surg. 2017; 21:199–204.
Article7. Francoz C, Durand F, Kahn JA, Genyk YS, Nadim MK. Hepatorenal syndrome. Clin J Am Soc Nephrol. 2019; 14:774–781.
Article8. Salerno F, Gerbes A, Gines P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007; 56:1310–1318.
Article9. Alessandria C, Ozdogan O, Guevara M, Restuccia T, Jimenez W, Arroyo V, et al. MELD score and clinical type predict prognosis in hepatorenal syndrome: relevance to liver transplantation. Hepatology. 2005; 41:1282–1289.
Article10. Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology. 2008; 48:2064–2077.
Article11. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004; 8:R204–R212.12. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11:R31.
Article13. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012; 120:c179–c184.
Article14. Angeli P, Gines P, Wong F, Bernardi M, Boyer TD, Gerbes A, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. Gut. 2015; 64:531–537.
Article15. Sagi SV, Mittal S, Kasturi KS, Sood GK. Terlipressin therapy for reversal of type 1 hepatorenal syndrome: a meta-analysis of randomized controlled trials. J Gastroenterol Hepatol. 2010; 25:880–885.
Article16. Boyer TD, Sanyal AJ, Garcia-Tsao G, Blei A, Carl D, Bexon AS, et al. Predictors of response to terlipressin plus albumin in hepatorenal syndrome (HRS) type 1: relationship of serum creatinine to hemodynamics. J Hepatol. 2011; 55:315–321.
Article17. AlEnezi F, Alhazzani W, Ma J, Alanazi S, Salib M, Attia M, et al. Continuous venovenous hemofiltration versus continuous venovenous hemodiafiltration in critically ill patients: a retrospective cohort study from a Canadian tertiary centre. Can Respir J. 2014; 21:176–180.
Article18. Agopian VG, Dhillon A, Baber J, Kaldas FM, Zarrinpar A, Farmer DG, et al. Liver transplantation in recipients receiving renal replacement therapy: outcomes analysis and the role of intraoperative hemodialysis. Am J Transplant. 2014; 14:1638–1647.
Article19. Matuszkiewicz-Rowinska J, Wieliczko M, MaXMLLink_XYZyszko J. Renal replacement therapy before, during, and after orthotopic liver transplantation. Ann Transplant. 2013; 18:248–255.
Article20. Korean Association for the Study of the Liver. KASL clinical practice guidelines: management of chronic hepatitis B. Clin Mol Hepatol. 2016; 22:18–75.21. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. Toward more than 400 liver transplantations a year at a single center. Transplant Proc. 2013; 45:1937–1941.
Article22. Massie AB, Luo X, Alejo JL, Poon AK, Cameron AM, Segev DL. Higher mortality in registrants with sudden model for end-stage liver disease increase: disadvantaged by the current allocation policy. Liver Transpl. 2015; 21:683–689.
Article23. Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996; 183:949–958.
Article24. Jones CH, Richardson D, Goutcher E, Newstead CG, Will EJ, Cohen AT, et al. Continuous venovenous high-flux dialysis in multiorgan failure: a 5-year single-center experience. Am J Kidney Dis. 1998; 31:227–233.25. Cordoba J, Blei AT, Mujais S. Determinants of ammonia clearance by hemodialysis. Artif Organs. 1996; 20:800–803.
Article26. Thorat A, Jeng LB. Management of renal dysfunction in patients with liver cirrhosis: role of pretransplantation hemodialysis and outcomes after liver transplantation. Semin Vasc Surg. 2016; 29:227–235.
Article27. Gonwa TA, Klintmalm GB, Levy M, Jennings LS, Goldstein RM, Husberg BS. Impact of pretransplant renal function on survival after liver transplantation. Transplantation. 1995; 59:361–365.
Article28. Vitin A, Muczynski K, Bakthavatsalam R, Martay K, Dembo G, Metzner J. Treatment of severe lactic acidosis during the pre-anhepatic stage of liver transplant surgery with intraoperative hemodialysis. J Clin Anesth. 2010; 22:466–472.
Article29. Townsend DR, Bagshaw SM, Jacka MJ, Bigam D, Cave D, Gibney RT. Intraoperative renal support during liver transplantation. Liver Transpl. 2009; 15:73–78.
Article