J Cardiovasc Imaging.
2019 Oct;27(4):257-265. 10.4250/jcvi.2019.27.e36.
Improvement of Left Ventricular Ejection Fraction and Pulmonary Hypertension Are Significant Prognostic Factors in Heart Failure with Reduced Ejection Fraction Patients
- Affiliations
-
- 1Department of Cardiology in Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea. jaehpark@cnu.ac.kr
- 2Department of Cardiology, Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2468352
- DOI: http://doi.org/10.4250/jcvi.2019.27.e36
Abstract
- BACKGROUND
We evaluated long-term prognosis according to improvement of pulmonary hypertension (PH) and left ventricular ejection fraction (LVEF) in patients with heart failure with reduced ejection fraction (HFrEF) and PH.
METHODS
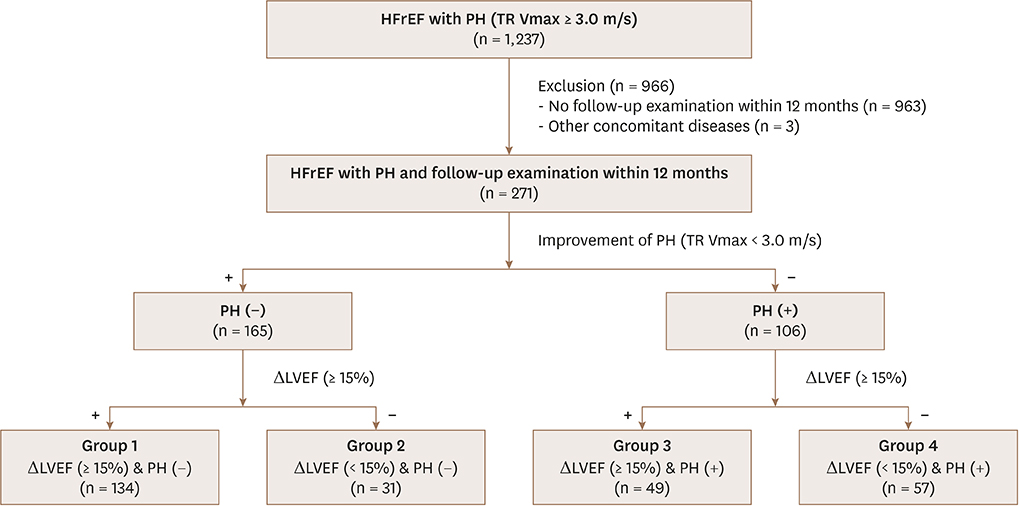
We included all consecutive patients with HFrEF and PH who had a baseline and follow-up echocardiographic examinations from September 2011 to March 2017. PH was defined as maximal velocity of tricuspid regurgitation (TR Vmax) over 3.0 m/s, and LVEF improvement was defined as LVEF change ≥ 15% from the baseline echocardiography. Primary outcome was 5-year major adverse cardio-cerebrovascular events (MACCE).
RESULTS
We analyzed 271 patients. Mean LVEF was 28±8% and TR Vmax was 3.4±0.4 m/s. On follow-up, 183 (68%) showed improvement of LVEF, and 165 (61%) demonstrated improvement of PH. We classified patients into 4 groups according to improvement of PH and LVEF; group 1 (both improvement, 134 patients), group 2 (PH improvement only, 31 patients), group 3 (LVEF improvement only, 49 patients) and group 4 (no improvement, 57 patients). Group 4 had older age, higher incidence of myocardial infarction and aggravation of pre-existing HF. During the follow-up (31±20 months), 27% died and 40.8% experienced MACCE. Group 4 had the worst survival (HR=4.332, 95% CI=2.396-7.833, p<0.001), and group 3 had increased MACCE rate (HR=2.030, 95% CI=1.060-3.888, p=0.033) compared with group 1. Group 2 had similar long-term clinical events (HR=1.085, 95% CI=0.458-2.571, p=0.853) to group 1.
CONCLUSIONS
In patients with HFrEF and PH, persistence of PH and no LVEF improvement was associated with the worst long-term outcome.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prognostic Implications of Changes in Left Ventricular Ejection Fraction and Pulmonary Hypertension in Patients with Heart Failure with Reduced Ejection Fraction
Hyun-Jin Kim
J Cardiovasc Imaging. 2019;27(4):266-267. doi: 10.4250/jcvi.2019.27.e41.
Reference
-
1. Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016; 37:67–119.2. Chung K, Strange G, Codde J, Celermajer D, Scalia GM, Playford D. Left heart disease and pulmonary hypertension: are we seeing the full picture? Heart Lung Circ. 2018; 27:301–309.
Article3. Georgiopoulou VV, Kalogeropoulos AP, Borlaug BA, Gheorghiade M, Butler J. Left ventricular dysfunction with pulmonary hypertension: part 1: epidemiology, pathophysiology, and definitions. Circ Heart Fail. 2013; 6:344–354.4. Kjaergaard J, Akkan D, Iversen KK, et al. Prognostic importance of pulmonary hypertension in patients with heart failure. Am J Cardiol. 2007; 99:1146–1150.
Article5. Grigioni F, Potena L, Galiè N, et al. Prognostic implications of serial assessments of pulmonary hypertension in severe chronic heart failure. J Heart Lung Transplant. 2006; 25:1241–1246.
Article6. Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiéry JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016; 37:942–954.
Article7. Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013; 62:D34–41.
Article8. Bursi F, McNallan SM, Redfield MM, et al. Pulmonary pressures and death in heart failure: a community study. J Am Coll Cardiol. 2012; 59:222–231.9. Aronson D, Eitan A, Dragu R, Burger AJ. Relationship between reactive pulmonary hypertension and mortality in patients with acute decompensated heart failure. Circ Heart Fail. 2011; 4:644–650.
Article10. Cappola TP, Felker GM, Kao WH, Hare JM, Baughman KL, Kasper EK. Pulmonary hypertension and risk of death in cardiomyopathy: patients with myocarditis are at higher risk. Circulation. 2002; 105:1663–1668.11. Kalogeropoulos AP, Siwamogsatham S, Hayek S, et al. Echocardiographic assessment of pulmonary artery systolic pressure and outcomes in ambulatory heart failure patients. J Am Heart Assoc. 2014; 3:e000363.
Article12. Merlos P, Núñez J, Sanchis J, et al. Echocardiographic estimation of pulmonary arterial systolic pressure in acute heart failure. Prognostic implications. Eur J Intern Med. 2013; 24:562–567.
Article13. Santas E, de la Espriella-Juan R, Mollar A, et al. Echocardiographic pulmonary artery pressure estimation and heart failure rehospitalization burden in patients with acute heart failure. Int J Cardiol. 2017; 241:407–410.
Article14. Lupón J, Díez-López C, de Antonio M, et al. Recovered heart failure with reduced ejection fraction and outcomes: a prospective study. Eur J Heart Fail. 2017; 19:1615–1623.
Article15. Le Jemtel TH, Alt EU. Are hemodynamic goals viable in tailoring heart failure therapy? Hemodynamic goals are outdated. Circulation. 2006; 113:1027–1032. discussion 1033.16. Kalogeropoulos AP, Georgiopoulou VV, Borlaug BA, Gheorghiade M, Butler J. Left ventricular dysfunction with pulmonary hypertension: part 2: prognosis, noninvasive evaluation, treatment, and future research. Circ Heart Fail. 2013; 6:584–593.17. Damy T, Goode KM, Kallvikbacka-Bennett A, et al. Determinants and prognostic value of pulmonary arterial pressure in patients with chronic heart failure. Eur Heart J. 2010; 31:2280–2290.
Article18. Santas E, Chorro FJ, Miñana G, et al. Tricuspid regurgitation and mortality risk across left ventricular systolic function in acute heart failure. Circ J. 2015; 79:1526–1533.
Article19. Shalaby A, Voigt A, El-Saed A, Saba S. Usefulness of pulmonary artery pressure by echocardiography to predict outcome in patients receiving cardiac resynchronization therapy heart failure. Am J Cardiol. 2008; 101:238–241.
Article20. Delgado JF, Conde E, Sánchez V, et al. Pulmonary vascular remodeling in pulmonary hypertension due to chronic heart failure. Eur J Heart Fail. 2005; 7:1011–1016.
Article21. Hoeper MM, Lee SH, Voswinckel R, et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol. 2006; 48:2546–2552.
Article22. Sciomer S, Magrì D, Badagliacca R. Non-invasive assessment of pulmonary hypertension: Doppler-echocardiography. Pulm Pharmacol Ther. 2007; 20:135–140.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Implications of Changes in Left Ventricular Ejection Fraction and Pulmonary Hypertension in Patients with Heart Failure with Reduced Ejection Fraction
- Total intravenous anesthesia using remimazolam for patients with heart failure with reduced ejection fraction: a case series
- Evaluation of Ejection Fraction Obtained by Echocardiography and Radionuclide Ventriculography
- Comparisons of the Left Ventricular Ejection Fraction Between M-Mode, Two-Dimension Echocardiographic Studies and Digital Cardiac Imaging(DCI) System in Ventricular Septal Defects*
- Heart failure with preserved ejection fraction: insights from recent clinical researches