J Korean Med Sci.
2016 Oct;31(10):1604-1610. 10.3346/jkms.2016.31.10.1604.
The Prescription Pattern of Acetaminophen and Non-Steroidal Anti-Inflammatory Drugs in Patients with Liver Cirrhosis
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine Pusan National University, Liver Center, Research Institute of Convergence for Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea. mcho@pusan.ac.kr
- 2Digestive Disease Center, Pusan National University Hospital, Busan, Korea.
- 3Research and Statistical Support, Research Institute of Convergence for Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2468251
- DOI: http://doi.org/10.3346/jkms.2016.31.10.1604
Abstract
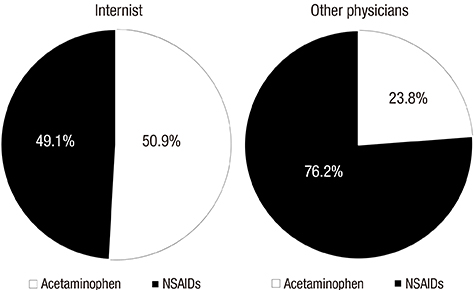
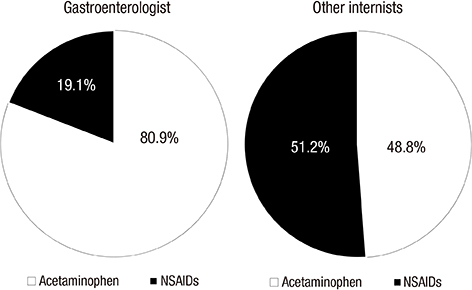
- Analgesics, known to be hepatotoxic drugs, are frequently prescribed to patients with liver cirrhosis who are prone to drug-induced liver injury. No guidelines are available regarding the prescription of analgesics in these patients. Therefore, we aimed to evaluate the prescription pattern of most frequently used analgesics in patients with cirrhosis. We assessed the prescription pattern of acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) in patients with liver cirrhosis registered in Health Insurance Review Assessment Service database between January 1, 2012 and December 31, 2012. A total of 125,505 patients with liver cirrhosis were registered from January 1, 2012 to December 31, 2012. Of that group, 50,798 (40.5%) patients claimed reimbursement for at least one prescription for acetaminophen or NSAIDs during the one year follow-up period. Overall, NSAIDs (82.7%) were more prescribed than acetaminophen (64.5%). NSAIDs were more prescribed than acetaminophen even in decompensated cirrhosis compared with compensated cirrhosis (71.5% vs. 68.8%, P value < 0.001). There was a marked difference in prescription preference between acetaminophen and NSAIDs among physicians. Internists more frequently prescribed acetaminophen than NSAIDs compared to other physicians (50.9% vs. 76.2%, P < 0.001). Gastroenterologists more frequently prescribed acetaminophen over NSAIDs compared to other internists (80.9% vs. 51.2%, P < 0.001). Analgesics were prescribed in 40.5% of patients with cirrhosis. NSAIDs were more frequently prescribed although they should be avoided. The prescription pattern of analgesics were different significantly among physicians in patients with liver cirrhosis. The harmful effects of NSAIDs in patients with cirrhosis should be reminded to all physicians prescribing analgesics.
Keyword
MeSH Terms
-
Acetaminophen/adverse effects/*therapeutic use
Aged
Analgesics/adverse effects/*therapeutic use
Anti-Inflammatory Agents, Non-Steroidal/adverse effects/*therapeutic use
Chemical and Drug Induced Liver Injury/etiology
Databases, Factual
Drug Prescriptions/*statistics & numerical data
Female
Hepatitis, Viral, Human/complications
Humans
Liver Cirrhosis/complications/*diagnosis
Male
Middle Aged
Registries
Analgesics
Anti-Inflammatory Agents, Non-Steroidal
Acetaminophen
Figure
Reference
-
1. Heard K, Green JL, Bailey JE, Bogdan GM, Dart RC. A randomized trial to determine the change in alanine aminotransferase during 10 days of paracetamol (acetaminophen) administration in subjects who consume moderate amounts of alcohol. Aliment Pharmacol Ther. 2007; 26:283–290.2. Dwyer JP, Jayasekera C, Nicoll A. Analgesia for the cirrhotic patient: a literature review and recommendations. J Gastroenterol Hepatol. 2014; 29:1356–1360.3. Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis - a practical guide. Aliment Pharmacol Ther. 2013; 37:1132–1156.4. Imani F, Motavaf M, Safari S, Alavian SM. The therapeutic use of analgesics in patients with liver cirrhosis: a literature review and evidence-based recommendations. Hepat Mon. 2014; 14:e23539.5. Rossi S, Assis DN, Awsare M, Brunner M, Skole K, Rai J, Andrel J, Herrine SK, Reddy RK, Navarro VJ. Use of over-the-counter analgesics in patients with chronic liver disease: physicians’ recommendations. Drug Saf. 2008; 31:261–270.6. Khalid SK, Lane J, Navarro V, Garcia-Tsao G. Use of over-the-counter analgesics is not associated with acute decompensation in patients with cirrhosis. Clin Gastroenterol Hepatol. 2009; 7:994–999.7. WHO Collaborating Center for Drug Statistics Methodology. Defined daily dose: definition and general considerations. accessed on 1 January 2016. Available at http://www.whocc.no/ddd/definition_and_general_considera/.8. D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006; 44:217–231.9. Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, Gustot T, Saliba F, Domenicali M, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013; 144:1426–1437. 1437.e1–1437.e9.10. Zimmerman HJ, Maddrey WC. Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: analysis of instances of therapeutic misadventure. Hepatology. 1995; 22:767–773.11. Lucena MI, Andrade RJ, Tognoni G, Hidalgo R, Sanchez de la Cuesta F; Spanish Collaborative Study Group on Therapeutic Management of Liver Diseases. Drug use for non-hepatic associated conditions in patients with liver cirrhosis. Eur J Clin Pharmacol. 2003; 59:71–76.12. Watkins PB, Kaplowitz N, Slattery JT, Colonese CR, Colucci SV, Stewart PW, Harris SC. Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA. 2006; 296:87–93.13. Schoene B, Fleischmann RA, Remmer H, von Oldershausen HF. Determination of drug metabolizing enzymes in needle biopsies of human liver. Eur J Clin Pharmacol. 1972; 4:65–73.14. Williams RL, Upton RA, Cello JP, Jones RM, Blitstein M, Kelly J, Nierenburg D. Naproxen disposition in patients with alcoholic cirrhosis. Eur J Clin Pharmacol. 1984; 27:291–296.15. Carson JL, Strom BL, Duff A, Gupta A, Das K. Safety of nonsteroidal anti-inflammatory drugs with respect to acute liver disease. Arch Intern Med. 1993; 153:1331–1336.16. Fry SW, Seeff LB. Hepatotoxicity of analgesics and anti-inflammatory agents. Gastroenterol Clin North Am. 1995; 24:875–905.17. Mirouze D, Zipser RD, Reynolds TB. Effect of inhibitors of prostaglandin synthesis on induced diuresis in cirrhosis. Hepatology. 1983; 3:50–55.18. Boyer TD, Zia P, Reynolds TB. Effect of indomethacin and prostaglandin A1 on renal function and plasma renin activity in alcoholic liver disease. Gastroenterology. 1979; 77:215–222.19. Schafer AI. Effects of nonsteroidal antiinflammatory drugs on platelet function and systemic hemostasis. J Clin Pharmacol. 1995; 35:209–219.20. Brater DC, Anderson SA, Brown-Cartwright D. Reversible acute decrease in renal function by NSAIDs in cirrhosis. Am J Med Sci. 1987; 294:168–174.21. Clària J, Kent JD, López-Parra M, Escolar G, Ruiz-Del-Arbol L, Ginès P, Jiménez W, Vucelic B, Arroyo V. Effects of celecoxib and naproxen on renal function in nonazotemic patients with cirrhosis and ascites. Hepatology. 2005; 41:579–587.22. Lee YC, Chang CH, Lin JW, Chen HC, Lin MS, Lai MS. Non-steroidal anti-inflammatory drugs use and risk of upper gastrointestinal adverse events in cirrhotic patients. Liver Int. 2012; 32:859–866.23. Luo JC, Leu HB, Hou MC, Huang CC, Lin HC, Lee FY, Chang FY, Chan WL, Lin SJ, Chen JW. Cirrhotic patients at increased risk of peptic ulcer bleeding: a nationwide population-based cohort study. Aliment Pharmacol Ther. 2012; 36:542–550.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four Cases of Drug Allergy Caused by Non-Steroidal Anti-Inflammatory Drugs in Children
- Changes in Toxicological Characteristics after Sales of Nonprescription Drugs in Convenience Stores
- Cancer Pain Management-Nonopoid Analgesics
- A Comparison of the Efficacy and Safety of Non-Steroidal Anti-Inflammatory Drugs versus Acetaminophen in Symptom Relief for the Common Cold: A Meta-Analysis of Randomized Controlled Trial Studies
- A case of acetaminophen anaphylaxis without aspirin sensitivity