Korean J Radiol.
2019 Jul;20(7):1195-1206. 10.3348/kjr.2018.0893.
Accuracy of Model-Based Iterative Reconstruction for CT Volumetry of Part-Solid Nodules and Solid Nodules in Comparison with Filtered Back Projection and Hybrid Iterative Reconstruction at Various Dose Settings: An Anthropomorphic Chest Phantom Study
- Affiliations
-
- 1Department of Radiology, Ansan Hospital, Korea University College of Medicine, Ansan, Korea. kiylee@korea.ac.kr
- 2Medical Science Research Center, Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- 3Department of Radiology, National Cancer Center, Goyang, Korea.
- 4Department of Radiology, Korea University Guro Hospital, College of Medicine Korea University, Seoul, Korea.
- 5Department of Radiology, Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 2467030
- DOI: http://doi.org/10.3348/kjr.2018.0893
Abstract
OBJECTIVE
To investigate the accuracy of model-based iterative reconstruction (MIR) for volume measurement of part-solid nodules (PSNs) and solid nodules (SNs) in comparison with filtered back projection (FBP) or hybrid iterative reconstruction (HIR) at various radiation dose settings.
MATERIALS AND METHODS
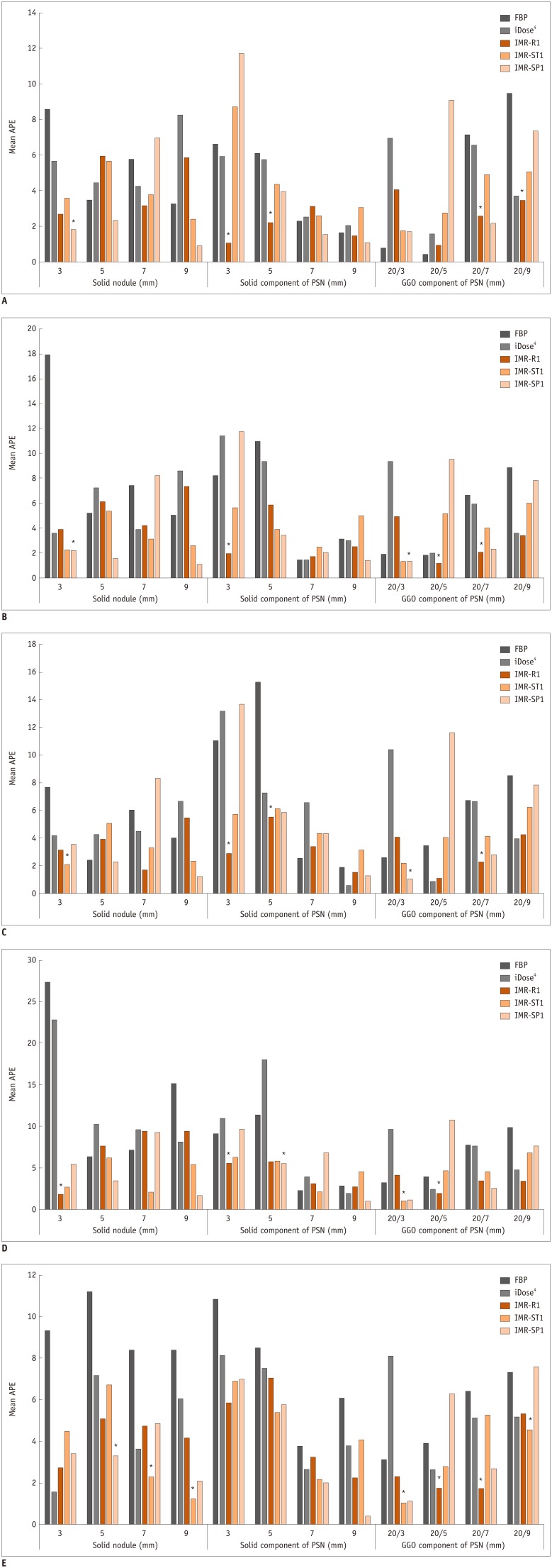
CT scanning was performed for eight different diameters of PSNs and SNs placed in the phantom at five radiation dose levels (120 kVp/100 mAs, 120 kVp/50 mAs, 120 kVp/20 mAs, 120 kVp/10 mAs, and 80 kVp/10 mAs). Each CT scan was reconstructed using FBP, HIR, or MIR with three different image definitions (body routine level 1 [IMR-R1], body soft tissue level 1 [IMR-ST1], and sharp plus level 1 [IMR-SP1]; Philips Healthcare). The SN and PSN volumes including each solid/ground-glass opacity portion were measured semi-automatically, after which absolute percentage measurement errors (APEs) of the measured volumes were calculated. Image noise was calculated to assess the image quality.
RESULTS
Across all nodules and dose settings, the APEs were significantly lower in MIR than in FBP and HIR (all p < 0.01). The APEs of the smallest inner solid portion of the PSNs (3 mm) and SNs (3 mm) were the lowest when MIR (IMR-R1 and IMR-ST1) was used for reconstruction for all radiation dose settings. (IMR-R1 and IMR-ST1 at 120 kVp/100 mAs, 1.06 ± 1.36 and 8.75 ± 3.96, p < 0.001; at 120 kVp/50 mAs, 1.95 ± 1.56 and 5.61 ± 0.85, p = 0.002; at 120 kVp/20 mAs, 2.88 ± 3.68 and 5.75 ± 1.95, p = 0.001; at 120 kVp/10 mAs, 5.57 ± 6.26 and 6.32 ± 2.91, p = 0.091; at 80 kVp/10 mAs, 5.84 ± 1.96 and 6.90 ± 3.31, p = 0.632). Image noise was significantly lower in MIR than in FBP and HIR for all radiation dose settings (120 kVp/100 mAs, 3.22 ± 0.66; 120 kVp/50 mAs, 4.19 ± 1.37; 120 kVp/20 mAs, 5.49 ± 1.16; 120 kVp/10 mAs, 6.88 ± 1.91; 80 kVp/10 mAs, 12.49 ± 6.14; all p < 0.001).
CONCLUSION
MIR was the most accurate algorithm for volume measurements of both PSNs and SNs in comparison with FBP and HIR at low-dose as well as standard-dose settings. Specifically, MIR was effective in the volume measurement of the smallest PSNs and SNs.
MeSH Terms
Figure
Cited by 1 articles
-
Advanced Sectioned Images of a Cadaver Head with Voxel Size of 0.04 mm
Beom Sun Chung, Miran Han, Donghwan Har, Jin Seo Park
J Korean Med Sci. 2019;34(34):. doi: 10.3346/jkms.2019.34.e218.
Reference
-
1. National Lung Screening Trial Research Team. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409. PMID: 21714641.
Article2. MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017; 284:228–243. PMID: 28240562.3. Vardhanabhuti V, Loader RJ, Mitchell GR, Riordan RD, Roobottom CA. Image quality assessment of standard- and low-dose chest CT using filtered back projection, adaptive statistical iterative reconstruction, and novel model-based iterative reconstruction algorithms. AJR Am J Roentgenol. 2013; 200:545–552. PMID: 23436843.
Article4. Katsura M, Matsuda I, Akahane M, Sato J, Akai H, Yasaka K, et al. Model-based iterative reconstruction technique for radiation dose reduction in chest CT: comparison with the adaptive statistical iterative reconstruction technique. Eur Radiol. 2012; 22:1613–1623. PMID: 22538629.
Article5. Yuki H, Oda S, Utsunomiya D, Funama Y, Kidoh M, Namimoto T, et al. Clinical impact of model-based type iterative reconstruction with fast reconstruction time on image quality of low-dose screening chest CT. Acta Radiol. 2016; 57:295–302. PMID: 25817455.
Article6. Kim C, Lee KY, Shin C, Kang EY, Oh YW, Ha M, et al. Comparison of filtered back projection, hybrid iterative reconstruction, model-based iterative reconstruction, and virtual monoenergetic reconstruction images at both low- and standard-dose settings in measurement of emphysema volume and airway wall thickness: a CT phantom study. Korean J Radiol. 2018; 19:809–817. PMID: 29962888.
Article7. Gavrielides MA, Berman BP, Supanich M, Schultz K, Li Q, Petrick N, et al. Quantitative assessment of nonsolid pulmonary nodule volume with computed tomography in a phantom study. Quant Imaging Med Surg. 2017; 7:623–635. PMID: 29312867.
Article8. Maruyama S, Fukushima Y, Miyamae Y, Koizumi K. Usefulness of model-based iterative reconstruction in semi-automatic volumetry for ground-glass nodules at ultra-low-dose CT: a phantom study. Radiol Phys Technol. 2018; 11:235–241. PMID: 29429016.
Article9. Chen B, Barnhart H, Richard S, Robins M, Colsher J, Samei E. Volumetric quantification of lung nodules in CT with iterative reconstruction (ASiR and MBIR). Med Phys. 2013; 40:111902. PMID: 24320435.
Article10. Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000; 73:1252–1259. PMID: 11205667.
Article11. Jennings SG, Winer-Muram HT, Tarver RD, Farber MO. Lung tumor growth: assessment with CT--comparison of diameter and cross-sectional area with volume measurements. Radiology. 2004; 231:866–871. PMID: 15163822.
Article12. Kim C, Lee SM, Choe J, Chae EJ, Do KH, Seo JB. Volume doubling time of lung cancer detected in idiopathic interstitial pneumonia: comparison with that in chronic obstructive pulmonary disease. Eur Radiol. 2018; 28:1402–1409. PMID: 29038933.
Article13. Devaraj A, van Ginneken B, Nair A, Baldwin D. Use of volumetry for lung nodule management: theory and practice. Radiology. 2017; 284:630–644. PMID: 28825886.
Article14. Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J, et al. on behalf of the British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax. 2015; 70(Suppl 2):ii1–ii54. PMID: 26082159.15. Cohen JG, Reymond E, Lederlin M, Medici M, Lantuejoul S, Laurent F, et al. Differentiating pre- and minimally invasive from invasive adenocarcinoma using CT-features in persistent pulmonary part-solid nodules in Caucasian patients. Eur J Radiol. 2015; 84:738–744. PMID: 25623825.
Article16. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994; 6:284–290.
Article17. Kim H, Park CM, Song YS, Lee SM, Goo JM. Influence of radiation dose and iterative reconstruction algorithms for measurement accuracy and reproducibility of pulmonary nodule volumetry: a phantom study. Eur J Radiol. 2014; 83:848–857. PMID: 24572380.
Article18. Kim H, Park CM, Chae HD, Lee SM, Goo JM. Impact of radiation dose and iterative reconstruction on pulmonary nodule measurements at chest CT: a phantom study. Diagn Interv Radiol. 2015; 21:459–465. PMID: 26359871.
Article19. Cohen JG, Kim H, Park SB, van Ginneken B, Ferretti GR, Lee CH, et al. Comparison of the effects of model-based iterative reconstruction and filtered back projection algorithms on software measurements in pulmonary subsolid nodules. Eur Radiol. 2017; 27:3266–3274. PMID: 28058482.
Article20. Doo KW, Kang EY, Yong HS, Woo OH, Lee KY, Oh YW. Accuracy of lung nodule volumetry in low-dose CT with iterative reconstruction: an anthropomorphic thoracic phantom study. Br J Radiol. 2014; 87:20130644. PMID: 25026866.
Article21. Willemink MJ, de Jong PA, Leiner T, de Heer LM, Nievelstein RA, Budde RP, et al. Iterative reconstruction techniques for computed tomography Part 1: technical principles. Eur Radiol. 2013; 23:1623–1631. PMID: 23314600.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Filtered Back Projection, Hybrid Iterative Reconstruction, Model-Based Iterative Reconstruction, and Virtual Monoenergetic Reconstruction Images at Both Low- and Standard-Dose Settings in Measurement of Emphysema Volume and Airway Wall Thickness: A CT Phantom Study
- Quantitative Image Quality and Histogram-Based Evaluations of an Iterative Reconstruction Algorithm at Low-to-Ultralow Radiation Dose Levels: A Phantom Study in Chest CT
- Effects of Iterative Reconstruction Algorithm, Automatic Exposure Control on Image Quality, and Radiation Dose: Phantom Experiments with Coronary CT Angiography Protocols
- Effect of Hybrid Kernel and Iterative Reconstruction on Objective and Subjective Analysis of Lung Nodule Calcification in Low-Dose Chest CT
- Contrast-Enhanced CT with Knowledge-Based Iterative Model Reconstruction for the Evaluation of Parotid Gland Tumors: A Feasibility Study