Imaging Sci Dent.
2019 Dec;49(4):317-321. 10.5624/isd.2019.49.4.317.
Steatocystoma multiplex: A case report of a rare entity
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea. hmslsh@snu.ac.kr
- 2Department of Oral and Maxillofacial Radiology, Seoul National University Dental Hospital, Seoul, Korea.
- 3Division of Oral and Maxillofacial Radiology, Department of Basic Science, Faculty of Dentistry, University of Health Sciences, Vientiane, Laos.
- KMID: 2466555
- DOI: http://doi.org/10.5624/isd.2019.49.4.317
Abstract
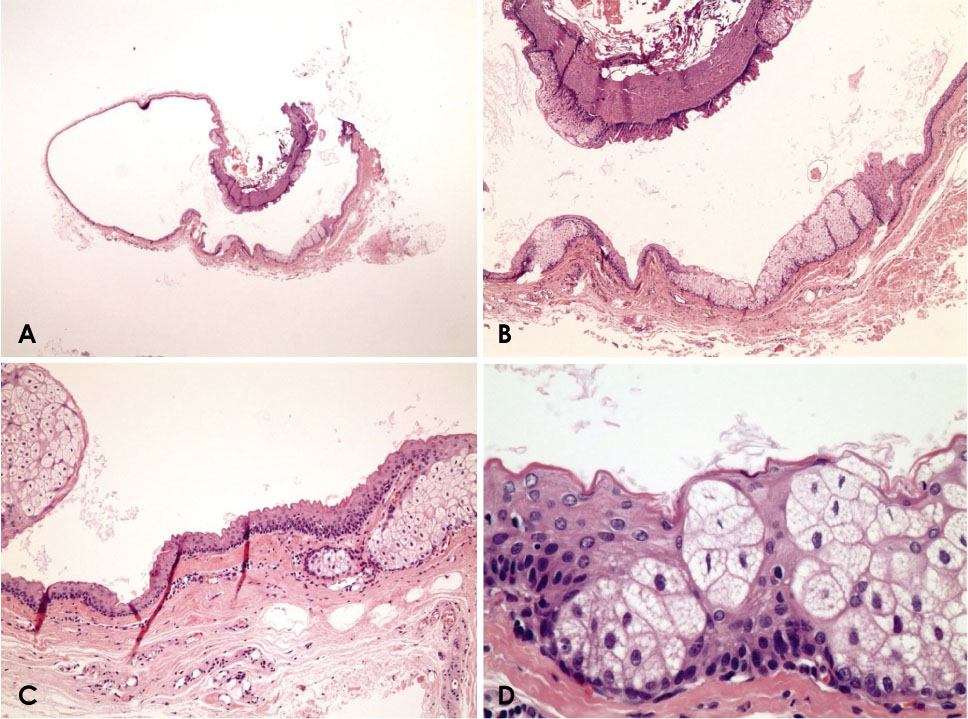
- Steatocystoma multiplex is an uncommon benign skin disease, which typically manifests as numerous intradermal cysts that can be scattered anywhere on the body. Although usually asymptomatic, it can be significantly disfiguring. One type of steatocystoma multiplex is known to be associated with the autosomal dominant inheritance of a mutation in the gene coding for keratin 17 (KRT17). In such cases, it is often concurrent with other developmental abnormalities of the ectoderm-derived tissues, such as the nails, hair, and teeth. To the best of our knowledge, few cases have been reported of steatocystoma multiplex of the oral and maxillofacial region. This report describes a case of steatocystoma multiplex of both sides of the neck and multiple dental anomalies, with a focus on its clinical, radiological, and histopathological characteristics, as well as the possibility that the patient exhibited the familial type of this condition.
MeSH Terms
Figure
Reference
-
1. Plewig G, Wolff HH, Braun-Falco O. Steatocystoma multiplex: anatomic reevaluation, electron microscopy, and autoradiography. Arch Dermatol Res. 1982; 272:363–380.
Article2. Sonnenblick EB, Buchness MR, Austin JH. CT demonstration of steatocystoma multiplex. J Comput Assist Tomogr. 1986; 10:357–359.
Article3. Park YM, Cho SH, Kang H. Congenital linear steatocystoma multiplex of the nose. Pediatr Dermatol. 2000; 17:136–138.4. Marzano AV, Tavecchio S, Balice Y, Polloni I, Veraldi S. Acral subcutaneous steatocystoma multiplex: a distinct subtype of the disease? Australas J Dermatol. 2012; 53:198–201.
Article5. Feinstein A, Friedman J, Schewach-Millet M. Pachyonychia congenita. J Am Acad Dermatol. 1988; 19:705–711.
Article6. Covello SP, Smith FJ, Sillevis Smitt JH, Paller AS, Munro CS, Jonkman MF, et al. Keratin 17 mutations cause either steatocystoma multiplex or pachyonychia congenita type 2. Br J Dermatol. 1998; 139:475–480.
Article7. Jamieson WA. Case of numerous cutaneous cysts scattered over the body. Edinb Med J. 1873; 19:223–225.8. Olsen DB, Mostofi RS, Lagrotteria LB. Steatocystoma simplex in the oral cavity: a previously undescribed condition. Oral Surg Oral Med Oral Pathol. 1988; 66:605–607.
Article9. Kim SJ, Park HJ, Oh ST, Lee JY, Cho BK. A case of steatocystoma multiplex limited to the scalp. Ann Dermatol. 2009; 21:106–109.
Article10. Ohtake N, Kubota Y, Takayama O, Shimada S, Tamaki K. Relationship between steatocystoma multiplex and eruptive vellus hair cysts. J Am Acad Dermatol. 1992; 26:876–878.
Article11. Papakonstantinou E, Franke I, Gollnick H. Facial Steatocystoma multiplex combined with eruptive vellus hair cysts: a hybrid? J Eur Acad Dermatol Venereol. 2015; 29:2051–2053.
Article12. Xiao SX, Feng YG, Ren XR, Tan SS, Li L, Wang JM, et al. A novel mutation in the second half of the keratin 17 1A domain in a large pedigree with delayed-onset pachyonychia congenita type 2. J Invest Dermatol. 2004; 122:892–895.
Article13. Smith FJ, Corden LD, Rugg EL, Ratnavel R, Leigh IM, Moss C, et al. Missense mutations in keratin 17 cause either pachyonychia congenita type 2 or a phenotype resembling steatocystoma multiplex. J Invest Dermatol. 1997; 108:220–223.
Article14. Moon SE, Lee YS, Youn JI. Eruptive vellus hair cyst and steatocystoma multiplex in a patient with pachyonychia congenita. J Am Acad Dermatol. 1994; 30:275–276.
Article15. Leachman SA, Kaspar RL, Fleckman P, Florell SR, Smith FJ, McLean WH, et al. Clinical and pathological features of pachyonychia congenita. J Investig Dermatol Symp Proc. 2005; 10:3–17.
Article16. Oh SW, Kim MY, Lee JS, Kim SC. Keratin 17 mutation in pachyonychia congenita type 2 patient with early onset steatocystoma multiplex and Hutchinson-like tooth deformity. J Dermatol. 2006; 33:161–164.
Article17. Zamiri M, McLean WH, Hodgins MB, Munro CS. Pachyonychia congenita type 2: abnormal dentition extending into adulthood. Br J Dermatol. 2008; 159:500–501.
Article18. Gass JK, Wilson NJ, Smith FJ, Lane EB, Mclean WH, Rytina E, et al. Steatocystoma multiplex, oligodontia and partial persistent primary dentition associated with a novel keratin 17 mutation. Br J Dermatol. 2009; 161:1396–1398.
Article