Intest Res.
2019 Oct;17(4):546-553. 10.5217/ir.2019.00009.
Is fecal calprotectin always normal in children with irritable bowel syndrome?
- Affiliations
-
- 1Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 2Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. jinped@cha.ac.kr
- KMID: 2465820
- DOI: http://doi.org/10.5217/ir.2019.00009
Abstract
- BACKGROUND/AIMS
Fecal calprotectin (FC) is a marker of intraluminal intestinal inflammation. Intestinal inflammation may contribute to the pathophysiology of irritable bowel syndrome (IBS). This study evaluated FC levels in children with IBS and differences in FC levels in children stratified by IBS subtype and healthy controls (HCs).
METHODS
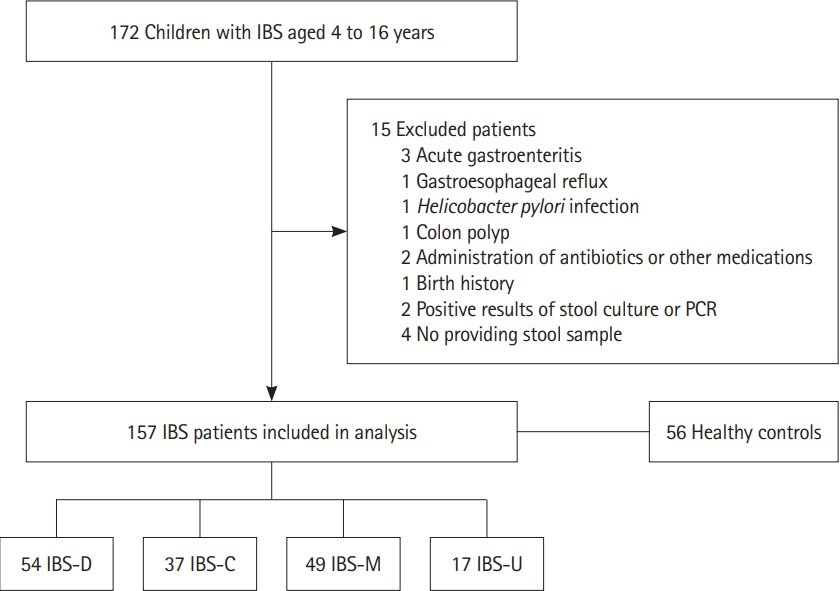
A total of 157 children with IBS and 56 HCs aged 4-16 years (119 boys, 94 girls, mean age of 9.48 years) were included in this prospective study. Children with IBS were diagnosed using the Rome III criteria and classified into 4 subtypes: IBS with constipation (IBS-C, n=37), IBS with diarrhea (IBS-D, n=54), IBS with alternating constipation and diarrhea (IBS-M, n=49), and IBS unsubtyped (IBS-U, n=17); postinfectious IBS (PI-IBS) was also considered. The FC concentration in stool samples was analyzed using an enzyme-linked immunosorbent assay. All participants answered a questionnaire regarding several demographic and clinical characteristics.
RESULTS
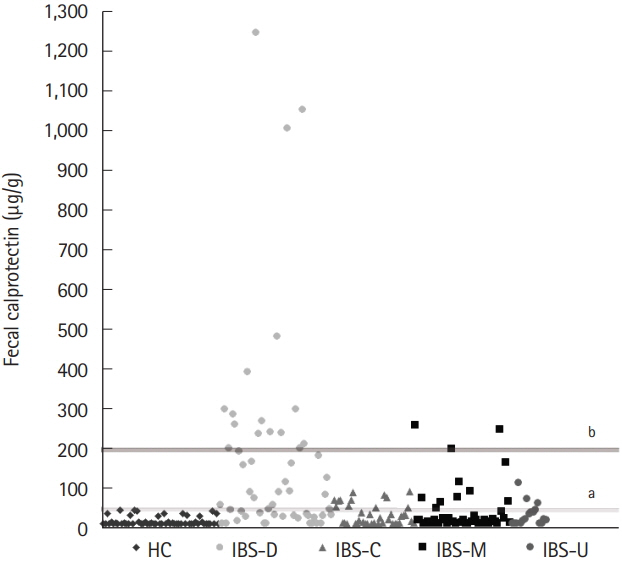
Children with IBS had significantly higher levels of FC than the HCs (88.71 μg/g vs. 17.77 μg/g). Among the 4 IBS subtypes, the FC concentration was highest in children with IBS-D, followed by those with IBS-M, IBS-C, and IBS-U (169.94 μg/g vs. 45.04, 31.22, and 33.52 μg/g, respectively), and these differences were statistically significant. For PI-IBS, 90% of cases were in the IBS-D group.
CONCLUSIONS
The FC level was significantly higher in children with IBS than in HCs and differed depending on the IBS subtype, supporting the notion that IBS is a type of low-grade bowel inflammation.
MeSH Terms
Figure
Reference
-
1. Devanarayana NM, Rajindrajith S, Pathmeswaran A, Abegunasekara C, Gunawardena NK, Benninga MA. Epidemiology of irritable bowel syndrome in children and adolescents in Asia. J Pediatr Gastroenterol Nutr. 2015; 60:792–798.2. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006; 130:1480–1491.
Article3. Abdul Rani R, Raja Ali RA, Lee YY. Irritable bowel syndrome and inflammatory bowel disease overlap syndrome: pieces of the puzzle are falling into place. Intest Res. 2016; 14:297–304.4. von Arnim U, Wex T, Ganzert C, Schulz C, Malfertheiner P. Fecal calprotectin: a marker for clinical differentiation of microscopic colitis and irritable bowel syndrome. Clin Exp Gastroenterol. 2016; 9:97–103.5. Gecse K, Róka R, Ferrier L, et al. Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity. Gut. 2008; 57:591–599.6. Barbara G, Zecchi L, Barbaro R, et al. Mucosal permeability and immune activation as potential therapeutic targets of probiotics in irritable bowel syndrome. J Clin Gastroenterol. 2012; 46:S52–S55.7. Di Nardo G, Barbara G, Cucchiara S, et al. Neuroimmune interactions at different intestinal sites are related to abdominal pain symptoms in children with IBS. Neurogastroenterol Motil. 2014; 26:196–204.
Article8. Saha L. Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol. 2014; 20:6759–6773.
Article9. Keohane J, O’Mahony C, O’Mahony L, O’Mahony S, Quigley EM, Shanahan F. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol. 2010; 105:1788–1794.
Article10. Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009; 136:1979–1988.11. von Roon AC, Karamountzos L, Purkayastha S, et al. Diagnostic precision of fecal calprotectin for inflammatory bowel disease and colorectal malignancy. Am J Gastroenterol. 2007; 102:803–813.12. Menees SB, Powell C, Kurlander J, Goel A, Chey WD. A meta-analysis of the utility of C-reactive protein, erythrocyte sedimentation rate, fecal calprotectin, and fecal lactoferrin to exclude inflammatory bowel disease in adults with IBS. Am J Gastroenterol. 2015; 110:444–454.13. Alibrahim B, Aljasser MI, Salh B. Fecal calprotectin use in inflammatory bowel disease and beyond: a mini-review. Can J Gastroenterol Hepatol. 2015; 29:157–163.
Article14. Schoepfer AM, Trummler M, Seeholzer P, Seibold-Schmid B, Seibold F. Discriminating IBD from IBS: comparison of the test performance of fecal markers, blood leukocytes, CRP, and IBD antibodies. Inflamm Bowel Dis. 2008; 14:32–39.15. Montalto M, Gallo A, Santoro L, D’Onofrio F, Landolfi R, Gasbarrini A. Role of fecal calprotectin in gastrointestinal disorders. Eur Rev Med Pharmacol Sci. 2013; 17:1569–1582.16. Olafsdottir I, Nemeth A, Lörinc E, Toth E, Agardh D. Value of fecal calprotectin as a biomarker for juvenile polyps in children investigated with colonoscopy. J Pediatr Gastroenterol Nutr. 2016; 62:43–46.17. Waugh N, Cummins E, Royle P, et al. Faecal calprotectin testing for differentiating amongst inflammatory and non-inflammatory bowel diseases: systematic review and economic evaluation. Health Technol Assess. 2013; 17:1–211.18. Self MM, Czyzewski DI, Chumpitazi BP, Weidler EM, Shulman RJ. Subtypes of irritable bowel syndrome in children and adolescents. Clin Gastroenterol Hepatol. 2014; 12:1468–1473.
Article19. Labaere D, Smismans A, Van Olmen A, et al. Comparison of six different calprotectin assays for the assessment of inflammatory bowel disease. United European Gastroenterol J. 2014; 2:30–37.20. Melchior C, Aziz M, Aubry T, et al. Does calprotectin level identify a subgroup among patients suffering from irritable bowel syndrome? Results of a prospective study. United European Gastroenterol J. 2017; 5:261–269.21. Marshall JK, Thabane M, Garg AX, et al. Intestinal permeability in patients with irritable bowel syndrome after a waterborne outbreak of acute gastroenteritis in Walkerton, Ontario. Aliment Pharmacol Ther. 2004; 20:1317–1322.22. Jonefjäll B, Strid H, Ohman L, Svedlund J, Bergstedt A, Simren M. Characterization of IBS-like symptoms in patients with ulcerative colitis in clinical remission. Neurogastroenterol Motil. 2013; 25:756–e578.23. Saulnier DM, Riehle K, Mistretta TA, et al. Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome. Gastroenterology. 2011; 141:1782–1791.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of three different fecal calprotectin tests in the diagnosis of inflammatory bowel disease
- The role of fecal calprotectin in pediatric disease
- Alteration of Fecal Microbiota in Patients With Postinfectious Irritable Bowel Syndrome
- Irritable bowel syndrome
- Diarrhea-predominant Irritable Bowel Syndrome-like Symptoms in Patients With Quiescent Crohn’s Disease: Comprehensive Analysis of Clinical Features and Intestinal Environment Including the Gut Microbiome, Organic Acids, and Intestinal Permeability