J Rhinol.
2019 Nov;26(2):106-112. 10.18787/jr.2019.26.2.106.
The Effects of Olfactory Training with Intranasal Corticosteroid Spray in Korean Patients with Olfactory Dysfunction
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, School of Medicine, Catholic University of Daegu, Daegu, Korea. miky@cu.ac.kr
- KMID: 2465542
- DOI: http://doi.org/10.18787/jr.2019.26.2.106
Abstract
- BACKGROUND AND OBJECTIVES
Olfactory training is an alternative treatment based on modulation of the regeneration process of the olfactory system via repeated exposure to odors. Our study aimed to investigate the impact of olfactory training with intranasal corticosteroid in Korean patients with various causes of olfactory dysfunction.
SUBJECTS AND METHOD
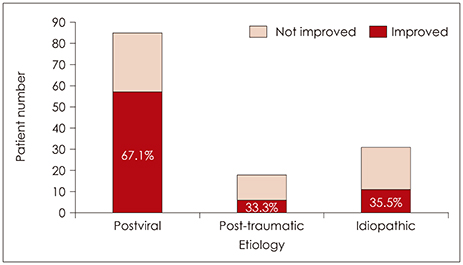
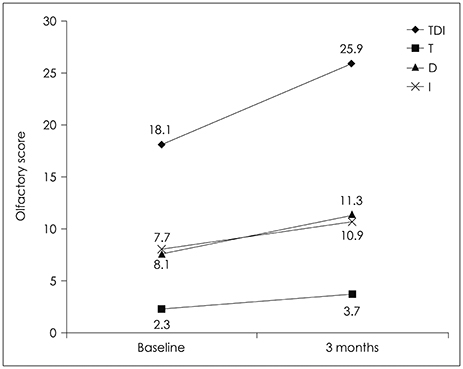
Our study population comprised 134 adults with olfactory dysfunction of different etiologies (postviral infection n=85; post-traumatic n=18; and idiopathic n=31). For training, patients exposed themselves to four different odors twice a day. All patients used fluticasone nasal spray (two sprays in each nostril once daily). Olfactory function was evaluated at baseline and again at three months, and results were quantified as patient TDI (threshold, discrimination, and identification) score
RESULTS
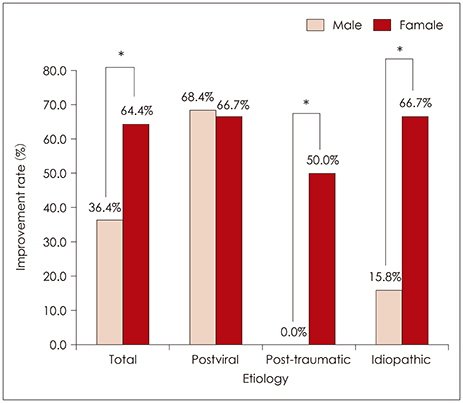
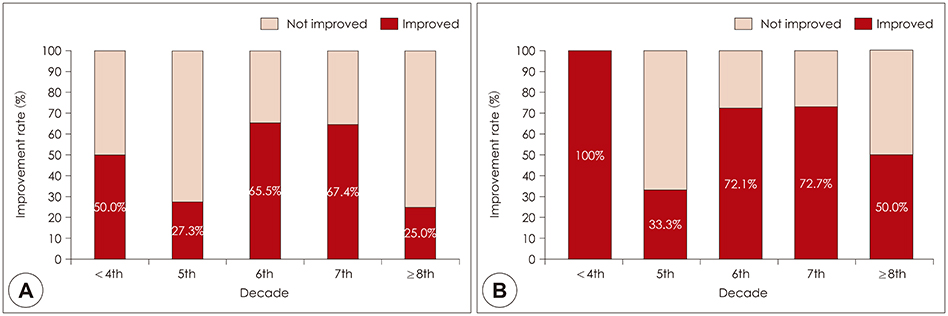
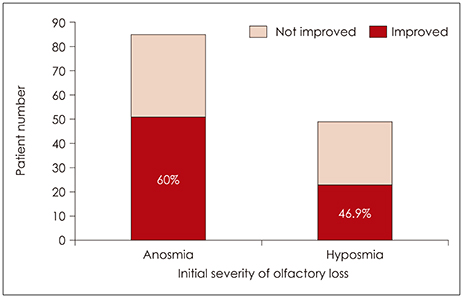
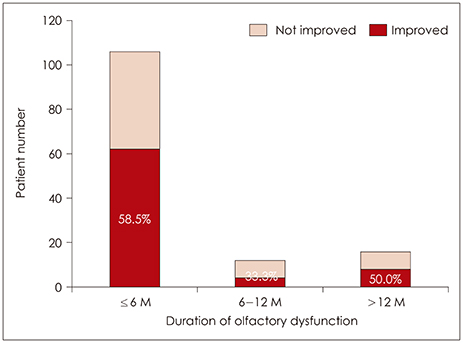
Olfactory function improved in 74 of 134 patients (55.2%). Etiology of olfactory disorder, sex, and age had statistically significant influence on the improvement rate of olfactory function, among which etiology of olfactory loss was the most important. However, initial severity and duration of olfactory loss had no statistically significant influence on the improvement rate. The TDI score at three months of olfactory training showed remarkable improvement, primarily because of improvements in the discrimination and identification components.
CONCLUSION
The present study showed that olfactory training with intranasal corticosteroid was beneficial to improve olfactory function in patients with olfactory dysfunction, particularly in postviral infection patients.
MeSH Terms
Figure
Reference
-
1. Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. Journal of Neurology. 2008; 255(8):1121–1126.
Article2. Murphy C, Schubert CR, Cruickshanks KJ, Klein BE, Klein R, Nondahl DM. Prevalence of olfactory impairment in older adults. JAMA. 2002; 288(18):2307–2312.
Article3. Landis BN, Hummel T. New evidence for high occurrence of olfactory dysfunctions within the population. Am J Med. 2006; 119(1):91–92.
Article4. Nordin S, Bramerson A, Millqvist E, Bende M. Prevalence of parosmia: the Skovde population-based studies. Rhinology. 2007; 45(1):50–53.5. Reden J, Herting B, Lill K, Kern R, Hummel T. Treatment of postinfectious olfactory disorders with minocycline: A double-blind, placebo-controlled study. The Laryngoscope. 2011; 121(3):679–682.
Article6. Hummel T, Rissom K, Reden J, Hahner A, Weidenbecher M, Huttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; 119(3):496–499.
Article7. Fleiner F, Lau L, Goktas O. Active olfactory training for the treatment of smelling disorders. Ear Nose Throat J. 2012; 91(5):198–203.
Article8. Henning H. Der geruch. Leipzig, Germany: Johann Ambrosius Barth;1916.9. Konstantinidis I, Tsakiropoulou E, Bekiaridou P, Kazantzidou C, Constantinidis J. Use of olfactory training in post-traumatic and postinfectious olfactory dysfunction. The Laryngoscope. 2013; 123(12):E85–E90.
Article10. Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2016; 6(3):299–307.
Article11. Wilson DA, Best AR, Sullivan RM. Plasticity in the Olfactory System: Lessons for the Neurobiology of Memory. The Neuroscientist. 2004; 10(6):513–524.
Article12. Damm M, Pikart LK, Reimann H, Burkert S, Goktas O, Haxel B, et al. Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study. Laryngoscope. 2014; 124(4):826–831.
Article13. Geissler K, Reimann H, Gudziol H, Bitter T, Guntinas-Lichius O. Olfactory training for patients with olfactory loss after upper respiratory tract infections. Eur Arch Otorhinolaryngol. 2014; 271(6):1557–1562.
Article14. Hedner M, Larsson M, Arnold N, Zucco GM, Hummel T. Cognitive factors in odor detection, odor discrimination, and odor identification tasks. J Clin Exp Neuropsychol. 2010; 32(10):1062–1067.
Article15. Wang L, Chen L, Jacob T. Evidence for peripheral plasticity in human odour response. J Physiol. 2004; 554(Pt 1):236–244.
Article16. Heilmann S, Huettenbrink KB, Hummel T. Local and systemic administration of corticosteroids in the treatment of olfactory loss. Am J Rhinol. 2004; 18(1):29–33.
Article17. Mott AE, Cain WS, Lafreniere D, Leonard G, Gent JF, Frank ME. Topical corticosteroid treatment of anosmia associated with nasal and sinus disease. Arch Otolaryngol Head Neck Surg. 1997; 123(4):367–372.
Article18. Blomqvist EH, Lundblad L, Bergstedt H, Stjärne P. Placebo-controlled, randomized, double-blind study evaluating the efficacy of fluticasone propionate nasal spray for the treatment of patients with hyposmia/anosmia. Acta Otolaryngol. 2014; 123(7):862–868.
Article19. Reden J, Mueller A, Mueller C, Konstantinidis I, Frasnelli J, Landis BN, et al. Recovery of Olfactory Function Following Closed Head Injury or Infections of the Upper Respiratory Tract. Arch Otolaryngol Head Neck Surg. 2006; 132(3):265–269.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparing the Effectiveness of Olfactory Training, According as Type and Preference of Odorant
- Pharmacologic therapy of olfaction disroders induced by COVID-19 upper respiratory infection
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19
- The Sniffing Bead System as a Useful Diagnostic Tool for Olfactory Dysfunction in COVID-19