J Korean Neuropsychiatr Assoc.
2019 Nov;58(4):339-345. 10.4306/jknpa.2019.58.4.339.
The Bodily Panic Symptoms and Predisposing Stressors in Korean Patients with Panic Disorder
- Affiliations
-
- 1Department of Psychiatry, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 2Department of Psychiatry and Institute of Behavioral Science in Medicine, College of Medicine, Yonsei University of Korea, Seoul, Korea.
- 3Department of Psychiatry, Inje University Haeundae Paik Hospital, Busan, Korea.
- 4Department of Psychiatry, Chonbuk National University Medical School, Jeonju, Korea.
- 5Department of Psychiatry, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 6Department of Psychiatry, CHA Bundang Medical Center, School of Medicine, CHA University of Korea, Seongnam, Korea.
- 7Department of psychiatry, School of Medicine, Kyungpook National University, Daegu, Korea.
- 8Department of Psychiatry, Kangbuk Samsung Hospital, College of Medicine, Sungkyunkwan University, Seoul, Korea.
- 9Department of Psychiatry, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 10Department of Psychiatry, Soonchunhyang University Seoul Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea.
- 11Department of Psychiatry, Samsung Medical Center, College of Medicine, Sungkyunkwan University, Seoul, Korea.
- 12Department of Psychiatry, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. healm@catholic.ac.kr
- KMID: 2465054
- DOI: http://doi.org/10.4306/jknpa.2019.58.4.339
Abstract
OBJECTIVES
The purpose of this study was to investigate the distinctive features of bodily panic symptoms and the predisposing conditions in Korean patients with panic disorder.
METHODS
This was a retrospective chart review study and the data were collected from twelve university-affiliated hospitals in Korea. The patients selected met the diagnostic criteria for panic disorder, were older than 20 years of age, and had initially visited a psychiatry department. The assessments included the chief complaints related to bodily panic symptoms, recent stressors, recent history of alcohol and sleep problems, and time to visit an outpatient clinic.
RESULTS
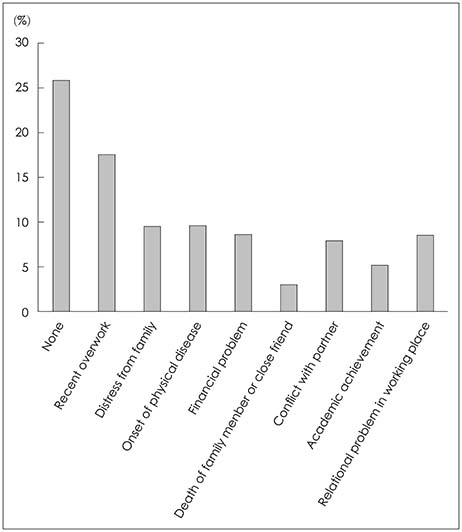
A total of 814 participants were included in the study. The most commonly experienced symptoms were cardiovascular and respiratory symptoms, which were observed in 63.9% and 55.4% of participants, respectively. Just before the onset of a panic attack, 25.6% of participants experienced sleep-related problems. Episodic binge drinking was also frequently observed (13.2%) and was more prevalent in men than in women (22.6% vs. 4.9%, p<0.001). About 75% of participants experienced stressful life events just before panic onset. Work-related issues were more prevalent in men than in women (22.0% vs. 13.4%, p=0.001). Family-related issues (4.8% vs. 14.1%, p<0.001) and conflict with a spouse or partner (4.0% vs.11.7%, p<0.001) were more prominent in women than in men.
CONCLUSION
Our results suggest that cardiovascular symptoms are the most common bodily panic symptoms in Korean patients. Our results suggest that a substantial portion of the Korean patients experienced stressful life events, sleep problems, and/or episodic binge drinking just before the onset of panic disorder.
MeSH Terms
Figure
Reference
-
1. American Psychiatry Association. Diagnostic and statistical manual of mental disorders, 5th edition: DSM-5. Arlington, VA: American Psychaitry Association;2013.2. de Jonge P, Roest AM, Lim CC, Florescu SE, Bromet EJ, Stein DJ, et al. Cross-national epidemiology of panic disorder and panic attacks in the world mental health surveys. Depress Anxiety. 2016; 33:1155–1177.
Article3. Sherbourne CD, Wells KB, Judd LL. Functioning and well-being of patients with panic disorder. Am J Psychiatry. 1996; 153:213–218.
Article4. Clark DM. A cognitive approach to panic. Behav Res Ther. 1986; 24:461–470.
Article5. Suh HS, Lee JH, Gim MS, Kim MK. Korean guidelines for the treatment of panic disorder. J Korean Med Assoc. 2018; 61:493–499.
Article6. McNally RJ. Panic and posttraumatic stress disorder: implications for culture, risk, and treatment. Cogn Behav Ther. 2008; 37:131–134.
Article7. Marques L, Robinaugh DJ, LeBlanc NJ, Hinton D. Cross-cultural variations in the prevalence and presentation of anxiety disorders. Expert Rev Neurother. 2011; 11:313–322.
Article8. Craske MG, Kircanski K, Epstein A, Wittchen HU, Pine DS, Lewis-Fernández R, et al. Panic disorder: a review of DSM-IV panic disorder and proposals for DSM-V. Depress Anxiety. 2010; 27:93–112.
Article9. Carter MM, Miller O Jr, Sbrocco T, Suchday S, Lewis EL. Factor structure of the Anxiety Sensitivity Index among African American college students. Psychological Assessment. 1999; 11:525–533.
Article10. Sierra-Siegert M, David AS. Depersonalization and individualism: the effect of culture on symptom profiles in panic disorder. J Nerv Ment Dis. 2007; 195:989–995.
Article11. Guarnaccia PJ, Rivera M, Franco F, Neighbors C. The experiences of ataques de nervios: towards an anthropology of emotions in Puerto Rico. Cult Med Psychiatry. 1996; 20:343–367.
Article12. Hinton DE, Hofmann SG, Pitman RK, Pollack MH, Barlow DH. The panic attack-posttraumatic stress disorder model: applicability to orthostatic panic among Cambodian refugees. Cogn Behav Ther. 2008; 37:101–116.
Article13. Kristensen AS, Mortensen EL, Mors O. The association between bodily anxiety symptom dimensions and the scales of the Revised NEO Personality Inventory and the Temperament and Character Inventory. Compr Psychiatry. 2009; 50:38–47.
Article14. Grant BF, Hasin DS, Stinson FS, Dawson DA, Goldstein RB, Smith S, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006; 67:363–374.
Article15. Cox BJ, Swinson RP, Endler NS, Norton GR. The symptom structure of panic attacks. Compr Psychiatry. 1994; 35:349–353.
Article16. Carleton RN, Duranceau S, Freeston MH, Boelen PA, McCabe RE, Antony MM. “But it might be a heart attack”: intolerance of uncertainty and panic disorder symptoms. J Anxiety Disord. 2014; 28:463–470.
Article17. Rho SS, Huh HJ, Chae JH, Kim DH, Lee DW, Seo HJ. Results of Public Awareness Survey of Panic Disorder at the 2014 Mental Health Exposition in Seoul. Anxiety and Mood. 2014; 10:176–181.18. Porcelli P, De Carne M. Non-fearful panic disorder in gastroenterology. Psychosomatics. 2008; 49:543–545.
Article19. Cox RC, Olatunji BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. 2016; 37:104–129.
Article20. Park HJ, Kim MS, Park EC, Jang SY, Kim W, Han KT. Association between sleep disorder and panic disorder in South Korea: nationwide nested case-control study of data from 2004 to 2013. Psychiatry Res. 2018; 260:286–291.
Article21. Fava GA, Grandi S, Rafanelli C, Canestrari R. Prodromal symptoms in panic disorder with agoraphobia: a replication study. J Affect Disord. 1992; 26:85–88.
Article22. Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychol Bull. 2009; 135:974–999.
Article23. Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002; 53:215–243.
Article24. Roth T, Roehrs T, Pies R. Insomnia: pathophysiology and implications for treatment. Sleep Med Rev. 2007; 11:71–79.
Article25. Cox BJ, Swinson RP, Shulman ID, Kuch K, Reichman JT. Gender effects and alcohol use in panic disorder with agoraphobia. Behav Res Ther. 1993; 31:413–416.
Article26. Stewart SH, Zeitlin SB. Anxiety sensitivity and alcohol use motives. J Anxiety Disord. 1995; 9:229–240.
Article27. Cosci F, Schruers KR, Abrams K, Griez EJ. Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship. J Clin Psychiatry. 2007; 68:874–880.28. Rassovsky Y, Hurliman E, Abrams K, Kushner MG. CO(2) hypersensitivity in recently abstinent alcohol dependent individuals:; a possible mechanism underlying the high risk for anxiety disorder among alcoholics. J Anxiety Disord. 2004; 18:159–176.
Article29. Klein DF. False suffocation alarms, spontaneous panics, and related conditions. An integrative hypothesis. Arch Gen Psychiatry. 1993; 50:306–317.
Article30. Klauke B, Deckert J, Reif A, Pauli P, Domschke K. Life events in panic disorder-an update on “candidate stressors”. Depress Anxiety. 2010; 27:716–730.
Article31. Uhde TW, Boulenger JP, Roy-Byrne PP, Geraci MF, Vittone BJ, Post RM. Longitudinal course of panic disorder: clinical and biological considerations. Prog Neuropsychopharmacol Biol Psychiatry. 1985; 9:39–51.
Article32. Faravelli C, Pallanti S. Recent life events and panic disorder. Am J Psychiatry. 1989; 146:622–626.
Article33. Pollard CA, Pollard HJ, Corn KJ. Panic onset and major events in the lives of agoraphobics: a test of contiguity. J Abnorm Psychol. 1989; 98:318–321.
Article34. Barzega G, Maina G, Venturello S, Bogetto F. Gender-related differences in the onset of panic disorder. Acta Psychiatr Scand. 2001; 103:189–195.
Article