J Korean Soc Radiol.
2019 Nov;80(6):1091-1106. 10.3348/jksr.2019.80.6.1091.
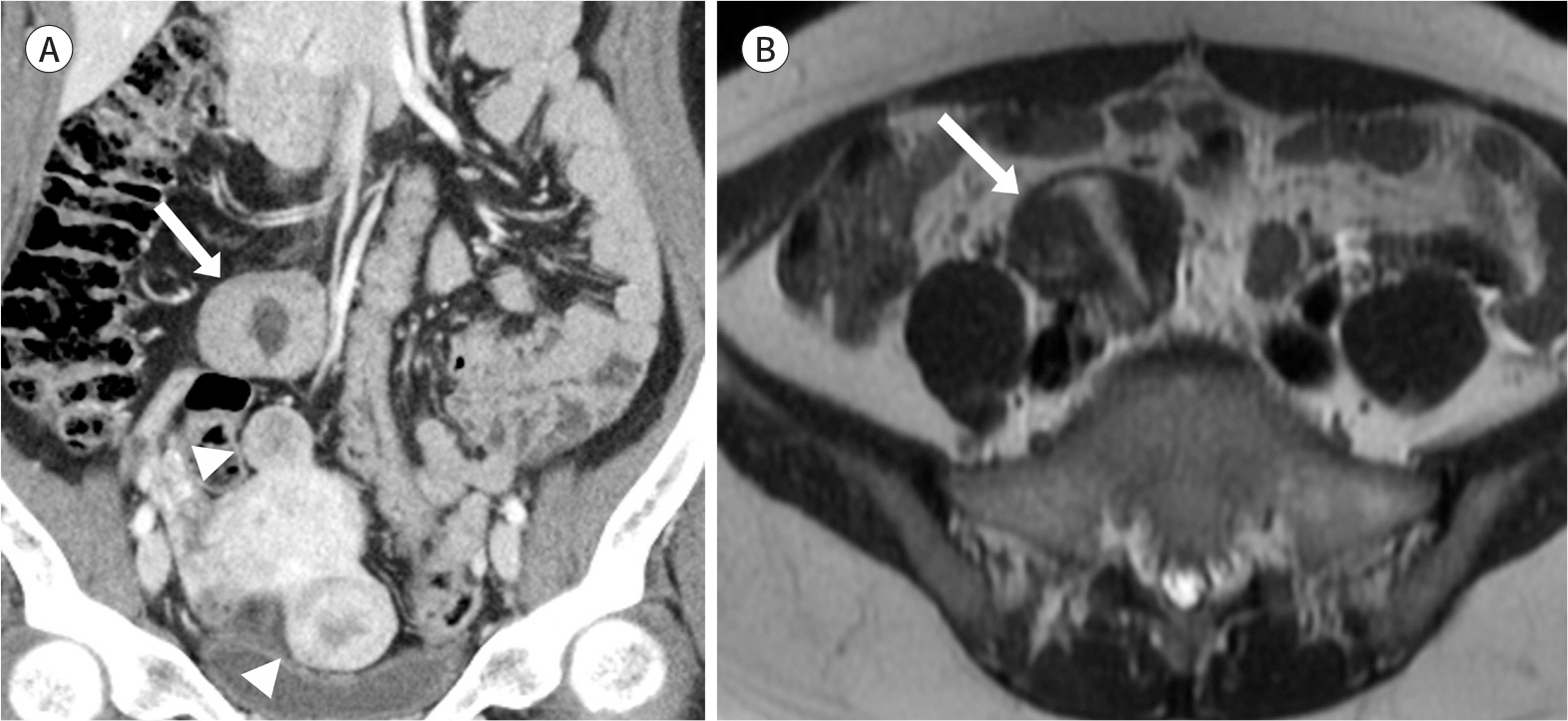
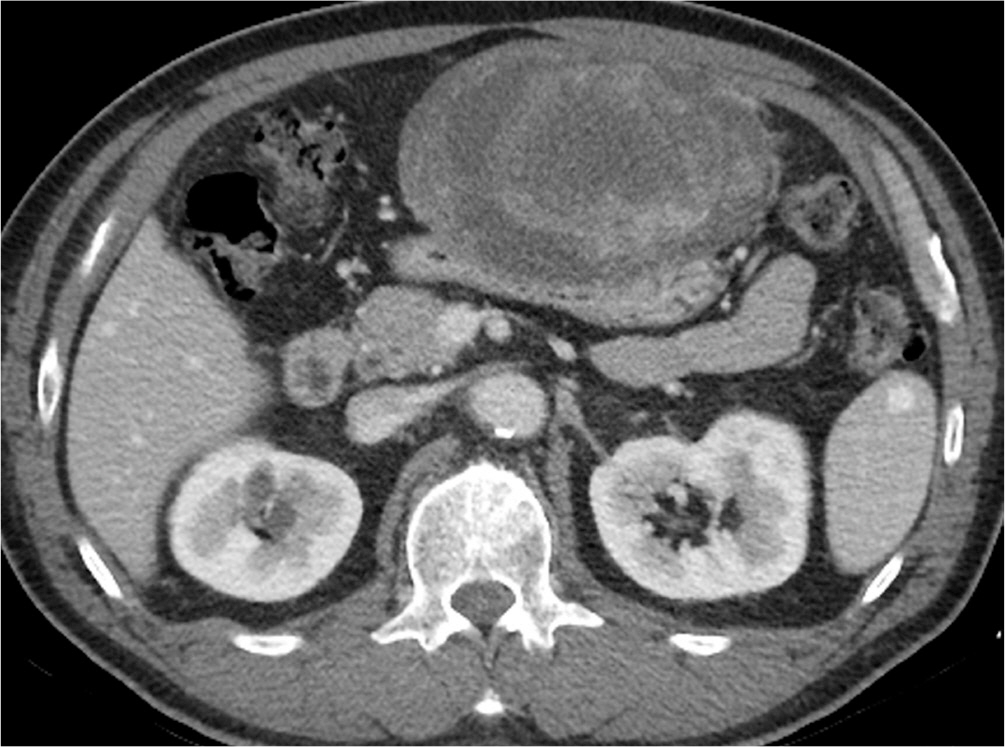
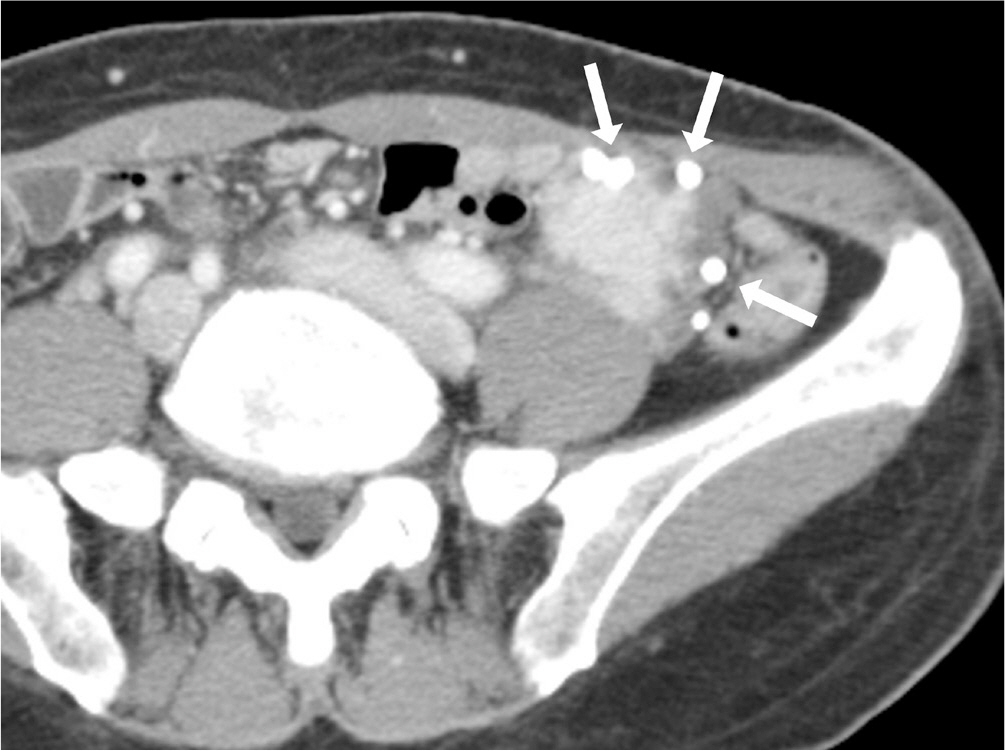
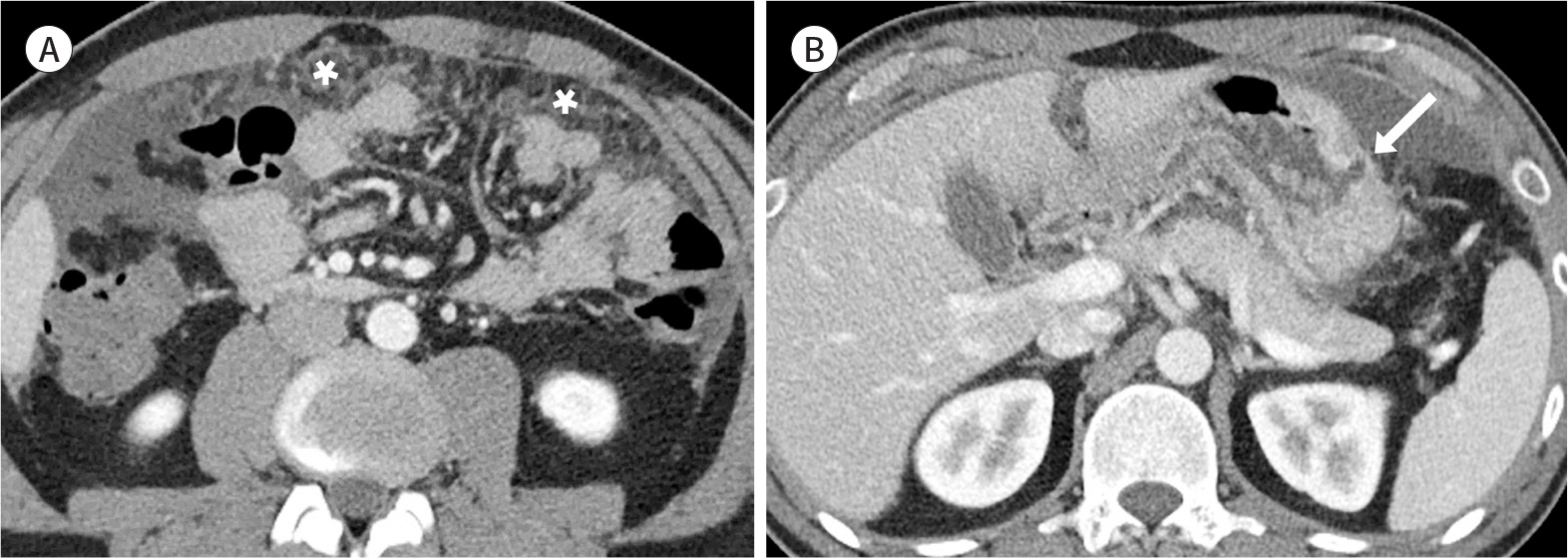
Mesenteric Lesions with Similar or Distinctive Appearances on CT
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University College of Medicine, Seoul Hospital, Seoul, Korea. jy0707hwang@schmc.ac.kr
- KMID: 2464909
- DOI: http://doi.org/10.3348/jksr.2019.80.6.1091
Abstract
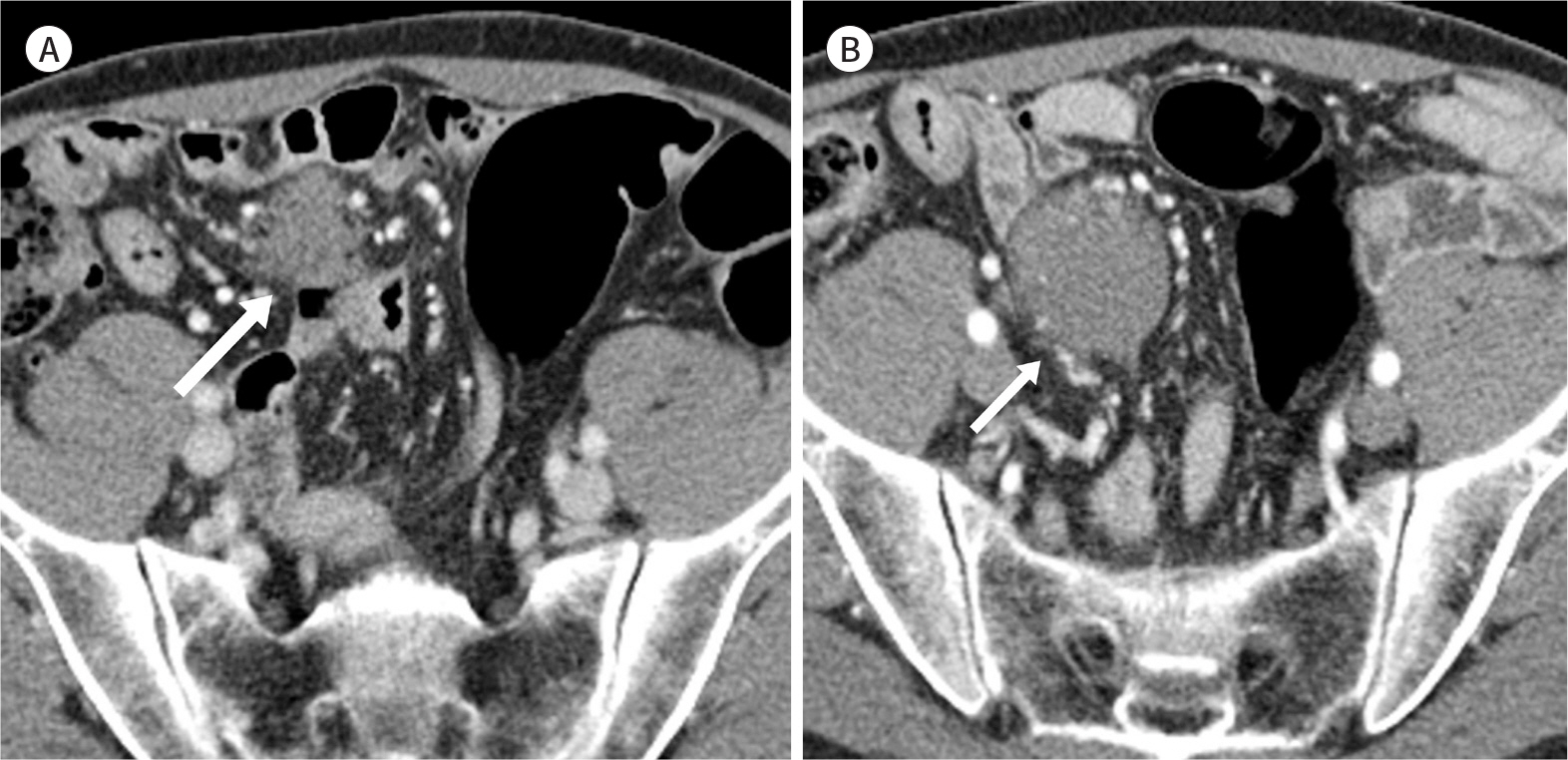
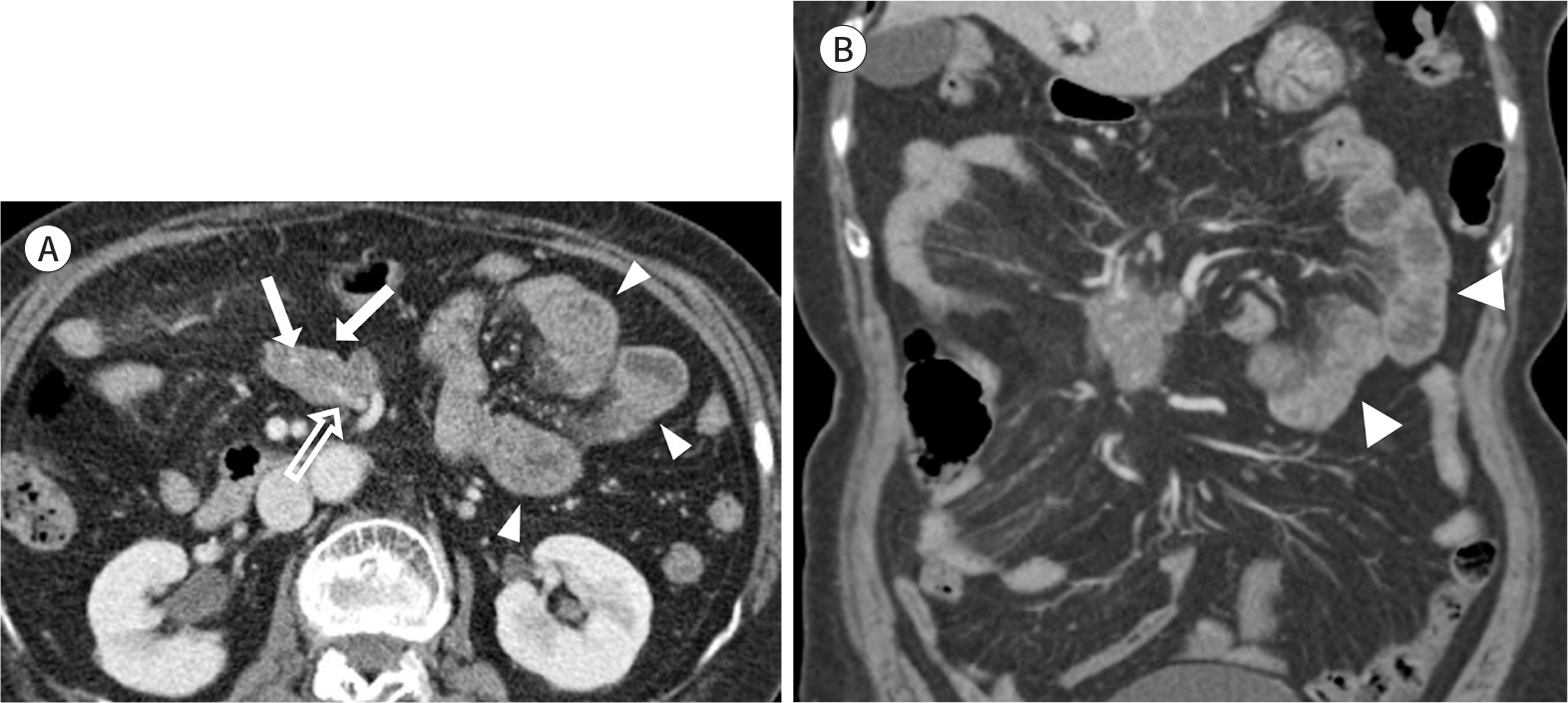
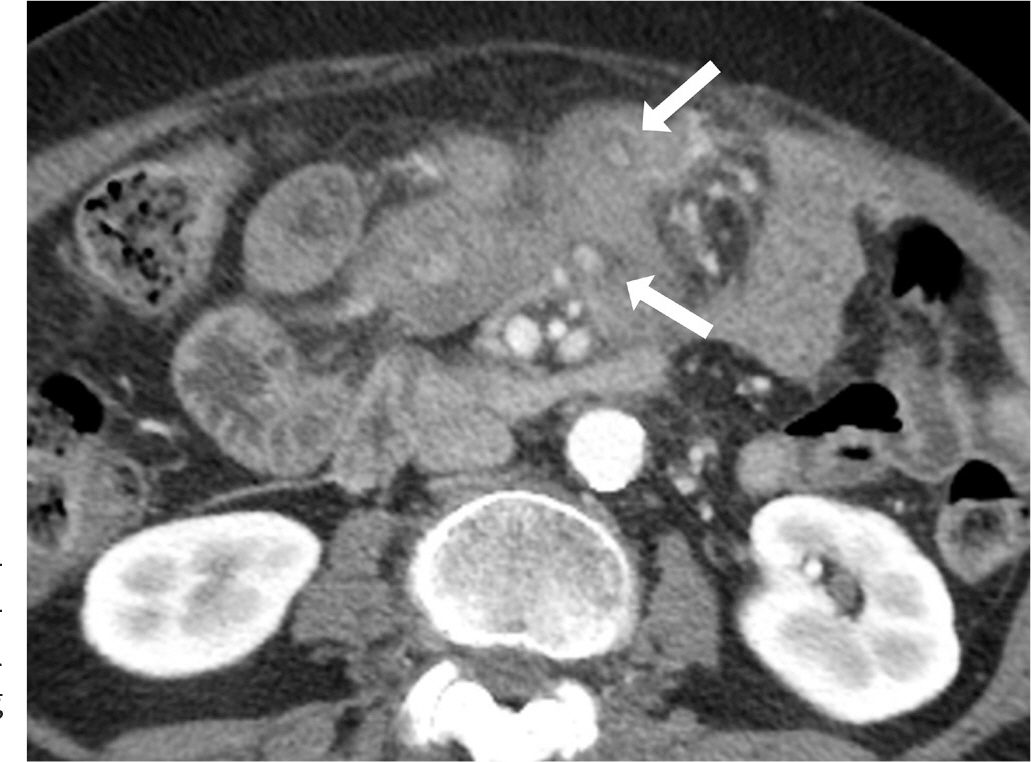
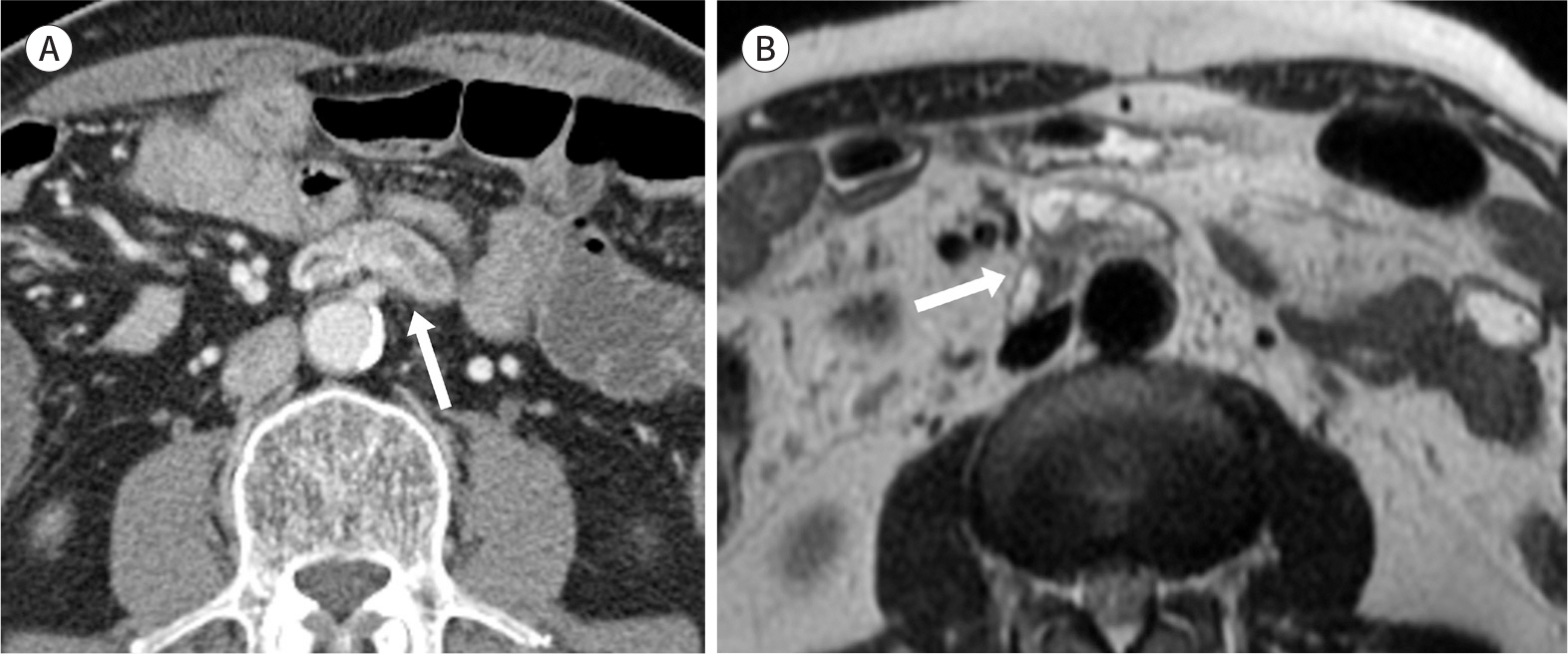
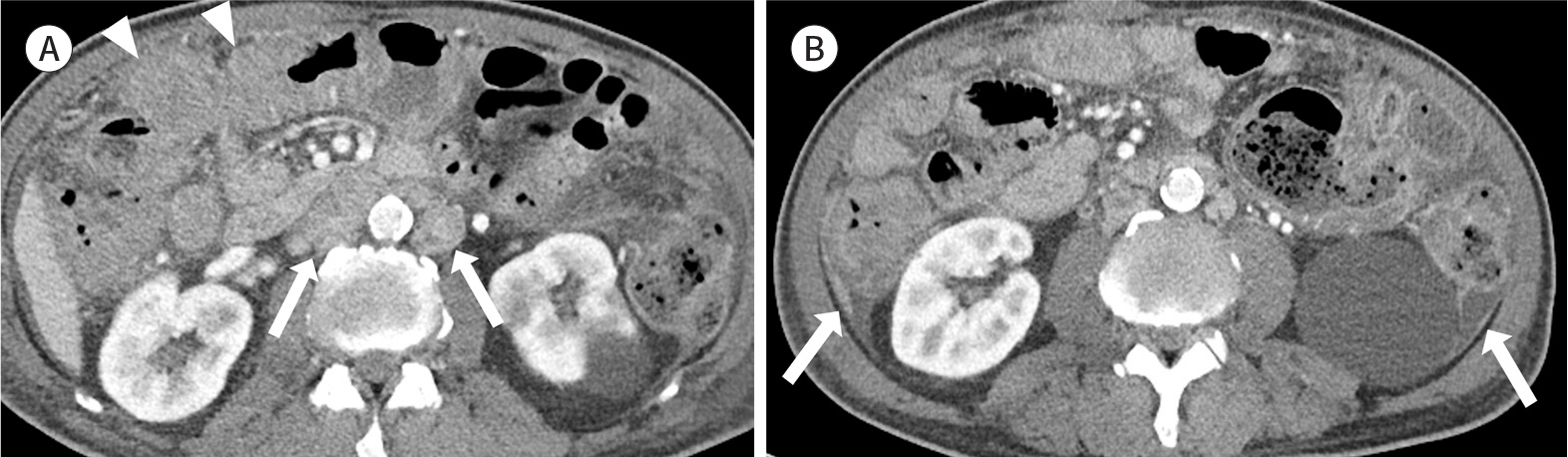
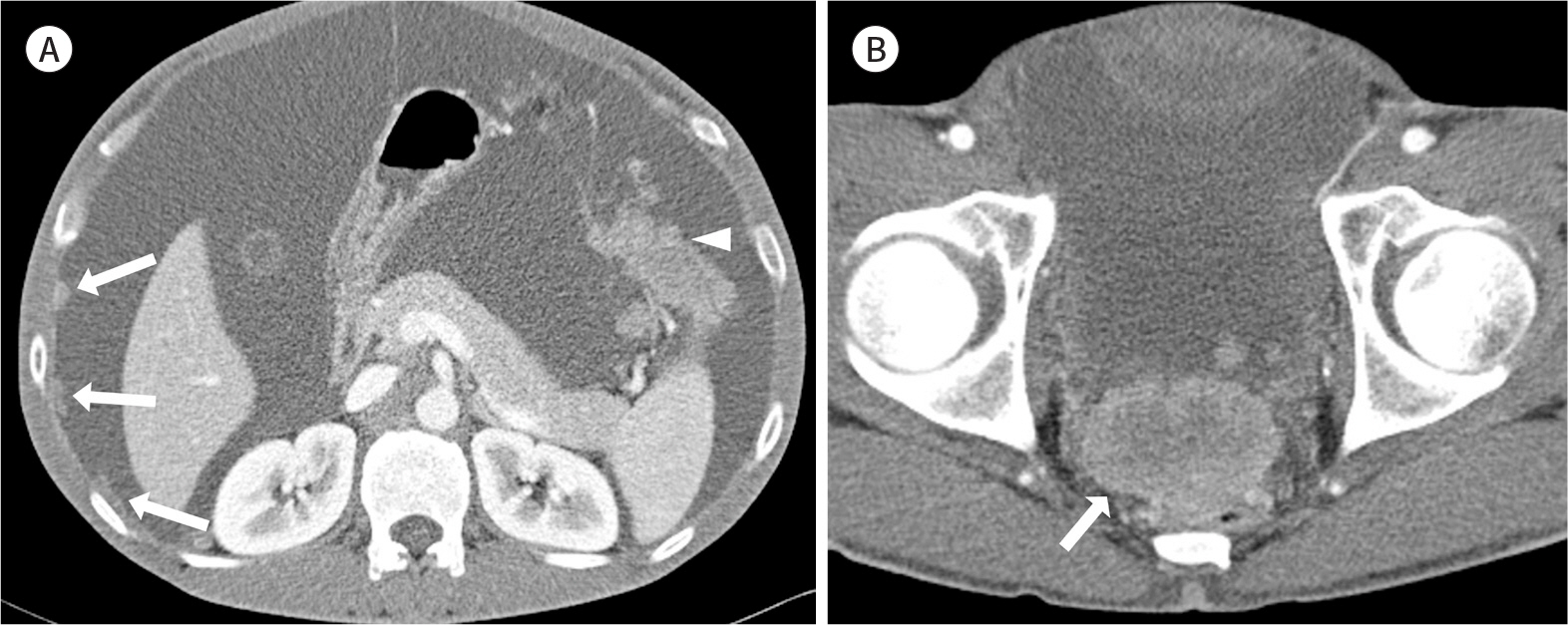
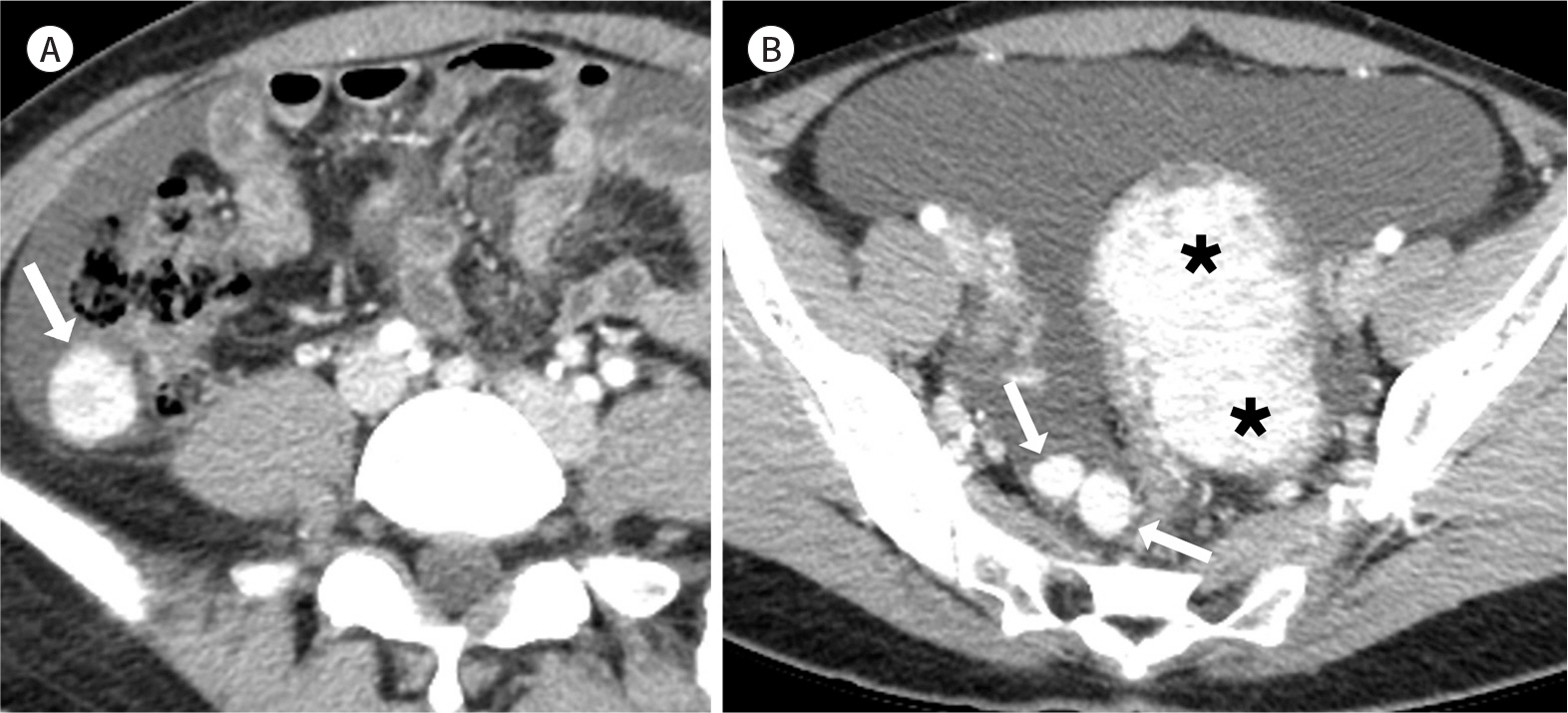
- The mesentery is a structure comprising a double peritoneal layer that attaches the bowel to the abdominal wall. Mesenteric disease can cause various non-specific clinical symptoms in adults and is sometimes found incidentally during unrelated diagnostic imaging studies. CT plays an essential role in the diagnosis of mesenteric disease, which can present with various radiologic features, including a solid mass, cystic mass, or local or diffuse infiltration on CT. Some mesenteric diseases present with distinctive characteristics, while others share similar findings, thereby complicating their differential diagnosis. Therefore, understanding the radiological findings of mesenteric disease is important for accurate diagnosis and appropriate treatment.
MeSH Terms
Figure
Reference
-
References
1. Sheth S, Horton KM, Garland MR, Fishman EK. Mesenteric neoplasms: CT appearances of primary and secondary tumors and differential diagnosis. Radiographics. 2003; 23:457–473. ; quiz 535–536.
Article2. Shinagare AB, Ramaiya NH, Jagannathan JP, Krajewski KM, Giardino AA, Butrynski JE, et al. A to Z of desmoid tumors.AJR Am J Roentgenol. 2011; 197:W1008–W1014.3. Righetti AE, Jacomini C, Parra RS, De Almeida AL, Rocha JJ, Féres O. Familial adenomatous polyposis and desmoid tumors. Clinics (Sao Paulo). 2011; 66:1839–1842.
Article4. Brooks AP, Reznek RH, Nugent K, Farmer KC, Thomson JP, Phillips RK. CT appearances of desmoid tumours in familial adenomatous polyposis: further observations. Clin Radiol. 1994; 49:601–607.
Article5. Chen TS, Montgomery EA. Are tumefactive lesions classified as sclerosing mesenteritis a subset of IgG4-related sclerosing disorders? J Clin Pathol. 2008; 61:1093–1097.
Article6. George V, Tammisetti VS, Surabhi VR, Shanbhogue AK. Chronic fibrosing conditions in abdominal imaging. Radiographics. 2013; 33:1053–1080.
Article7. Levy AD, Rimola J, Mehrotra AK, Sobin LH. From the archives of the AFIP: benign fibrous tumors and tumorlike lesions of the mesentery: radiologic-pathologic correlation. Radiograph/iics. 2006; 26:245–264.8. Horton KM, Lawler LP, Fishman EK. CT findings in sclerosing mesenteritis (panniculitis): spectrum of disease. Radiographics. 2003; 23:1561–1567.
Article9. Halligan S, Plumb A, Taylor S. Mesenteric panniculitis: systematic review of cross-sectional imaging findings and risk of subsequent malignancy. Eur Radiol. 2016; 26:4531–4537.
Article10. Chang S, Choi D, Lee SJ, Lee WJ, Park MH, Kim SW, et al. Neuroendocrine neoplasms of the gastrointestinal.11. Sahani DV, Bonaffini PA, Fernández-Del Castillo C, Blake MA. Gastroenteropancreatic neuroendocrine tumors: role of imaging in diagnosis and management.Radiology. 2013; 266:38–61.12. Tan EH, Tan CH. Imaging of gastroenteropancreatic neuroendocrine tumors.World J Clin Oncol. 2011; 2:28–43.13. Whitley NO, Bohlman ME, Baker LP. CT patterns of mesenteric disease. J Comput Assist Tomogr. 1982; 6:490–496.
Article14. Granger J, Mahapatra R, Hamid B, Gillespie K, Fok M, Vimalachandran D. Incidental mesenteric paraganglioma: a csse report and literature review.Ann Coloproctol. 2017; 33:197–200.15. Ozkan Z, San Ozdemir C, Yasar G, Altas O, Koc M, Gul Y, et al. An unusual mesenteric tumor ‘paraganglioma': a case report.Iran Red Crescent Med J. 2014; 16:e16837.16. Fujita T, Kamiya K, Takahashi Y, Miyazaki S, Iino I, Kikuchi H, et al. Mesenteric paraganglioma: report of a case.World J Gastrointest Surg. 2013; 5:62–67.17. Kim HI, Koo BK, Lee YJ, Kim JT, Cho YM, Lee KU, et al. A case of paraganglioma arising in the transverse mesocolon. J Korean Soc Endocrinol. 2005; 20:496–501.
Article18. Erickson D, Kudva YC, Ebersold MJ, Thompson GB, Grant CS, Van Heerden JA, et al. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients.J Clin Endocrinol Metab. 2001; 86:5210–5216.19. Lee KY, Oh YW, Noh HJ, Lee YJ, Yong HS, Kang EY, et al. Extraadrenal paragangliomas of the body: imaging features. AJR Am J Roentgenol. 2006; 187:492–504.
Article20. Rosica G, Santilli G, Bucari D, Amici B, Bulletti F, Patacchiola F, et al. A case of disseminated peritoneal leiomyomatosis and diffuse uterine leiomyomatosis. Clin Exp Obstet Gynecol. 2011; 38:84–87.21. Fasih N, Prasad Shanbhogue AK, Macdonald DB, Fraser-Hill MA, Papadatos D, Kielar AZ, et al. Leiomyomas beyond the uterus: unusual locations, rare manifestations.Radiographics. 2008; 28:1931–1948.22. Julien C, Bourgouin S, Boudin L, Balandraud P. Disseminated peritoneal leiomyomatosis.J Gastrointest Surg. 2019; 23:605–607.23. Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000; 13:577–585.
Article24. Angelico G, Spadola S, Trombatore C. Clinicopathological and prognostic features of extragastrointestinal stromal tumors of the omentum: a review. J Gastroenterol Res. 2017; 1:9–13.
Article25. Watal P, Brahmbhatt SG, Thoriya PJ, Bahri NU. Retroperitoneal extragastrointestinal stromal tumor: radiologic pathologic correlation.J Clin Imaging Sci. 2014; 4:34.26. Bass JC, Korobkin M, Francis IR, Ellis JH, Cohan RH. Retroperitoneal plexiform neurofibromas: CT findings. AJR Am J Roentgenol. 1994; 163:617–620.
Article27. Fortman BJ, Kuszyk BS, Urban BA, Fishman EK. Neurofibromatosis type 1: a diagnostic mimicker at CT. Radi ographics. 2001; 21:601–612.
Article28. Romeo V, Maurea S, Mainenti PP, Camera L, Aprea G, Cozzolino I, et al. Correlative imaging of cystic lymphangiomas: ultrasound, CT and MRI comparison. Acta Radiol Open. 2015; 4:2047981614564911.
Article29. Levy AD, Cantisani V, Miettinen M. Abdominal lymphangiomas: imaging features with pathologic correlation. AJR Am J Roentgenol. 2004; 182:1485–1491.
Article30. Palomeque Jiménez A, Herrera Fernández FA, Calzado Baeza S, Reyes Moreno M. Giant mesenteric cystic lymphangioma as an incidental finding in a young adult.Gastroenterol Hepatol. 2014; 37:416–417.31. Park JY, Kim KW, Kwon HJ, Park MS, Kwon GY, Jun SY, et al. Peritoneal mesotheliomas: clinicopathologic features, CT findings, and differential diagnosis.AJR Am J Roentgenol. 2008; 191:814–825.32. Lee R, Tong A, Kurtis B, Gilet AG. Benign multicystic peritoneal mesothelioma: AIRP best cases in radiologic-pathologic correlation. Radiographics. 2016; 36:407–411.33. Ojili V, Tirumani SH, Gunabushanam G, Nagar A, Surabhi VR, Chintapalli KN, et al. Abdominal hemangiomas: a pictorial review of unusual, atypical, and rare types. Can Assoc Radiol J. 2013; 64:18–27.
Article34. Ilhan M, Oner G, Gök AF, BulakçI M, Yeg˘en G. Treatment of atypically-localized cavernous hemangioma in abdomen with atypical pain.Int J Surg Case Rep. 2016; 25:24–27.35. Si-Mohamed S, Aufort S, Khellaf L, Ramos J, Gasne P, Durand L. Mesenteric cavernous hemangioma: imaging-pathologic correlation.Diagn Interv Imaging. 2015; 96:495–498.36. Gezer NS, Bas¸ara I, Altay C, Harman M, Rocher L, Karabulut N, et al. Abdominal sarcoidosis: cross-sectional imaging findings.Diagn Interv Radiol. 2015; 21:111–117.37. Warshauer DM, Lee JK. Imaging manifestations of abdominal sarcoidosis.AJR Am J Roentgenol. 2004; 182.38. Lee WK, Lau EW, Duddalwar VA, Stanley AJ, Ho YY. Abdominal manifestations of extranodal lymphoma: imaging features. ISRN Radiol. 2013; 2013:483069.39. Manzella A, Borba-Filho P, D'Ippolito G, Farias M. Abdominal manifestations of lymphoma: spectrum of imaging features. ISRN Radiol. 2013; 2013:483069.
Article40. Nishino M, Hayakawa K, Minami M, Yamamoto A, Ueda H, Takasu K. Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues.Radiographics. 2003; 23:45–57.41. Demirkazik FB, Akhan O, Ozmen MN, Akata D. US and CT findings in the diagnosis of tuberculous peritonitis. Acta Rad/iiol. 1996; 37:517–520.
Article42. Ha HK, Jung JI, Lee MS, Choi BG, Lee MG, Kim YH, et al. CT differentiation of tuberculous peritonitis and peritoneal carcinomatosis.AJR Am J Roentgenol. 1996; 167:743–748.43. Na-ChiangMai W, Pojchamarnwiputh S, Lertprasertsuke N, Chitapanarux T. CT findings of tuberculous peritonitis.Singapore Med J. 2008; 49:488–491.44. Levy AD, Shaw JC, Sobin LH. Secondary tumors and tumorlike lesions of the peritoneal cavity: imaging features with pathologic correlation.Radiographics. 2009; 29:347–373.45. Walkey MM, Friedman AC, Sohotra P, Radecki PD. CT manifestations of peritoneal carcinomatosis.AJR Am J Roentgenol. 1988; 150:1035–1041.46. Karaosmanoglu D, Karcaaltincaba M, Oguz B, Akata D, Ozmen M, Akhan O. CT findings of lymphoma with peritoneal, omental and mesenteric involvement: peritoneal lymphomatosis.Eur J Radiol. 2009; 71:313–317.47. Cabral FC, Krajewski KM, Kim KW, Ramaiya NH, Jagannathan JP. Peritoneal lymphomatosis: CT and PET/CT findings and how to differentiate between carcinomatosis and sarcomatosis.Cancer Imaging. 2013; 13.48. Selikoff IJ, Hammond EC, Seidman H. Latency of asbestos disease among insulation workers in the United States and Canada. Cancer. 1980; 46:2736–2740.49. Arleo EK, Schwartz PE, Hui P, McCarthy S. Review of leiomyoma variants.AJR Am J Roentgenol. 2015; 205:912–921.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Appearances of Appendiceal Diseases
- Phytobezoars in the Small Intestine: CT and US Appearances
- Radiologic Imaging of Traumatic Bowel and Mesenteric Injuries: A Comprehensive Up-to-Date Review
- Assessment of Mesenteric Vascular Steno-occlusive Lesion in Acute Mesenteric Ischemia: Comparison between CT Angiography and Digital Subtraction Angiography
- Liver Neoplasms: Atypical CT and MR Imaging Findings