Ann Hepatobiliary Pancreat Surg.
2019 Nov;23(4):372-376. 10.14701/ahbps.2019.23.4.372.
Clinical importance of preoperative and postoperative prognostic nutritional index in patients with pancreatic ductal adenocarcinoma
- Affiliations
-
- 1Department of Surgery, Tottori Prefectural Central Hospital, Tottori, Japan. ikeguchim@tp-ch.jp
- KMID: 2464327
- DOI: http://doi.org/10.14701/ahbps.2019.23.4.372
Abstract
- BACKGROUNDS/AIMS
The prognostic nutritional index (PNI) is based on the albumin concentration and absolute lymphocyte count and is designed to assess the nutritional and immunological status of patients. In this study, we evaluated the prognostic importance of the preoperative and postoperative PNI in patients who underwent curative resection of pancreatic ductal adenocarcinoma (PDAC).
METHODS
From 2006 to 2017, 50 patients with PDAC underwent curative resection at our hospital. We performed distal pancreatectomy (DP) with splenectomy in 15 patients, pancreaticoduodenectomy (PD) in 27 patients, PD combined with portal vein partial resection in 6 patients, and total pancreatectomy with splenectomy in 2 patients. We compared the preoperative PNI and postoperative PNI (1 and 2 months postoperatively) and analyzed the prognostic importance for these patients.
RESULTS
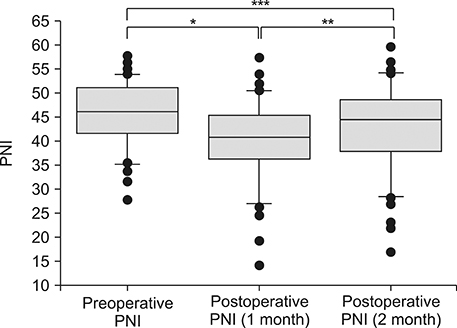
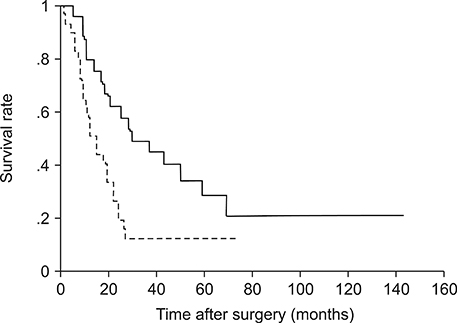
The mean PNI significantly decreased from 45.5 preoperatively to 39.8 at 1 month postoperatively (p<0.001), but recovered to 42.7 at 2 months postoperatively. In 23 patients, the PNI at 2 months postoperatively recovered to the preoperative level (recovered group), but in the remaining 27 patients, the PNI at 2 months postoperatively did not reach the preoperative level (non-recovered group). The overall median survival time in the recovered group (29 months) was significantly longer than that in the non-recovered group (12 months, p=0.003). The multivariate overall analysis demonstrated that good recovery of the postoperative PNI was strongly correlated with a better prognosis.
CONCLUSIONS
Effective postoperative nutrition may have a prognostic benefit for patients with operable PDAC.
MeSH Terms
Figure
Reference
-
1. Onodera T, Goseki N, Kosaki G. [Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients]. Nihon Geka Gakkai Zasshi. 1984; 85:1001–1005. Japanese.2. Nozoe T, Kohno M, Iguchi T, Mori E, Maeda T, Matsukuma A, et al. The prognostic nutritional index can be a prognostic indicator in colorectal carcinoma. Surg Today. 2012; 42:532–535.3. Kato M, Hashimoto H, Noro T, Takahashi H, Hirashima T, Yamashiro A, et al. Pre and postoperative immunity in aged cancer patients-with special refference to the postoperative mehcllin-cefem resistant staphylococcus aureus (MRSA) infection and cell-mediated immunity. J Jpn Surg Assoc. 1992; 53:1033–1038.4. Sagawa M, Yoshimatsu K, Yokomizo H, Yano Y, Okayama S, Yamada Y, et al. Pulmonary dysfunction function and poor nutritional status are risk factors for remote infections following surgery for colorectal cancer. J Nippon Med Sch. 2018; 85:208–214.5. Ikeguchi M, Ashida K, Saito H. New prognostic indicator is useful for predicting the survival of patients with unresectable advanced colorectal cancer. Hepatogastroenterology. 2015; 62:859–862.6. Li D, Yuan X, Liu J, Li C, Li W. Prognostic value of prognostic nutritional index in lung cancer: a meta-analysis. J Thorac Dis. 2018; 10:5298–5307.7. Luo Z, Zhou L, Balde AI, Li Z, He L, Zhen Wei C, et al. Prognostic impact of preoperative prognostic nutritional index in resected advanced gastric cancer: a multicenter propensity score analysis. Eur J Surg Oncol. 2019; 45:425–431.8. Yamamoto T, Yagi S, Kinoshita H, Sakamoto Y, Okada K, Uryuhara K, et al. Long-term survival after resection of pancreatic cancer: a single-center retrospective analysis. World J Gastroenterol. 2015; 21:262–268.9. Sato D, Tsuchikawa T, Mitsuhashi T, Hatanaka Y, Marukawa K, Morooka A, et al. Stromal palladin expression is an independent prognostic factor in pancreatic ductal adenocarcinoma. PLoS One. 2016; 11:e0152523.10. Greene FL, editor. AJCC cancer staging handbook: from the AJCC cancer staging manual. 6th ed. New York: Springer;2002.11. Li Z, Bai B, Ji G, Li J, Zhao Q. Relationship between Clavien-Dindo classification and long-term survival outcomes after curative resection for gastric cancer: a propensity score-matched analysis. Int J Surg. 2018; 60:67–73.12. Choe JW, Kim HJ, Kim JS, Cha J, Joo MK, Lee BJ, et al. Usefulness of CA 19-9 for pancreatic cancer screening in patients with new-onset diabetes. Hepatobiliary Pancreat Dis Int. 2018; 17:263–268.13. Riedel B, Sloan E, Forget P. Long-term consequences of the acute neural-inflammatory stress response in the cancer surgical patient: new findings and perspectives. Int Anesthesiol Clin. 2016; 54:58–71.14. Gottschalk A, Sharma S, Ford J, Durieux ME, Tiouririne M. Review article: the role of the perioperative period in recurrence after cancer surgery. Anesth Analg. 2010; 110:1636–1643.15. Horowitz M, Neeman E, Sharon E, Ben-Eliyahu S. Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol. 2015; 12:213–226.16. Murakami Y, Saito H, Kono Y, Shishido Y, Kuroda H, Matsunaga T, et al. Combined analysis of the preoperative and postoperative prognostic nutritional index offers a precise predictor of the prognosis of patients with gastric cancer. Surg Today. 2018; 48:395–403.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative outcomes of older adult patients with pancreatic cancer based on nutritional status: a retrospective cohorat study
- Pathological Classification of Panaeatic Cancer and Precancerous Casion
- Preoperative nutritional scores to predict mortality after liver transplantation: a retrospective cohort study
- Preoperative Prognostic Nutritional Index is a significant predictive factor for posthepatectomy bile leakage
- The Effect of Preoperative Nutritional Depletion on Postoperative Complications in the patient with Multiple Injuries