J Gastric Cancer.
2019 Mar;19(1):62-71. 10.5230/jgc.2019.19.e1.
Long-term Outcomes of Laparoscopic Versus Open Transhiatal Approach for the Treatment of Esophagogastric Junction Cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. hhkim@snubh.org
- KMID: 2458818
- DOI: http://doi.org/10.5230/jgc.2019.19.e1
Abstract
- PURPOSE
The laparoscopic transhiatal approach (LA) for adenocarcinoma of the esophagogastric junction (AEJ) is advantageous since it allows better visualization of the surgical field than the open approach (OA). We compared the surgical outcomes of the 2 approaches.
MATERIALS AND METHODS
We analyzed 108 patients with AEJ who underwent transhiatal distal esophagectomy and gastrectomy with curative intent between 2003 and 2015. Surgical outcomes were reviewed using electronic medical records.
RESULTS
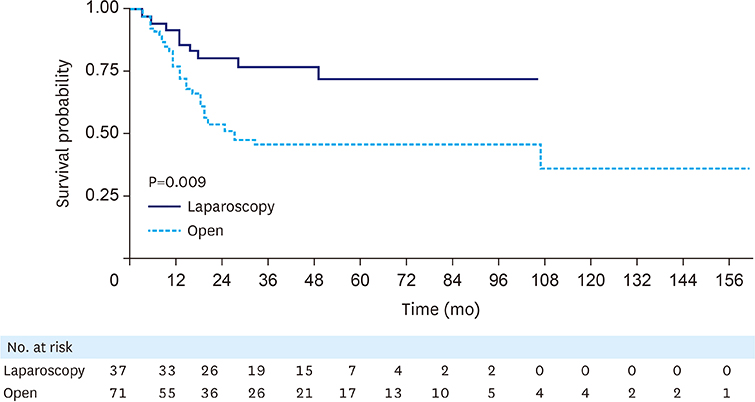
The LA and OA were performed in 37 and 71 patients, respectively. Compared to the OA, the LA was associated with significantly shorter duration of postoperative hospital stay (9 vs. 11 days, P=0.001), shorter proximal resection margins (3 vs. 7 mm, P=0.004), and extended operative times (240 vs. 191 min, P=0.001). No significant difference was observed between the LA and OA for intraoperative blood loss (100 vs. 100 mL, P=0.392) or surgical morbidity rate (grade≥II) for complications (8.1% vs. 23.9%, P=0.080). Two cases of anastomotic leakage occurred in the OA group. The number of harvested lymph nodes was not significantly different between the LA and OA groups (54 vs. 51, P=0.889). The 5-year overall and 3-year relapse-free survival rates were 81.8% and 50.7% (P=0.024) and 77.3% and 46.4% (P=0.009) for the LA and OA groups, respectively. Multivariable analyses revealed no independent factors associated with overall survival.
CONCLUSIONS
The LA is feasible and safe with short- and long-term oncologic outcomes similar to those of the OA.
MeSH Terms
Figure
Reference
-
1. Buas MF, Vaughan TL. Epidemiology and risk factors for gastroesophageal junction tumors: understanding the rising incidence of this disease. Semin Radiat Oncol. 2013; 23:3–9.
Article2. Hasegawa S, Yoshikawa T, Cho H, Tsuburaya A, Kobayashi O. Is adenocarcinoma of the esophagogastric junction different between Japan and western countries? The incidence and clinicopathological features at a Japanese high-volume cancer center. World J Surg. 2009; 33:95–103.
Article3. Chung JW, Lee GH, Choi KS, Kim DH, Jung KW, Song HJ, et al. Unchanging trend of esophagogastric junction adenocarcinoma in Korea: experience at a single institution based on Siewert's classification. Dis Esophagus. 2009; 22:676–681.
Article4. Hatta W, Tong D, Lee YY, Ichihara S, Uedo N, Gotoda T. Different time trend and management of esophagogastric junction adenocarcinoma in three Asian countries. Dig Endosc. 2017; 29:Suppl 2. 18–25.
Article5. Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K, et al. Adenocarcinoma of the gastroesophageal junction in Japan: relevance of Siewert's classification applied to 177 cases resected at a single institution. J Am Coll Surg. 1999; 189:594–601.
Article6. Suh YS, Han DS, Kong SH, Lee HJ, Kim YT, Kim WH, et al. Should adenocarcinoma of the esophagogastric junction be classified as esophageal cancer? A comparative analysis according to the seventh AJCC TNM classification. Ann Surg. 2012; 255:908–915.
Article7. Orringer MB. Transhiatal esophagectomy without thoracotomy for carcinoma of the thoracic esophagus. Ann Surg. 1984; 200:282–288.
Article8. Kurokawa Y, Sasako M, Sano T, Yoshikawa T, Iwasaki Y, Nashimoto A, et al. Ten-year follow-up results of a randomized clinical trial comparing left thoracoabdominal and abdominal transhiatal approaches to total gastrectomy for adenocarcinoma of the oesophagogastric junction or gastric cardia. Br J Surg. 2015; 102:341–348.9. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.10. Kinoshita T, Gotohda N, Kato Y, Takahashi S, Konishi M, Okazumi S, et al. Laparoscopic transhiatal resection for Siewert type II adenocarcinoma of the esophagogastric junction: operative technique and initial results. Surg Laparosc Endosc Percutan Tech. 2012; 22:e199–e203.11. DePaula AL, Hashiba K, Ferreira EA, de Paula RA, Grecco E. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc. 1995; 5:1–5.12. Swanstrom LL, Hansen P. Laparoscopic total esophagectomy. Arch Surg. 1997; 132:943–947.
Article13. Perry KA, Enestvedt CK, Pham T, Welker M, Jobe BA, Hunter JG, et al. Comparison of laparoscopic inversion esophagectomy and open transhiatal esophagectomy for high-grade dysplasia and stage I esophageal adenocarcinoma. Arch Surg. 2009; 144:679–684.
Article14. Montenovo MI, Chambers K, Pellegrini CA, Oelschlager BK. Outcomes of laparoscopic-assisted transhiatal esophagectomy for adenocarcinoma of the esophagus and esophago-gastric junction. Dis Esophagus. 2011; 24:430–436.
Article15. Sugita S, Kinoshita T, Kaito A, Watanabe M, Sunagawa H. Short-term outcomes after laparoscopic versus open transhiatal resection of Siewert type II adenocarcinoma of the esophagogastric junction. Surg Endosc. 2018; 32:383–390.
Article16. Huang CM, Lv CB, Lin JX, Chen QY, Zheng CH, Li P, et al. Laparoscopic-assisted versus open total gastrectomy for Siewert type II and III esophagogastric junction carcinoma: a propensity score-matched case-control study. Surg Endosc. 2017; 31:3495–3503.
Article17. Lee MS, Lee JH, Park DJ, Lee HJ, Kim HH, Yang HK. Comparison of short- and long-term outcomes of laparoscopic-assisted total gastrectomy and open total gastrectomy in gastric cancer patients. Surg Endosc. 2013; 27:2598–2605.
Article18. Kim HS, Kim BS, Lee IS, Lee S, Yook JH, Kim BS. Comparison of totally laparoscopic total gastrectomy and open total gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A. 2013; 23:323–331.
Article19. Kim JH, Park SS, Kim J, Boo YJ, Kim SJ, Mok YJ, et al. Surgical outcomes for gastric cancer in the upper third of the stomach. World J Surg. 2006; 30:1870–1876.
Article20. Bissolati M, Desio M, Rosa F, Rausei S, Marrelli D, Baiocchi GL, et al. Risk factor analysis for involvement of resection margins in gastric and esophagogastric junction cancer: an Italian multicenter study. Gastric Cancer. 2017; 20:70–82.
Article21. Jang YJ, Park MS, Kim JH, Park SS, Park SH, Kim SJ, et al. Advanced gastric cancer in the middle one-third of the stomach: Should surgeons perform total gastrectomy? J Surg Oncol. 2010; 101:451–456.22. Lee JH, Kim YI. Which is the optimal extent of resection in middle third gastric cancer between total gastrectomy and subtotal gastrectomy? J Gastric Cancer. 2010; 10:226–233.
Article23. Lee CM, Jee YS, Lee JH, Son SY, Ahn SH, Park DJ, et al. Length of negative resection margin does not affect local recurrence and survival in the patients with gastric cancer. World J Gastroenterol. 2014; 20:10518–10524.
Article24. Hosoda K, Yamashita K, Katada N, Moriya H, Mieno H, Sakuramoto S, et al. Impact of lower mediastinal lymphadenectomy for the treatment of esophagogastric junction carcinoma. Anticancer Res. 2015; 35:445–456.25. Suh YS, Lee KG, Oh SY, Kong SH, Lee HJ, Kim WH, et al. Recurrence pattern and lymph node metastasis of adenocarcinoma at the esophagogastric junction. Ann Surg Oncol. 2017; 24:3631–3639.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic and Laparoscopic Full-Thickness Resection of Endophytic Gastric Submucosal Tumors Very Close to the Esophagogastric Junction
- Total robotic transhiatal excision for a large left-sided esophageal epiphrenic diverticulum: a case report
- Long-term Outcomes of Laparoscopic versus Open Surgery for Rectal Cancer: A Singlecenter Retrospective Analysis
- Diagnostic Approach for Esophagogastric Junction Outflow Obstruction
- Laparoscopic Gastric Wedge Resection and Prophylactic Antireflux Surgery for a Submucosal Tumor of Gastroesophageal Junction