J Gastric Cancer.
2015 Dec;15(4):278-285. 10.5230/jgc.2015.15.4.278.
Endoscopic and Laparoscopic Full-Thickness Resection of Endophytic Gastric Submucosal Tumors Very Close to the Esophagogastric Junction
- Affiliations
-
- 1Gastric Cancer Center, Kyungpook National University Medical Center, Daegu, Korea. wyu@knu.ac.kr
- KMID: 2391563
- DOI: http://doi.org/10.5230/jgc.2015.15.4.278
Abstract
- PURPOSE
Gastric submucosal tumors (SMTs) located very close to the esophagogastric junction (EGJ) are a challenge for gastric surgeons. Therefore, this study reports on the experience of using endoscopic and laparoscopic full-thickness resection (ELFR) with laparoscopic two-layer suturing in such tumors.
MATERIALS AND METHODS
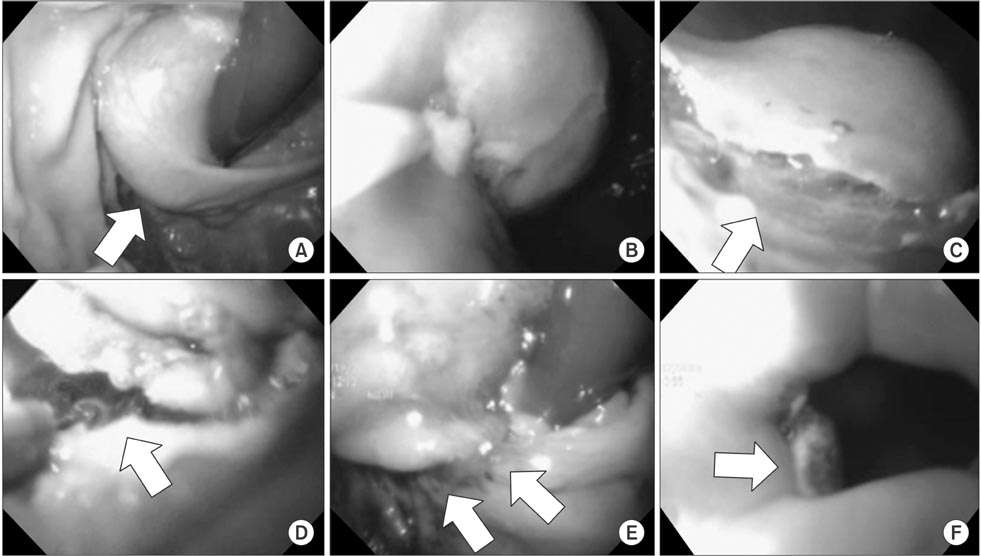
Six patients with gastric SMTs very close to the EGJ underwent ELFR with laparoscopic two-layer suturing at Kyungpook National University Medical Center. With the patient under general anesthesia, the lesser curvature and posterior aspect adjacent to the EGJ were meticulously dissected and visualized using a laparoscopic approach. A partially circumferential full-thickness incision at the distal margin of the tumor was then made using an endoscopic approach under laparoscopic guidance. The SMT was resected using laparoscopic ultrasonic shears, and the gastric wall was closed using two-layer suturing. Thereafter, the patency and any leakage were checked through endoscopy.
RESULTS
All the ELFR procedures with laparoscopic two-layer suturing were performed successfully without an open conversion. The mean operation time was 139.2+/-30.9 minutes and the blood loss was too minimal to be measured. The tumors from four patients were leiomyomas, while the tumors from the other two patients were gastrointestinal stromal tumors with clear resection margins. All the patients started oral intake on the third postoperative day. There was no morbidity or mortality. The mean hospital stay was 7.7+/-0.8 days.
CONCLUSIONS
ELFR with laparoscopic two-layer suturing is a safe treatment option for patients with an SMT close to the EGJ, as major resection of the stomach is avoided.
MeSH Terms
Figure
Cited by 1 articles
-
Endoscopic Full-Thickness Resection Combined with Laparoscopic Surgery
Chan Gyoo Kim
Clin Endosc. 2018;51(1):33-36. doi: 10.5946/ce.2017.153.
Reference
-
1. Hedenbro JL, Ekelund M, Wetterberg P. Endoscopic diagnosis of submucosal gastric lesions. The results after routine endoscopy. Surg Endosc. 1991; 5:20–23.2. Ponsaing LG, Kiss K, Hansen MB. Classification of submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007; 13:3311–3315.3. Berindoague R, Targarona EM, Feliu X, Artigas V, Balagué C, Aldeano A, et al. Laparoscopic resection of clinically suspected gastric stromal tumors. Surg Innov. 2006; 13:231–237.4. Novitsky YW, Kercher KW, Sing RF, Heniford BT. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg. 2006; 243:738–745. discussion 745-7475. Sexton JA, Pierce RA, Halpin VJ, Eagon JC, Hawkins WG, Linehan DC, et al. Laparoscopic gastric resection for gastrointestinal stromal tumors. Surg Endosc. 2008; 22:2583–2587.6. Sasaki A, Koeda K, Obuchi T, Nakajima J, Nishizuka S, Terashima M, et al. Tailored laparoscopic resection for suspected gastric gastrointestinal stromal tumors. Surgery. 2010; 147:516–520.7. Choi YB, Oh ST. Laparoscopy in the management of gastric submucosal tumors. Surg Endosc. 2000; 14:741–745.8. Abe N, Takeuchi H, Yanagida O, Masaki T, Mori T, Sugiyama M, et al. Endoscopic full-thickness resection with laparoscopic assistance as hybrid NOTES for gastric submucosal tumor. Surg Endosc. 2009; 23:1908–1913.9. Blay JY, Bonvalot S, Casali P, Choi H, Debiec-Richter M, Dei Tos AP, et al. GIST consensus meeting panelists. Consensus meeting for the management of gastrointestinal stromal tumors. Report of the GIST Consensus Conference of 20-21 March 2004, under the auspices of ESMO. Ann Oncol. 2005; 16:566–578.10. Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw. 2010; 8:Suppl 2. S1–S41. quiz S42-S4411. Nishida T, Hirota S, Yanagisawa A, Sugino Y, Minami M, Yamamura Y, et al. GIST Guideline Subcommittee. Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol. 2008; 13:416–430.12. Song KY, Kim SN, Park CH. Tailored-approach of laparoscopic wedge resection for treatment of submucosal tumor near the esophagogastric junction. Surg Endosc. 2007; 21:2272–2276.13. Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008; 22:1729–1735.14. Hwang SH, Park do J, Kim YH, Lee KH, Lee HS, Kim HH, et al. Laparoscopic surgery for submucosal tumors located at the esophagogastric junction and the prepylorus. Surg Endosc. 2009; 23:1980–1987.15. Shim JH, Lee HH, Yoo HM, Jeon HM, Park CH, Kim JG, et al. Intragastric approach for submucosal tumors located near the Z-line: a hybrid laparoscopic and endoscopic technique. J Surg Oncol. 2011; 104:312–315.16. Li QL, Yao LQ, Zhou PH, Xu MD, Chen SY, Zhong YS, et al. Submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a large study of endoscopic submucosal dissection (with video). Gastrointest Endosc. 2012; 75:1153–1158.17. Katoh T, Itoh Y, Mohri T, Suzuki H. Endoscopic enucleation of gastrointestinal stromal tumors of the stomach: report of five cases. World J Gastroenterol. 2008; 14:2609–2611.18. Kang YK, Kim KM, Sohn T, Choi D, Kang HJ, Ryu MH, et al. Korean GIST Study Group. Clinical practice guideline for accurate diagnosis and effective treatment of gastrointestinal stromal tumor in Korea. J Korean Med Sci. 2010; 25:1543–1552.19. Tagaya N, Mikami H, Kogure H, Kubota K, Hosoya Y, Nagai H. Laparoscopic intragastric stapled resection of gastric submucosal tumors located near the esophagogastric junction. Surg Endosc. 2002; 16:177–179.20. Sakamoto Y, Sakaguchi Y, Akimoto H, Chinen Y, Kojo M, Sugiyama M, et al. Safe laparoscopic resection of a gastric gastrointestinal stromal tumor close to the esophagogastric junction. Surg Today. 2012; 42:708–711.21. Abe N, Mori T, Takeuchi H, Ueki H, Yanagida O, Masaki T, et al. Successful treatment of early stage gastric cancer by laparoscopy-assisted endoscopic full-thickness resection with lymphadenectomy. Gastrointest Endosc. 2008; 68:1220–1224.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Gastric Wedge Resection and Prophylactic Antireflux Surgery for a Submucosal Tumor of Gastroesophageal Junction
- Endoscopic Full-thickness Resection for Gastric Tumor
- Choice of LECS Procedure for Benign and Malignant Gastric Tumors
- Endoscopic Treatment for Gastric Subepithelial Tumor
- Advancements in Endoscopic Treatment for Gastric Subepithelial Tumors