J Korean Neurosurg Soc.
2017 Sep;60(5):540-549. 10.3340/jkns.2016.0809.008.
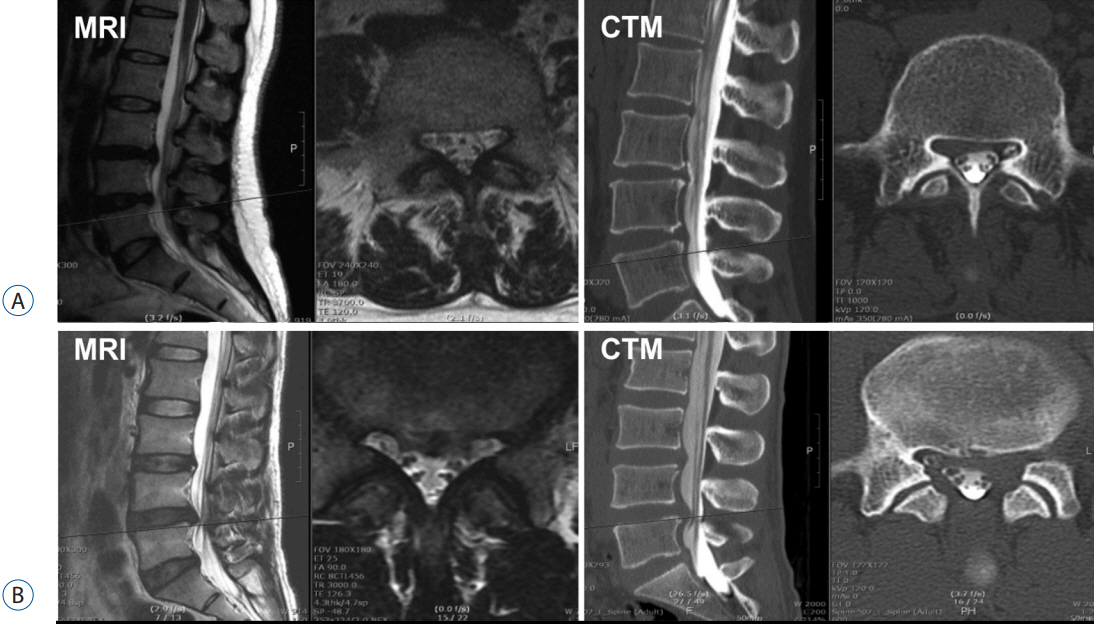
Comparison of Root Images between Post-Myelographic Computed Tomography and Magnetic Resonance Imaging in Patients with Lumbar Radiculopathy
- Affiliations
-
- 1Good Doctor Teun Teun Hospital, Anyang, Korea.
- 2Department of Neurosurgery, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea. kosailee73@gmail.com
- 3Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2457961
- DOI: http://doi.org/10.3340/jkns.2016.0809.008
Abstract
OBJECTIVE
To evaluate the diagnostic value of computed tomography-myelography (CTM) compared to that of magnetic resonance imaging (MRI) in patients with lumbar radiculopathy.
METHODS
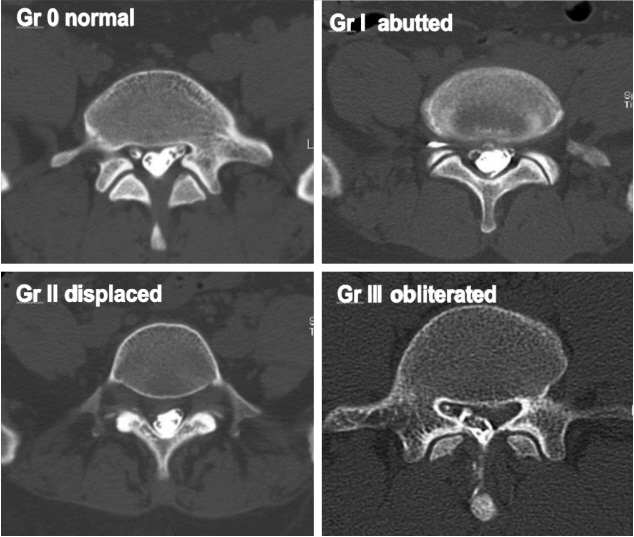
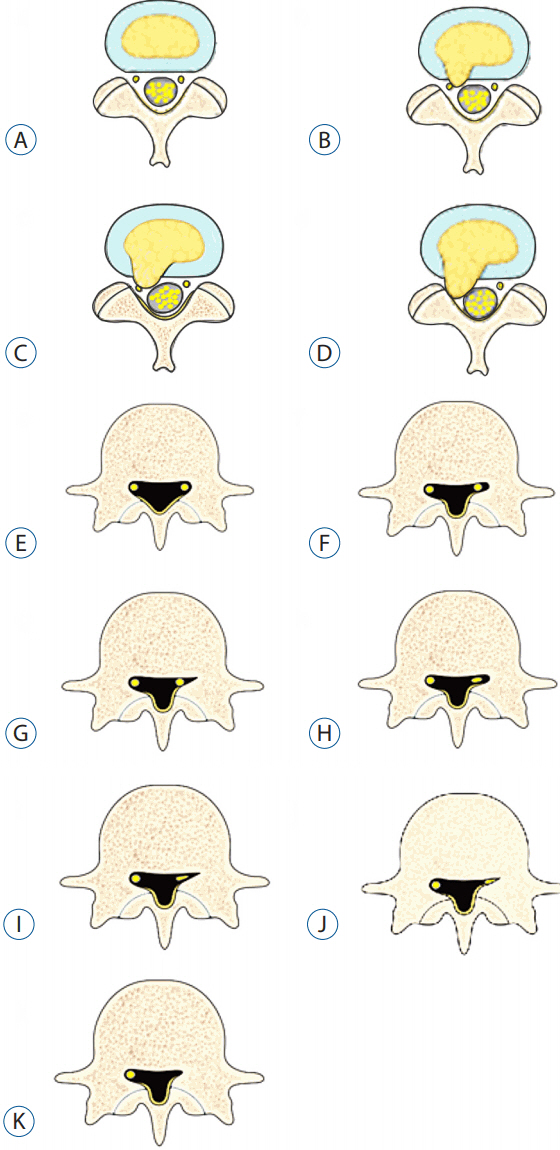
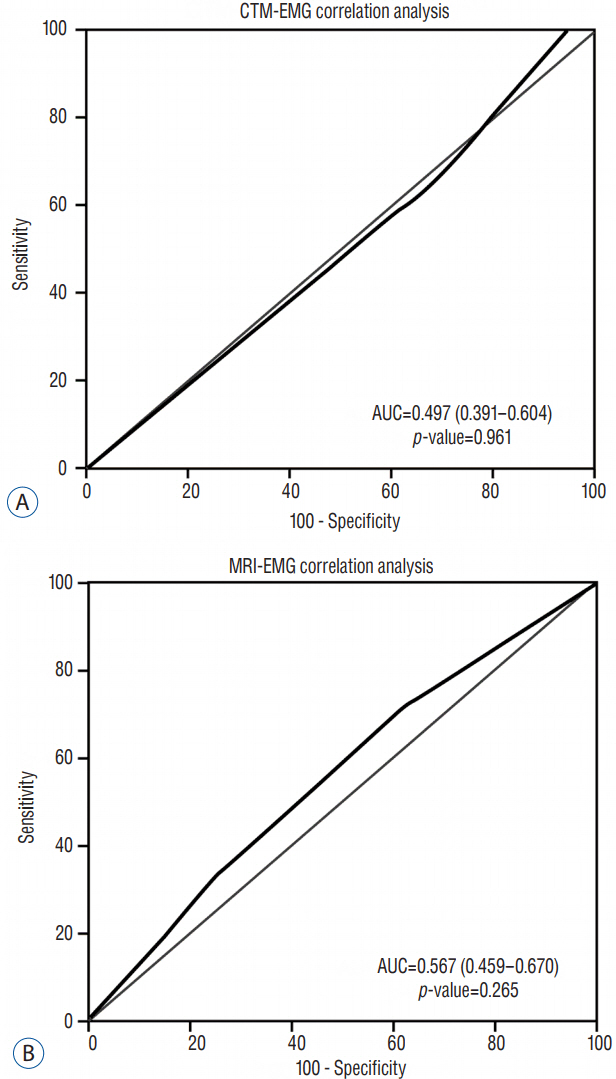
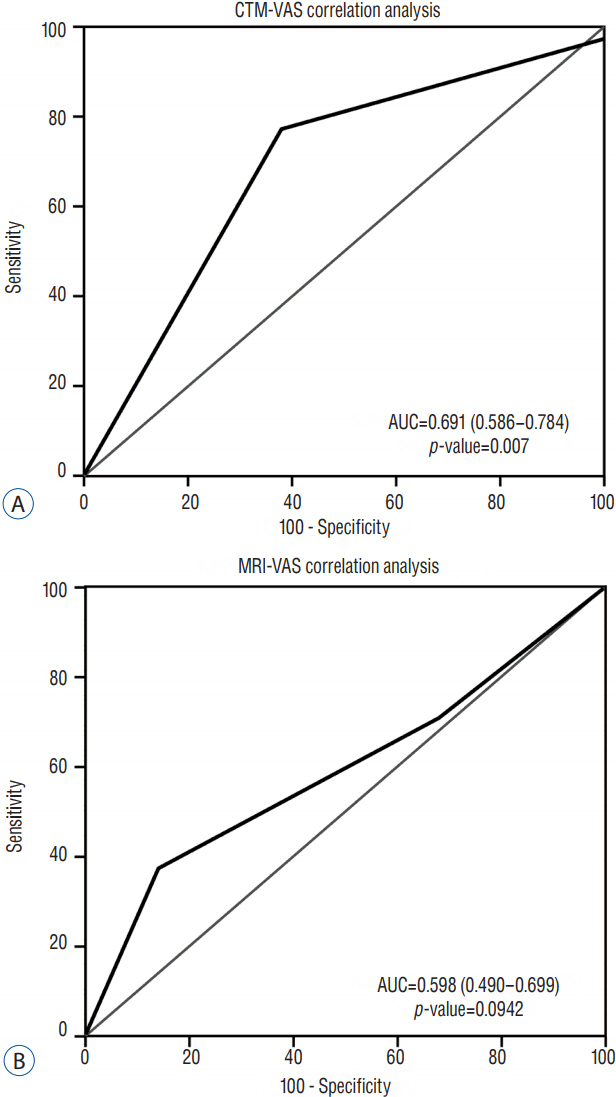
The study included 91 patients presenting with radicular leg pain caused by herniated nucleus pulposus or lateral recess stenosis in the lumbar spine. The degree of nerve root compression on MRI and CTM was classified into four grades. The results of each imaging modality as assessed by two different observers were compared. Visual analog scale score for pain and electromyography result were the clinical parameters used to evaluate the relationships between clinical features and nerve root compression grades on both MRI and CTM. These relationships were quantified by calculating the receiver-operating characteristic curves, and the degree of relationship was compared between MRI and CTM.
RESULTS
McNemar's test revealed that the two diagnostic modalities did not show diagnostic concurrence (p<0.0001). Electromyography results did not correlate with grades on either MRI or CTM. The visual analog pain scale score results were correlated better with changes of the grades on CTM than those on MRI (p=0.0007).
CONCLUSION
The present study demonstrates that CTM could better define the pathology of degenerative lumbar spine diseases with radiculopathy than MRI. CTM can be considered as a useful confirmative diagnostic tool when the exact cause of radicular pain in a patient with lumbar radiculopathy cannot be identified by using MRI. However, the invasiveness and potential complications of CTM are still considered to be pending questions to settle.
MeSH Terms
Figure
Reference
-
References
1. Bartynski WS, Lin L. Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR Am J Neuroradiol. 24:348–360. 2003.2. Bischoff RJ, Rodriquez RP, Gupta K, Righi A, Dalton JE, Whitecloud TS. A comparison of computed tomography-myelography, magnetic resonance imaging, and myelography in the diagnosis of herniated nucleus pulposus and spinal stenosis. J Spinal Disord. 6:289–295. 1993.
Article3. Botwin KP, Gruber RD. Lumbar spinal stenosis: anatomy and pathogenesis. Phys Med Rehabil Clin N Am. 14:1–15. v2003.
Article4. Breivik EK, Björnsson GA, Skovlund E. A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain. 16:22–28. 2000.
Article5. Burton CV, Kirkaldy-Willis WH, Yong-Hing K, Heithoff KB. Causes of failure of surgery on the lumbar spine. Clin Orthop Relat Res. 157:191–199. 1981.
Article6. Chiodo A, Haig AJ, Yamakawa KS, Quint D, Tong H, Choksi VR. Needle EMG has a lower false positive rate than MRI in asymptomatic older adults being evaluated for lumbar spinal stenosis. Clin Neurophysiol. 118:751–756. 2007.
Article7. Colosimo C, Gaudino S, Alexandre AM. Imaging in degenerative spine pathology. Acta Neurochir Suppl. 108:9–15. 2011.
Article8. Emch TM, Modic MT. Imaging of lumbar degenerative disk disease: history and current state. Skeletal Radiol. 40:1175–1189. 2011.
Article9. Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 26:E93–E113. 2001.10. Grams AE, Gempt J, Förschler A. Comparison of spinal anatomy between 3-Tesla MRI and CT-myelography under healthy and pathological conditions. Surg Radiol Anat. 32:581–585. 2010.
Article11. Greiner M, Pfeiffer D, Smith RD. Principals and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med. 45:23–41. 2000.
Article12. Harreld JH, McMenamy JM, Toomay SM, Chason DP. Myelography: a primer. Curr Probl Diagn Radiol. 40:149–157. 2011.
Article13. Jackson RP, Cain JE Jr, Jacobs RR, Cooper BR, McManus GE. The neuroradiographic diagnosis of lumbar herniated nucleus pulposus: II. A comparison of computed tomography (CT), myelography, CT-myelography, and magnetic resonance imaging. Spine (Phila Pa 1976). 14:1362–1367. 1989.
Article14. Janssen ME, Bertrand SL, Joe C, Levine MI. Lumbar herniated disk disease: comparison of MRI, myelography, and post-myelographic CT scan with surgical findings. Orthopedics. 17:121–127. 1994.
Article15. Jindal G, Pukenas B. Normal spinal anatomy on magnetic resonance imaging. Magn Reson Imaging Clin N Am. 19:475–488. 2011.
Article16. Kang SH, Choi SH, Seong NJ, Ko JM, Cho ES, Ko KP. Comparative study of lumbar magnetic resonance imaging and myelography in young soldiers with herniated lumbar disc. J Korean Neurosurg Soc. 48:501–505. 2010.
Article17. Kang YS, Kang JH, Kim MC, Yu BY, Sung EJ, Lee SY, et al. Cutoff of percent body fat to predict obesity and metabolic risk in children and adolescents: 2007 children and adolescent physical growth standard. Korean J Fam Med. 30:887–894. 2009.
Article18. Kent DL, Haynor DR, Larson EB, Deyo RA. Diagnosis of lumbar spinal stenosis in adults: a metaanalysis of the accuracy of CT, MR, and myelography. AJR Am J Roentgenol. 158:1135–1144. 1992.
Article19. Mondelli M, Aretini A, Arrigucci U, Ginanneschi F, Greco G, Sicurelli F. Clinical findings and electrodiagnostic testing in 108 consecutive cases of lumbosacral radiculopathy due to herniated disc. Neurophysiol Clin. 43:205–215. 2013.
Article20. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 230:583–588. 2004.
Article21. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 17:45–56. 1983.
Article22. Sandow BA, Donnal JF. Myelography complications and current practice patterns. AJR Am J Roentgenol. 185:768–771. 2005.
Article23. Song KJ, Choi BW, Kim GH, Kim JR. Clinical usefulness of CT-myelogram comparing with the MRI in degenerative cervical spinal disorders: is CTM still useful for primary diagnostic tool? J Spinal Disord Tech. 22:353–357. 2009.
Article24. Wildermuth S, Zanetti M, Duewell S, Schmid MR, Romanowski B, Benini A, et al. Lumbar spine: quantitative and qualitative assessment of positional (upright flexion and extension) MR imaging and myelography. Radiology. 207:391–398. 1998.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- L2 Radicular Compression Caused by a Foraminal Extradural Gas Pseudocyst
- Value of functional myelography with both lateral bending anterior-posterior views in lumbar radiculopathy
- Utility of Limited Protocol Magnetic Resonance Imaging Lumbar Spine for Nerve Root Compression in a Developing Country, Is It Accurate and Cost Effective?
- Image Study of the Lumbar Spine
- Ganglion Cyst in the Lumbar Anterior Epidural Space: A Case Report