Pediatr Gastroenterol Hepatol Nutr.
2019 Sep;22(5):453-459. 10.5223/pghn.2019.22.5.453.
Effect of Synbiotic on the Treatment of Jaundice in Full Term Neonates: A Randomized Clinical Trial
- Affiliations
-
- 1Razi Herbal Medicine Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran.
- 2Department of Pediatrics, Faculty of Medicine, Lorestan University of Medical Sciences, Khorramabad, Iran. dr.a.Mohsenzadeh@gmail.com
- 3Department of Social Medicine, School of Medicine, Lorestan University of Medical Sciences, Khorramabad, Iran.
- 4Pediatric Gastroenterology and Hepatology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
- 5Department of Pharmacology and Toxicology, Faculty of Pharmacy, Lorestan University of Medical Sciences, Khorramabad, Iran.
- KMID: 2457747
- DOI: http://doi.org/10.5223/pghn.2019.22.5.453
Abstract
- PURPOSE
Jaundice accounts for most hospital admissions in the neonatal period. Nowadays, in addition to phototherapy, other auxiliary methods are used to reduce jaundice and the length of hospitalization. This study aimed to investigate the effect of probiotics on the treatment of hyper-bilirubinemia in full-term neonates.
METHODS
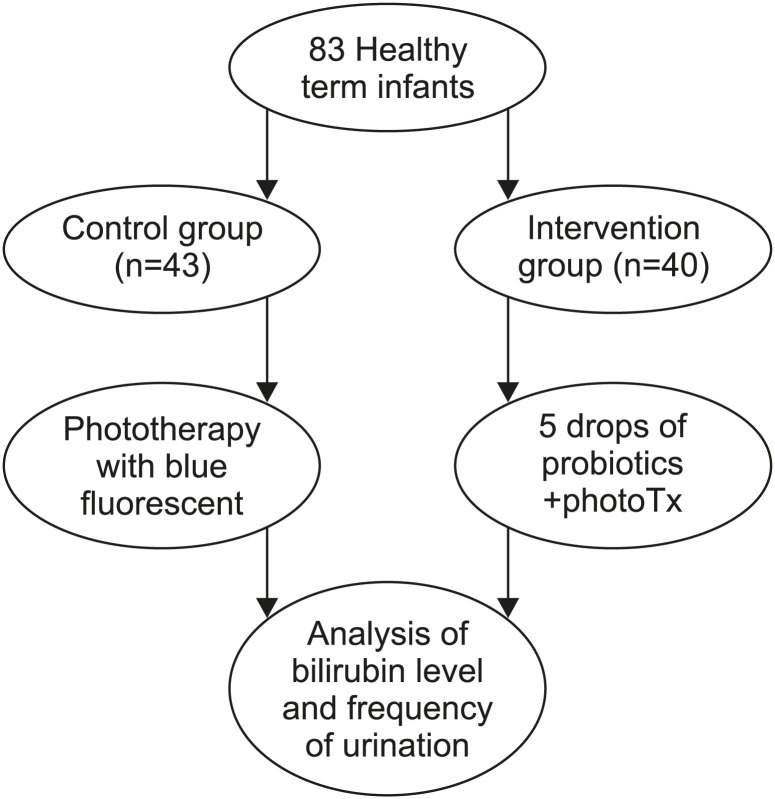
In this randomized clinical trial, 83 full-term neonates, who were admitted to the hospital to receive phototherapy in the first 6 months of 2015, were randomly divided into two groups: synbiotic (SG, n=40) and control (CG, n=43). Both groups received phototherapy but the SG also received 5 drops/day of synbiotics. Serum bilirubin, urine, stool, feeding frequency, and weight were measured daily until hospital discharge. A p-value<0.05 was considered statistically significant.
RESULTS
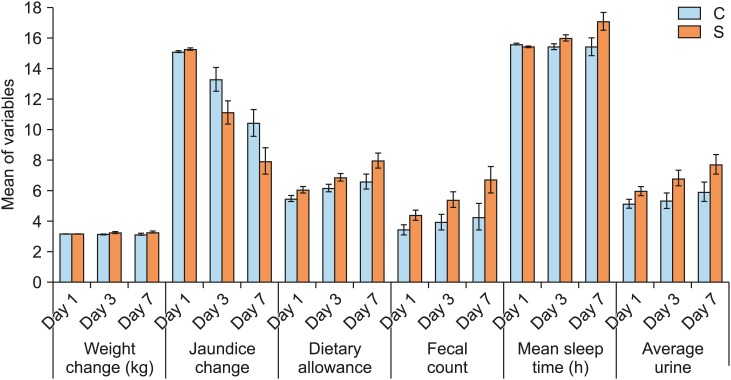
The mean total serum bilirubin in the SG was lower than that in the CG (9.38±2.37 and 11.17±2.60 mg/dL, respectively). The urine and stool frequency in the SG was significantly higher than that in the CG (p<0.05). The duration of hospitalization in the SG was shorter than that in the CG.
CONCLUSION
Use of synbiotics as an adjuvant therapy had a significant treatment effect on jaundice in full-term neonates. Further studies including larger samples with long follow-up periods are essential to confirm the benefits of routine use of synbiotics in neonatal patients with jaundice.
MeSH Terms
Figure
Reference
-
1. Alex M, Gallant DP. Toward understanding the connections between infant jaundice and infant feeding. J Pediatr Nur. 2008; 23:429–438.
Article2. Martin RJ, Fanaroff AA, Walsh WM. Fanaroff and Martin's neonatal perinatal medicine diseases of the fetus and infant. Philadelphia: Mosby;2006.3. Cohen SM. Jaundice in the full-term newborn. Pediatr Nurs. 2006; 32:202–208. PMID: 16802676.4. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004; 114:297–316. PMID: 15231951.5. Mahé E, Beauchet A, Aegerter P, Saiag P. Neonatal blue-light phototherapy does not increase nevus count in 9-year-old children. Pediatrics. 2009; 123:e896–e900. PMID: 19403483.6. McDonagh AF. Bilirubin, copper-porphyrins, and the bronze-baby syndrome. J Pediatr. 2011; 158:160–164. PMID: 20888578.
Article7. Bhutani VK, Johnson-Hamerman L. The clinical syndrome of bilirubin-induced neurologic dysfunction. Semin Fetal Neonatal Med. 2015; 20:6–13. PMID: 25577653.
Article8. McDonagh AF, Maisels MJ. Bilirubin unbound: déjà vu all over again? Pediatrics. 2006; 117:523–525. PMID: 16452373.9. Nag N, Halder S, Chaudhuri R, Adhikary S, Mazumder S. Role of bilirubin as antioxidant in neonatal jaundice and effect of ethanolic extract of sweet lime peel on experimentally induced jaundice in rat. Indian J Biochem Biophys. 2009; 46:73–78. PMID: 19374257.10. Stanton C, Gardiner G, Meehan H, Collins K, Fitzgerald G, Lynch PB, et al. Market potential for probiotics. Am J Clin Nutr. 2001; 73(2 Suppl):476S–483S. PMID: 11157361.
Article11. Cummings JH, Macfarlane GT, Macfarlane S. Intestinal bacteria and ulcerative colitis. Curr Issues Intest Microbiol. 2003; 4:9–20. PMID: 12691258.12. Salminen S, Bouley C, Boutron-Ruault MC, Cummings JH, Franck A, Gibson GR, et al. Functional food science and gastrointestinal physiology and function. Br J Nutr. 1998; 80 Suppl 1:S147–S71. PMID: 9849357.
Article13. Sur D, Manna B, Niyogi SK, Ramamurthy T, Palit A, Nomoto K, et al. Role of probiotic in preventing acute diarrhoea in children: a community-based, randomized, double-blind placebo-controlled field trial in an urban slum. Epidemiol Infect. 2011; 139:919–926. PMID: 20670468.
Article14. Prescott SL, Björkstén B. Probiotics for the prevention or treatment of allergic diseases. J Allergy Clin Immunol. 2007; 120:255–262. PMID: 17544096.
Article15. Hoyos AB. Reduced incidence of necrotizing enterocolitis associated with enteral administration of Lactobacillus acidophilus and Bifidobacterium infantis to neonates in an intensive care unit. Int J Infect Dis. 1999; 3:197–202. PMID: 10575148.
Article16. Maruo Y, Nishizawa K, Sato H, Sawa H, Shimada M. Prolonged unconjugated hyperbilirubinemia associated with breast milk and mutations of the bilirubin uridine diphosphate- glucuronosyltransferase gene. Pediatrics. 2000; 106:E59. PMID: 11061796.
Article17. Porter ML, Dennis BL. Hyperbilirubinemia in the term newborn. Am Fam Physician. 2002; 65:599–606. PMID: 11871676.18. Armanian AM, Barekatain B, Hoseinzadeh M, Salehimehr N. Prebiotics for the management of hyperbilirubinemia in preterm neonates. J Matern Fetal Neonatal Med. 2016; 29:3009–3013. PMID: 26513278.
Article19. Chen Z, Zhang L, Zeng L, Yang X, Jiang L, Gui G, et al. Probiotics supplementation therapy for pathological neonatal jaundice: a systematic review and meta-analysis. Front Pharmacol. 2017; 8:432. PMID: 28713275.
Article20. Deshmukh J, Deshmukh M, Patole S. Probiotics for the management of neonatal hyperbilirubinemia: a systematic review of randomized controlled trials. J Matern Fetal Neonatal Med. 2019; 32:154–163. PMID: 28823200.
Article21. Torkaman M, Afsharpaiman SH, Hoseini MJ, Moradi M, Mazraati A, Amirsalari S, et al. Platelet count and neonatal sepsis: a high prevalence of Enterobacter spp. Singapore Med J. 2009; 50:482–485. PMID: 19495516.22. Goldin BR, Gorbach SL. The relationship between diet and rat fecal bacterial enzymes implicated in colon cancer. J Natl Cancer Inst. 1976; 57:371–375. PMID: 1003518.23. Goldin BR, Gorbach SL. Effect of Lactobacillus acidophilus dietary supplements on 1,2-dimethylhydrazine dihydrochloride-induced intestinal cancer in rats. J Natl Cancer Inst. 1980; 64:263–265. PMID: 6766509.24. Osborn LM, Reiff MI, Bolus R. Jaundice in the full-term neonate. Pediatrics. 1984; 73:520–525. PMID: 6709433.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study of Nosocomial Infection of Rotavirus in Preterm and Full-term Neonates
- Comparison of Purgative Manna Drop and Phototherapy with Phototherapy Treatment of Neonatal Jaundice: A Randomized Double-Blind Clinical Trial
- Combination of synbiotic and sitagliptin in nonalcoholic fatty liver disease: Is it better than sitagliptin alone?
- Intracranial hemorrhage in full-term neonates by ultrasonography
- Readmission in Neonatal Period among the Normal Full-term Neonates