Neonatal Med.
2019 Aug;26(3):147-154. 10.5385/nm.2019.26.3.147.
Clinical or Radiological Findings Suggestive of Spontaneous Intestinal Perforation in Extremely Low Birth Weight Infants with Gasless Abdomen
- Affiliations
-
- 1Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea. ychang@dankook.ac.kr
- 2Department of Pediatric Radiology, Dankook University College of Medicine, Cheonan, Korea.
- 3Department of Pediatric Surgery, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2457182
- DOI: http://doi.org/10.5385/nm.2019.26.3.147
Abstract
- PURPOSE
This study aimed to evaluate the clinical and radiologic findings suggestive of spontaneous intestinal perforation (SIP) in extremely-low-birth-weight infants (ELBWIs) with persistent gasless abdomen, and to investigate the usefulness of abdominal ultrasonography for the diagnosis of SIP.
METHODS
In total, 22 infants with birth weights less than 1,000 g who showed persistent gasless abdomen on simple abdominal radiography were included. Perinatal, neonatal, and perioperative clinical findings were retrospectively reviewed, and the risk factors for intestinal perforation were evaluated. Abdominal sonographic findings suggestive of intestinal perforation were also identified, and postoperative short-term outcomes were evaluated.
RESULTS
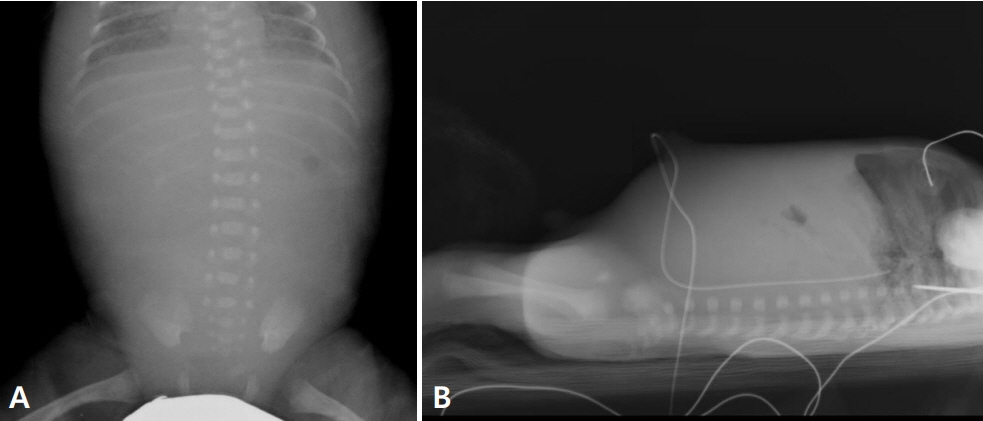
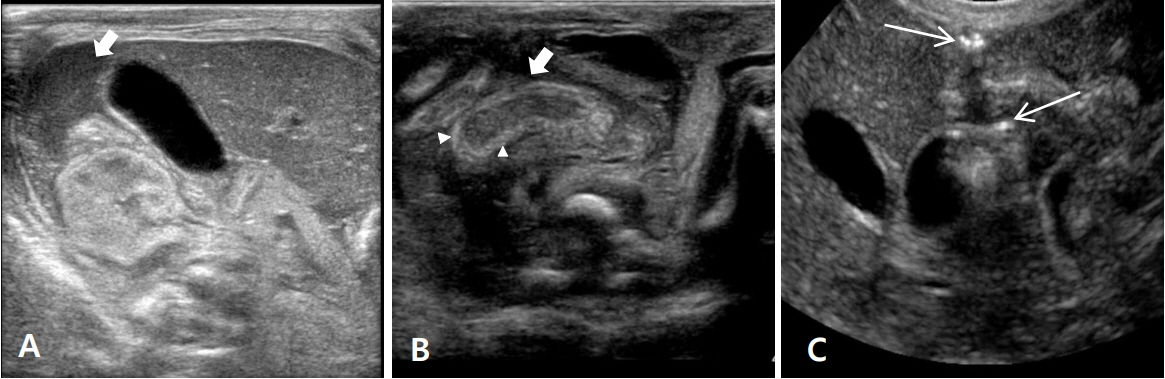
In total, eight of the 22 infants (36.4%) with gasless abdomen had SIP. The number of infants with patent ductus arteriosus who were treated with intravenous ibuprofen or indomethacin was significantly higher in the SIP group than in the non-SIP group (P<0.05). Greenish or red gastric residue, abdominal distension, or decreased bowel sound were more frequent in infants with SIP (P<0.05), in addition to gray or bluish discoloration of abdomen, suggestive of meconium peritonitis (P<0.05). Pneumoperitoneum on simple abdominal radiography was found in only one of the eight infants (12.5%) with SIP. Intramural echogenicity and echogenic extramural material on abdominal ultrasonography were exclusively observed in infants with SIP. Four infants (50%) with SIP died after surgical intervention.
CONCLUSION
Intestinal perforation may occur in ELBWIs with gasless abdomen. As intramural echogenicity and extraluminal echogenic materials on abdominal ultrasonography are indicative of SIP, this technique could be useful for diagnosing SIP.
MeSH Terms
-
Abdomen*
Birth Weight
Diagnosis
Ductus Arteriosus, Patent
Humans
Ibuprofen
Indomethacin
Infant*
Infant, Extremely Low Birth Weight
Infant, Low Birth Weight*
Infant, Newborn
Intestinal Perforation*
Meconium
Peritonitis
Pneumoperitoneum
Radiography, Abdominal
Retrospective Studies
Risk Factors
Ultrasonography
Ibuprofen
Indomethacin
Figure
Reference
-
1. Fischer A, Vachon L, Durand M, Cayabyab RG. Ultrasound to diagnose spontaneous intestinal perforation in infants weighing ≤ 1000 g at birth. J Perinatol. 2015; 35:104–9.2. Miller SF, Seibert JJ, Kinder DL, Wilson AR. Use of ultrasound in the detection of occult bowel perforation in neonates. J Ultrasound Med. 1993; 12:531–5.3. Attridge JT, Herman AC, Gurka MJ, Griffin MP, McGahren ED, Gordon PV. Discharge outcomes of extremely low birth weight infants with spontaneous intestinal perforations. J Perinatol. 2006; 26:49–54.4. Pumberger W, Mayr M, Kohlhauser C, Weninger M. Spontaneous localized intestinal perforation in very-low-birth-weight infants: a distinct clinical entity different from necrotizing enterocolitis. J Am Coll Surg. 2002; 195:796–803.5. Mintz AC, Applebaum H. Focal gastrointestinal perforations not associated with necrotizing enterocolitis in very low birth weight neonates. J Pediatr Surg. 1993; 28:857–60.6. Adderson EE, Pappin A, Pavia AT. Spontaneous intestinal perforation in premature infants: a distinct clinical entity associated with systemic candidiasis. J Pediatr Surg. 1998; 33:1463–7.7. Seibert JJ, Williamson SL, Golladay ES, Mollitt DL, Seibert RW, Sutterfield SL. The distended gasless abdomen: a fertile field for ultrasound. J Ultrasound Med. 1986; 5:301–8.8. Oretti C, Bussani R, Janes A, Demarini S. Multiple segmental absence of intestinal musculature presenting as spontaneous isolated perforation in an extremely low-birth-weight infant. J Pediatr Surg. 2010; 45:E25–7.9. Kubota A, Yamanaka H, Okuyama H, Shiraishi J, Kawahara H, Hasegawa T, et al. Focal intestinal perforation in extremelylow-birth-weight neonates: etiological consideration from histological findings. Pediatr Surg Int. 2007; 23:997–1000.10. Dzieniecka M, Grzelak-Krzymianowska A, Kulig A. Segmental congenital defect of the intestinal musculature. Pol J Pathol. 2010; 61:94–6.11. Kang J, Im IJ, Lee DS, Go JH, Chang YP. A case of spontaneous focal Intestinal perforation due to defect of the intestinal musculature. J Korean Soc Neonatol. 2006; 13:180–3.12. Buyuktiryaki M, Kanmaz HG, Okur N, Ates U, Sirvan AL, Uras N. Segmental absence of intestinal muscle with ileal web in an extremely low birth weight infant: case report. Arch Argent Pediatr. 2016; 114:e108–10.13. Gordon PV. Understanding intestinal vulnerability to perforation in the extremely low birth weight infant. Pediatr Res. 2009; 65:138–44.14. Tatekawa Y, Muraji T, Imai Y, Nishijima E, Tsugawa C. The mechanism of focal intestinal perforations in neonates with low birth weight. Pediatr Surg Int. 1999; 15:549–52.15. Meyer CL, Payne NR, Roback SA. Spontaneous, isolated intestinal perforations in neonates with birth weight less than 1,000 g not associated with necrotizing enterocolitis. J Pediatr Surg. 1991; 26:714–7.16. Choi SY, Choi IJ, Kim SM, Jung JH, Kim GH, Son CM. Spontaneous ileal perforation in very low birth weight infant without evidence of necrotizing enterocolitis. J Korean Soc Neonatol. 2004; 11:77–80.17. Shah TA, Meinzen-Derr J, Gratton T, Steichen J, Donovan EF, Yolton K, et al. Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation. J Perinatol. 2012; 32:552–8.18. Gordon PV, Attridge JT. Understanding clinical literature relevant to spontaneous intestinal perforations. Am J Perinatol. 2009; 26:309–16.19. Jakaitis BM, Bhatia AM. Definitive peritoneal drainage in the extremely low birth weight infant with spontaneous intestinal perforation: predictors and hospital outcomes. J Perinatol. 2015; 35:607–11.20. Tiwari C, Sandlas G, Jayaswal S, Shah H. Spontaneous intestinal perforation in neonates. J Neonatal Surg. 2015; 4:14.21. Holland AJ, Shun A, Martin HC, Cooke-Yarborough C, Holland J. Small bowel perforation in the premature neonate: congenital or acquired? Pediatr Surg Int. 2003; 19:489–94.22. Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (2) two populations of patients with perforations. J Perinatol. 2006; 26:185–8.23. Gordon PV, Young ML, Marshall DD. Focal small bowel perforation: an adverse effect of early postnatal dexamethasone therapy in extremely low birth weight infants. J Perinatol. 2001; 21:156–60.24. Paquette L, Friedlich P, Ramanathan R, Seri I. Concurrent use of indomethacin and dexamethasone increases the risk of spontaneous intestinal perforation in very low birth weight neonates. J Perinatol. 2006; 26:486–92.25. Attridge JT, Clark R, Gordon PV. New insights into spontaneous intestinal perforation using a national data set (3): antenatal steroids have no adverse association with spontaneous intestinal perforation. J Perinatol. 2006; 26:667–70.26. Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (1) SIP is associated with early indomethacin exposure. J Perinatol. 2006; 26:93–9.27. Tatli MM, Kumral A, Duman N, Demir K, Gurcu O, Ozkan H. Spontaneous intestinal perforation after oral ibuprofen treatment of patent ductus arteriosus in two very-low-birthweight infants. Acta Paediatr. 2004; 93:999–1001.28. Shah J, Singhal N, da Silva O, Rouvinez-Bouali N, Seshia M, Lee SK, et al. Intestinal perforation in very preterm neonates: risk factors and outcomes. J Perinatol. 2015; 35:595–600.29. Buchheit JQ, Stewart DL. Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics. 1994; 93:32–6.30. Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR, et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg. 2005; 241:984–9.31. Gebus M, Michel JL, Samperiz S, Harper L, Alessandri JL, Ramful D. Management of neonatal spontaneous intestinal perforation by peritoneal needle aspiration. J Perinatol. 2018; 38:159–63.32. Rao SC, Basani L, Simmer K, Samnakay N, Deshpande G. Peritoneal drainage versus laparotomy as initial surgical treatment for perforated necrotizing enterocolitis or spontaneous intestinal perforation in preterm low birth weight infants. Cochrane Database Syst Rev. 2011; (6):CD006182.33. Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK, et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics. 2006; 117:e680–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Meconium Obstruction Syndrome in Two Extremely Low Birth Weight Infants
- Spontaneous Ileal Perforation in Very Low Birth Weight Infant without Evidence of Necrotizing Enterocolitis
- A Case of Intestinal Perforation with Candida Infection in Extremely Low Birth Weight Infant
- Usefulness of peritoneal drainage in extremely low birth weight infants with intestinal perforation: a single-center experience
- A Survival Case of a 630 gram Extremely Low Birth Weight Neonate after Surgery for the Small Bowel Perforation