J Korean Acad Nurs.
2019 Aug;49(4):375-385. 10.4040/jkan.2019.49.4.375.
A Structural Model for Chemotherapy Related Cognitive Impairment and Quality of Life in Breast Cancer Patients
- Affiliations
-
- 1Department of Nursing, Korea Cancer Center Hospital, Seoul, Korea.
- 2Department of Nursing, Sahmyook University, Seoul, Korea. ohpj@syu.ac.kr
- KMID: 2456142
- DOI: http://doi.org/10.4040/jkan.2019.49.4.375
Abstract
- PURPOSE
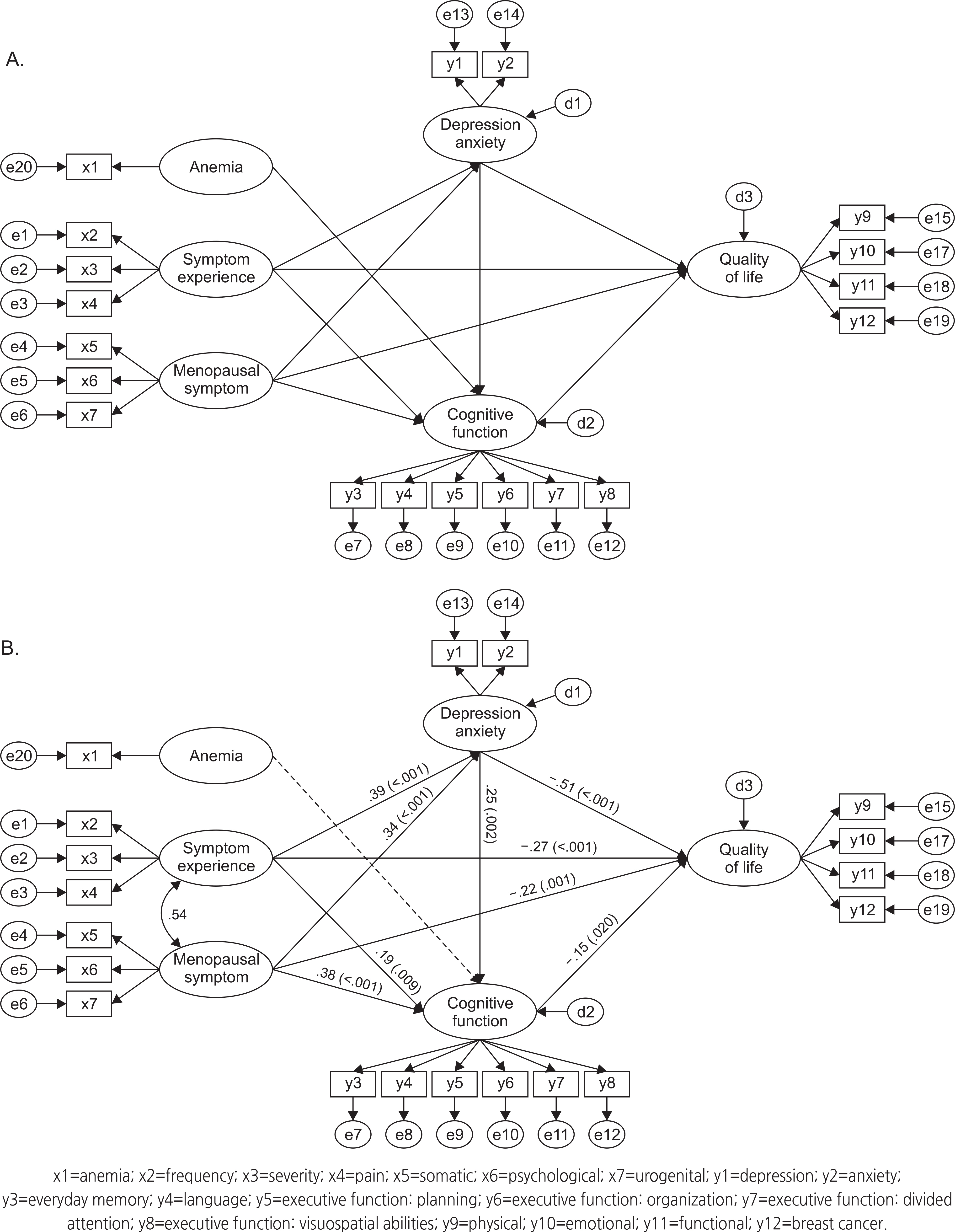
This study aimed to develop and test a structural model for chemotherapy-related cognitive impairment of breast cancer patients based on a literature review and Hess and Insel's chemotherapy-related cognitive change model.
METHODS
The Participants consisted of 250 patients who were ≥19 years of age. The assessment tools included the Menopause Rating Scale, Symptom Experience Scale, Hospital Anxiety and Depression Scale, Everyday Cognition, and Functional Assessment of Cancer Therapy-Breast Cancer. Data were analyzed using the SPSS 21.0 and AMOS 21.0 programs.
RESULTS
The modified model was a good fit for the data. The model fit indices were χ2=423.18 (p<.001), χ2/df=3.38, CFI=.91, NFI=.91, TLI=.89, SRMR=.05, RMSEA=.09, and AIC=515.18. Chemotherapy-related cognitive impairment was directly influenced by menopausal symptoms (β=.38, p=.002), depression and anxiety (β=.25, p=.002), and symptom experiences (β=.19, p=.012). These predictors explained 47.7% of the variance in chemotherapy-related cognitive impairment. Depression and anxiety mediated the relations among menopausal symptoms, symptom experiences, and with chemotherapy related cognitive impairment. Depression and anxiety (β=−.51, p=.001), symptom experiences (β=−.27, p=.001), menopausal symptoms (β=−.22, p=.008), and chemotherapy-related cognitive impairment (β=−.15, p=.024) had direct effects on the quality of life and these variables explained 91.3%.
CONCLUSION
These results suggest that chemotherapy-related toxicity is highly associated with cognitive decline and quality of life in women with breast cancer. Depression and anxiety increased vulnerability to cognitive impairment after chemotherapy. Nursing intervention is needed to relieve chemotherapy-related toxicity and psychological factor as well as cognitive decline for quality of life in patients undergoing chemotherapy.
MeSH Terms
Figure
Reference
-
References
1. Korea Breast Cancer Society. 2015 Breast cancer facts & figures [Internet]. Seoul: Korea Breast Cancer Society;c2015. [cited 2018 Jul 5]. Available from:. http://www.kbcs.or.kr/journal/file/2015_Breast_Cancer_Facts_and_Figures_updated.pdf.2. Brem S, Kumar NB. Management of treatment-related symptoms in patients with breast cancer. Clinical Journal of Oncology Nursing. 2011; 15(1):63–71. https://doi.org/10.1188/11.CJON.63-71.
Article3. Calvio L, Peugeot M, Bruns GL, Todd BL, Feuerstein M. Measures of cognitive function and work in occupationally active breast cancer survivors. Journal of Occupational and Environmental Medicine. 2010; 52(2):219–227. https://doi.org/10.1097/JOM.0b013e3181d0bef7.
Article4. Wefel JS, Saleeba AK, Buzdar AU, Meyers CA. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer. 2010; 116(14):3348–3356. https://doi.org/10.1002/cncr.25098.
Article5. Schagen SB, Muller MJ, Boogerd W, Mellenbergh GJ, van Dam FSAM. Change in cognitive function after chemotherapy: A prospective longitudinal study in breast cancer patients. Journal of the National Cancer Institute. 2006; 98(23):1742–1745. https://doi.org/10.1093/jnci/djj470.
Article6. Nelson CJ, Nandy N, Roth AJ. Chemotherapy and cognitive deficits: Mechanisms, findings, and potential interventions. Palliative & Supportive Care. 2007; 5(3):273–280. https://doi.org/10.1017/S1478951507000442.
Article7. Biglia N, Moggio G, Peano E, Sgandurra P, Ponzone R, Nappi RE, et al. Effects of surgical and adjuvant therapies for breast cancer on sexuality, cognitive functions, and body weight. The Journal of Sexual Medicine. 2010; 7(5):1891–1900. https://doi.org/10.1111/j.1743-6109.2010.01725.x.
Article8. Hess LM, Insel KC. Chemotherapy-related change in cognitive function: A conceptual model. Oncology Nursing Forum. 2007; 34(5):981–994. https://doi.org/10.1188/07.ONF.981-994.
Article9. Vardy J, Tannock I. Cognitive function after chemotherapy in adults with solid tumours. Critical Reviews in Oncology/Hema-tology. 2007; 63(3):183–202. https://doi.org/10.1016/j.critrevonc.2007.06.001.
Article10. Weiss B. Evaluation of multiple neurotoxic outcomes in cancer chemotherapy. Raffa RB, Tallarida RJ, editors. Chemo Fog. Advances in Experimental Medicine and Biology, vol 678. New York: Springer;2010. p. 96–112. https://doi.org/10.1007/978-1-4419-6306-2_13.
Article11. Biegler KA, Chaoul MA, Cohen L. Cancer, cognitive impairment, and meditation. Acta Oncologica. 2009; 48(1):18–26. https://doi.org/10.1080/02841860802415535.
Article12. Von Ah D, Russell KM, Storniolo AM, Carpenter JS. Cognitive dysfunction and its relationship to quality of life in breast cancer survivors. Oncology Nursing Forum. 2009; 36(3):326–336. https://doi.org/10.1188/09.ONF.326-334.
Article13. Vearncombe KJ, Rolfe M, Wright M, Pachana NA, Andrew B, Beadle G. Predictors of cognitive decline after chemotherapy in breast cancer patients. Journal of the International Neuropsychological Society. 2009; 15(6):951–962. https://doi.org/10.1017/S1355617709990567.
Article14. Sarenmalm EK, Öhlén J, Jonsson T, Gaston-Johansson F. Coping with recurrent breast cancer: Predictors of distressing symptoms and health-related quality of life. Journal of Pain and Symptom Management. 2007; 34(1):24–39. https://doi.org/10.1016/j.jpainsymman.2006.10.017.
Article15. Bishop S, Duncan J, Brett M, Lawrence AD. Prefrontal cortical function and anxiety: Controlling attention to threat-related stimuli. Nature Neuroscience. 2004; 7(2):184–188. https://doi.org/10.1038/nn1173.
Article16. Woo JP. Understanding and concepts of structural equation model. Seoul: Hannarae Publishing Co.;2012. p. 275–377.17. Samarel N, Leddy SK, Greco K, Cooley ME, Torres SC, Tulman L, et al. Development and testing of the symptom experience scale. Journal of Pain and Symptom Management. 1996; 12(4):221–228. https://doi.org/10.1016/0885-3924(96)00150-9.
Article18. Chae MJ. A structural model for sexual function of patients with breast cancer [dissertation]. Gwangju: Chonnam National University;2012. p. 1–133.19. Heinemann K, Ruebig A, Potthoff P, Schneider HPG, Strelow F, Heinemann LAJ, et al. The menopause rating scale (MRS) scale: A methodological review. Health and Quality of Life Outcomes. 2004; 2:45. https://doi.org/10.1186/1477-7525-2-45.20. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983; 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Article21. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: A comparison of normal, depressed and anxious groups. Journal of the Korean Neuropsychiatric Association. 1999; 38(2):289–296.22. Farias ST, Mungas D, Reed BR, Cahn-Weiner D, Jagust W, Baynes K, et al. The measurement of everyday cognition (ECog): Scale development and psychometric properties. Neuropsychology. 2008; 22(4):531–544. https://doi.org/10.1037/0894-4105.22.4.531.
Article23. Chung BY, Cho EJ. Correlates influencing cognitive impairment in breast cancer patients receiving chemotherapy. Asian Oncology Nursing. 2012; 12(3):221–229. https://doi.org/10.5388/aon.2012.12.3.221.
Article24. Yoo HJ, Ahn SH, Eremenco S, Kim H, Kim WK, Kim SB, et al. Korean translation and validation of the functional assessment of cancer therapy-breast (FACT-B) scale version 4. Quality of Life Research. 2005; 14(6):1627–1632. https://doi.org/10.1007/s11136-004-7712-1.
Article25. Henderson VW. Cognitive changes after menopause: Influence of estrogen. Clinical Obstetrics and Gynecology. 2008; 51(3):618–626. https://doi.org/10.1097/GRF.0b013e318180ba10.
Article26. Oppermann K, Fuchs SC, Donato G, Bastos CA, Spritzer PM. Physical, psychological, and menopause-related symptoms and minor psychiatric disorders in a community-based sample of Brazilian premenopausal, perimenopausal, and postmenopausal women. Menopause. 2012; 19(3):355–360. https://doi.org/10.1097/gme.0b013e31822ba026.
Article27. Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA. The cognitive sequelae of standard‐dose adjuvant chemotherapy in women with breast carcinoma: Results of a prospective, randomized, longitudinal trial. Cancer. 2004; 100(11):2292–2299. https://doi.org/10.1002/cncr.20272.28. Collins B, Mackenzie J, Stewart A, Bielajew C, Verma S. Cognitive effects of chemotherapy in post‐menopausal breast cancer patients 1 year after treatment. Psycho-Oncology. 2009; 18(2):134–143. https://doi.org/10.1002/pon.1379.
Article29. Lee JR, Oh PJ. Cognitive decline and quality of life among patients with breast cancer undergoing chemotherapy: The mediating effect of health promotion behavior. Korean Journal of Adult Nursing. 2016; 28(2):202–212. https://doi.org/10.7475/kjan.2016.28.2.202.
Article30. Kim JH, Oh PJ. Menopause symptoms and perceived cognitive decline in menopausal women: The mediating effect of health promotion behavior. Korean Journal of Adult Nursing. 2017; 29(2):200–210. https://doi.org/10.7475/kjan.2017.29.2.200.
Article31. Hutchinson AD, Hosking JR, Kichenadasse G, Mattiske JK, Wilson C. Objective and subjective cognitive impairment following chemotherapy for cancer: A systematic review. Cancer Treatment Reviews. 2012; 38(7):926–934. https://doi.org/10.1016/j.ctrv.2012.05.002.
Article32. Kim HJ, Kim S, Lee H, Oh SE. Factors affecting symptom experiences of breast cancer patients: Based on the theory of unpleasant symptoms. Asian Oncology Nursing. 2014; 14(1):7–14. https://doi.org/10.5388/aon.2014.14.1.7.
Article33. Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: A review of epidemiology and treatment. General Hospital Psychiatry. 2008; 30(2):112–126. https://doi.org/10.1016/j.genhosppsych.2007.10.008.
Article34. Kim KH, Chung BY, Kim GD, Byun HS, Choi EH, Cho EJ. Cognitive function in breast cancer patients receiving adjuvant chemotherapy. Asian Oncology Nursing. 2012; 12(1):1–11. https://doi.org/10.5388/aon.2012.12.1.1.
Article35. Byun HS, Kim GD. Impacts of fatigue, pain, anxiety, and depression on the quality of life in patients with breast cancer. Asian Oncology Nursing. 2012; 12(1):27–34. https://doi.org/10.5388/aon.2012.12.1.27.
Article36. Luckett T, King MT, Butow PN, Oguchi M, Rankin N, Price MA, et al. Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: Issues, evidence and recommendations. Annals of Oncology. 2011; 22(10):2179–2190. https://doi.org/10.1093/annonc/mdq721.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlates Influencing Cognitive Impairment in Breast Cancer Patients receiving Chemotherapy
- The Experience of Chemotherapy Related Cognitive Impairment in Patients with Cancer
- A Meta-analysis of Chemotherapy related Cognitive Impairment in Patients with Breast Cancer
- Research Trends on Cancer-Related Cognitive Impairment in Patients with Non-Central Nervous System Cancer: Text Network Analysis and Topic Modeling
- Impact of Cognitive Function and Cancer Coping on Quality of Life among Women with Post-chemotherapy Breast Cancer