Hip Pelvis.
2019 Sep;31(3):136-143. 10.5371/hp.2019.31.3.136.
Surgical Outcomes of Internal Fixation Using Multiple Screws in Femoral Neck Fractures with Valgus Impaction: When Should We Consider Hip Arthroplasty? A Retrospective, Multicenter Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Bio-Medical Research Institute, Pusan National University Hospital, Busan, Korea. kuentak@pusan.ac.kr
- 2Department of Orthopedic Surgery, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2455986
- DOI: http://doi.org/10.5371/hp.2019.31.3.136
Abstract
- PURPOSE
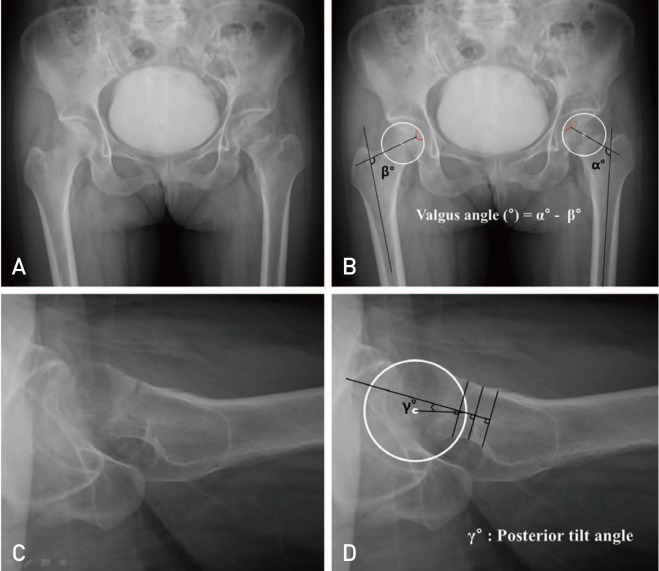
We analyzed the surgical outcomes at two institutions after internal fixation using multiple screws in femoral neck fractures with valgus impaction to determine independent predictors and their cut-off values for nonunion and reoperation.
MATERIALS AND METHODS
Between January 2006 and December 2016, 104 femoral neck fractures with valgus impaction that underwent internal fixation using multiple screws from two institutions were enrolled. The multiple logistic regression model and receiver operating characteristics analysis were used to determine the independent predictors and cut-off values for nonunion and reoperation.
RESULTS
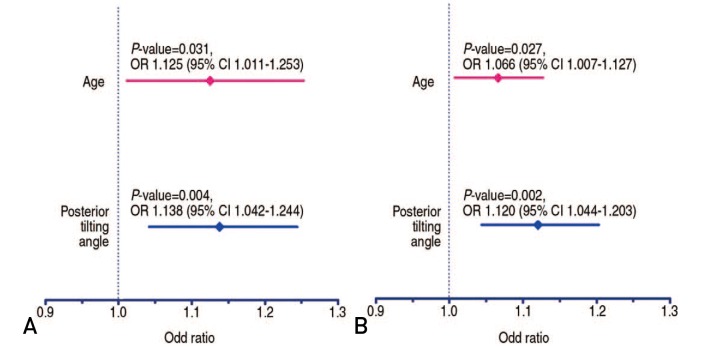
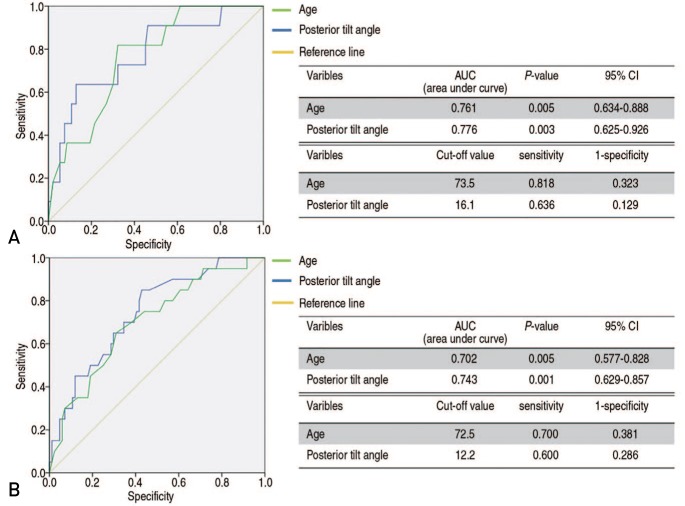
There were 20 reoperations (19.2%) due to 11 nonunions (10.6%) and nine cases of femoral head osteonecrosis (8.7%). Multiple logistic regression analysis revealed that independent predictors of nonunion and reoperation were age and posterior tilt angle (P<0.05). The cut-off value for age and the posterior tilt angle for reoperation were 72.5 years and 12.2°, respectively. The patients with a posterior tilt angle of greater than 13° had poorer radiological and clinical outcomes compared with those with a posterior tilt angle of less than 13°, even though they did achieve bone union.
CONCLUSION
Primary hip arthroplasty should be considered in patients older than 73 years of age with a posterior tilt angle greater than 13°.
MeSH Terms
Figure
Reference
-
1. Hoelsbrekken SE, Dolatowski FC. The influence of the hips position on measurements of posterior tilt in a valgus-impacted femoral neck fracture. Injury. 2017; 48:2184–2188. PMID: 28859846.
Article2. Kim YC, Lee JY, Song JH, Oh S. The result of in situ pinning for valgus impacted femoral neck fractures of patients over 70 years old. Hip Pelvis. 2014; 26:263–268. PMID: 27536591.3. Rodríguez-Merchán EC. In situ fixation of nondisplaced intracapsular fractures of the proximal femur. Clin Orthop Relat Res. 2002; (399):42–51. PMID: 12011693.4. Palm H, Gosvig K, Krasheninnikoff M, Jacobsen S, Gebuhr P. A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year. Acta Orthop. 2009; 80:303–307. PMID: 19634021.5. Song HK, Lee JJ, Oh HC, Yang KH. Clinical implication of subgrouping in valgus femoral neck fractures: comparison of 31-B1.1 with 31-B1.2 fractures using the OTA/AO classification. J Orthop Trauma. 2013; 27:677–682. PMID: 23454857.6. Shimizu T, Miyamoto K, Masuda K, et al. The clinical significance of impaction at the femoral neck fracture site in the elderly. Arch Orthop Trauma Surg. 2007; 127:515–521. PMID: 17541613.
Article7. Stockton DJ, Lefaivre KA, Deakin DE, et al. Incidence, magnitude, and predictors of shortening in young femoral neck fractures. J Orthop Trauma. 2015; 29:e293–e298. PMID: 26226462.
Article8. Liu Y, Ai ZS, Shao J, Yang T. Femoral neck shortening after internal fixation. Acta Orthop Traumatol Turc. 2013; 47:400–404. PMID: 24509219.
Article9. Dolatowski FC, Adampour M, Frihagen F, Stavem K, Erik Utva°g S, Hoelsbrekken SE. Preoperative posterior tilt of at least 20° increased the risk of fixation failure in Garden-I and -II femoral neck fractures. Acta Orthop. 2016; 87:252–256. PMID: 26937557.
Article10. Sung YB, Jung EY, Kim KI, Kim SY. Risk factors for neck shortening in patients with valgus impacted femoral neck fractures treated with three parallel screws: is bone density an affecting factor? Hip Pelvis. 2017; 29:277–285. PMID: 29250503.
Article11. Kemker B, Magone K, Owen J, Atkinson P, Martin S, Atkinson T. A sliding hip screw augmented with 2 screws is biomechanically similar to an inverted triad of cannulated screws in repair of a Pauwels type-III fracture. Injury. 2017; 48:1743–1748. PMID: 28511967.
Article12. Yang YH, Wang YR, Jiang SD, Jiang LS. Proximal femoral nail antirotation and third-generation Gamma nail: which is a better device for the treatment of intertrochanteric fractures? Singapore Med J. 2013; 54:446–450. PMID: 24005451.
Article13. Sidi A, Lobato EB, Cohen JA. The American Society of Anesthesiologists’ Physical Status: category V revisited. J Clin Anesth. 2000; 12:328–334. PMID: 10960208.
Article14. Yoon PW, Shin YH, Yoo JJ, Yoon KS, Kim HJ. Progression of a fracture site impaction as a prognostic indicator of impacted femoral neck fracture treated with multiple pinning. Clin Orthop Surg. 2012; 4:66–71. PMID: 22379557.
Article15. Alho A, Benterud JG, Solovieva S. Internally fixed femoral neck fractures. Early prediction of failure in 203 elderly patients with displaced fractures. Acta Orthop Scand. 1999; 70:141–144. PMID: 10366914.
Article16. Min BW, Bae KC, Kang CH, Song KS, Kim SY, Won YY. Valgus intertrochanteric osteotomy for non-union of femoral neck fracture. Injury. 2006; 37:786–790. PMID: 16765958.
Article17. Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004; 86:1711–1716. PMID: 15292419.
Article18. Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008; 64:163–169. PMID: 18188116.
Article19. Chammout GK, Mukka SS, Carlsson T, Neander GF, Stark AW, Skoldenberg OG. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Joint Surg Am. 2012; 94:1921–1928. PMID: 23014835.20. Barenius B, Inngul C, Alagic Z, Enocson A. A randomized controlled trial of cemented versus cementless arthroplasty in patients with a displaced femoral neck fracture: a four-year follow-up. Bone Joint J. 2018; 100:1087–1093. PMID: 30062941.21. Bartels S, Gjertsen JE, Frihagen F, Rogmark C, Utva°g SE. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop. 2018; 89:53–58. PMID: 28914130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Valgus Deformity and Progression of Ostheoarthritis in Non-Displaced Femoral Neck Fractures
- The Result of In Situ Pinning for Valgus Impacted Femoral Neck Fractures of Patients over 70 Years Old
- Internal Fixation of Pauwels Type-3 Undisplacedincomplete Insufficiency Femoral Neck Fractures with Cephalomedullary Nails
- Femoral Neck Fracture
- Risk Factors for Neck Shortening in Patients with Valgus Impacted Femoral Neck Fractures Treated with Three Parallel Screws: Is Bone Density an Affecting Factor?