Anesth Pain Med.
2019 Jul;14(3):280-287. 10.17085/apm.2019.14.3.280.
Postoperative pain control by ultrasound guided brachial plexus block reduces emergence delirium in pediatric patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chungnam National University Hospital, Daejeon, Korea. limtwo2@gmail.com
- 2Department of Anesthesiology and Pain Medicine, Chungnam National University College of Medicine, Daejeon, Korea.
- 3Department of Orthopedic Surgery, Chungnam National University College of Medicine, Daejeon, Korea.
- KMID: 2454812
- DOI: http://doi.org/10.17085/apm.2019.14.3.280
Abstract
- BACKGROUND
Pediatric patients awakening from general anesthesia may experience emergence delirium (ED), often due to inadequate pain control. Nerve block completely inhibits innervation of the surgical site and is superior to systemic analgesics. This study assessed whether pain control through nerve block relieves ED after general anesthesia.
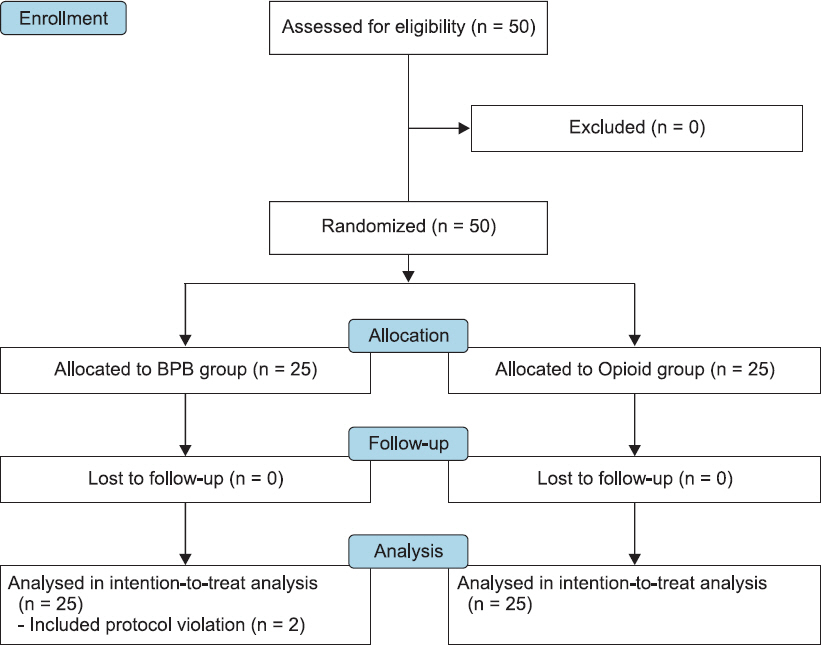
METHODS
Fifty patients aged 2-7 years with humerus condyle fractures were randomly assigned to receive ultrasound guided supraclavicular brachial plexus block (BPB group) or intravenous fentanyl (Opioid group). The primary outcome was score on the pediatric anesthesia emergence delirium (PAED) scale on arrival at the postanesthesia care unit (PACU). Secondary outcomes were severity of agitation and pain in the PACU, the incidence of ED, and postoperative administration of rescue analgesics over 24 h.
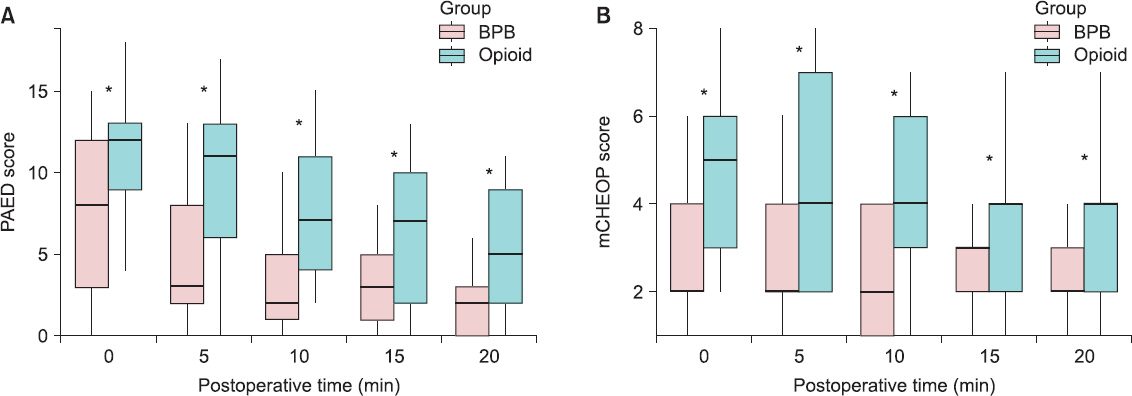
RESULTS
PAED scale was significantly lower in the BPB group at arrival in the PACU (7.2 ± 4.9 vs. 11.6 ± 3.2; mean difference [95% confidence interval (CI)] = 4.4 [2.0-6.8], P < 0.001) and at all other time points. The rate of ED was significantly lower in the BPB group (36% vs. 72%; relative risk [95% CI] = 0.438 [0.219-0.876], P = 0.023). The BPB group also had significantly lower pain scores and requiring rescue analgesics than Opioid group in the PACU.
CONCLUSIONS
Ultrasound guided BPB, which is a good option for postoperative acute phase pain control, also contributes to reducing the severity and incidence of ED.
MeSH Terms
Figure
Reference
-
1. Vlajkovic GP, Sindjelic RP. Emergence delirium in children:many questions, few answers. Anesth Analg. 2007; 104:84–91. DOI: 10.1213/01.ane.0000250914.91881.a8. PMID: 17179249.2. Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997; 87:1298–300. DOI: 10.1097/00000542-199712000-00006. PMID: 9416712.3. Aouad MT, Nasr VG. Emergence agitation in children:an update. Curr Opin Anaesthesiol. 2005; 18:614–9. DOI: 10.1097/01.aco.0000188420.84763.35. PMID: 16534301.4. Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004; 99:1648–54. DOI: 10.1213/01.ANE.0000136471.36680.97. PMID: 15562048.5. Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002; 94:1178–81. DOI: 10.1097/00000539-200205000-00023. PMID: 11973185.6. Cohen IT, Hannallah RS, Hummer KA. The incidence of emergence agitation associated with desflurane anesthesia in children is reduced by fentanyl. Anesth Analg. 2001; 93:88–91. DOI: 10.1097/00000539-200107000-00019. PMID: 11429345.7. Taenzer AH, Walker BJ, Bosenberg AT, Martin L, Suresh S, Polaner DM, et al. Asleep versus awake:does it matter?:pediatric regional block complications by patient state:a report from the Pediatric Regional Anesthesia Network. Reg Anesth Pain Med. 2014; 39:279–83. DOI: 10.1097/AAP.0000000000000102. PMID: 24918334.8. Taenzer A, Walker BJ, Bosenberg AT, Krane EJ, Martin LD, Polaner DM, et al. Interscalene brachial plexus blocks under general anesthesia in children:is this safe practice?:a report from the Pediatric Regional Anesthesia Network (PRAN). Reg Anesth Pain Med. 2014; 39:502–5. DOI: 10.1097/AAP.0000000000000166. PMID: 25304482.9. Lam DK, Corry GN, Tsui BC. Evidence for the use of ultrasound imaging in pediatric regional anesthesia:a systematic review. Reg Anesth Pain Med. 2016; 41:229–41. DOI: 10.1097/AAP.0000000000000208. PMID: 25675289.10. Polaner DM, Taenzer AH, Walker BJ, Bosenberg A, Krane EJ, Suresh S, et al. Pediatric Regional Anesthesia Network (PRAN):a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012; 115:1353–64. DOI: 10.1213/ANE.0b013e31825d9f4b. PMID: 22696610.11. Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004; 100:1138–45. DOI: 10.1097/00000542-200405000-00015. PMID: 15114210.12. Hong B, Lim CS, Kim YH, Lee JU, Kim YM, Jung C, et al. Comparison of topical ropivacaine with and without ketamine on post-surgical pain in children undergoing tonsillectomy:a randomized controlled double-blind study. J Anesth. 2017; 31:559–64. DOI: 10.1007/s00540-017-2353-z. PMID: 28409242.13. Kim HS, Kim CS, Kim SD, Lee JR. Fascia iliaca compartment block reduces emergence agitation by providing effective analgesic properties in children. J Clin Anesth. 2011; 23:119–23. DOI: 10.1016/j.jclinane.2010.08.007. PMID: 21377075.14. Wells LT, Rasch DK. Emergence “delirium” after sevoflurane anesthesia: a paranoid delusion? Anesth Analg. 1999; 88:1308–10. DOI: 10.1097/00000539-199906000-00020. PMID: 10357335.15. Cravero J, Surgenor S, Whalen K. Emergence agitation in paediatric patients after sevoflurane anaesthesia and no surgery:a comparison with halothane. Paediatr Anaesth. 2000; 10:419–24. DOI: 10.1046/j.1460-9592.2000.00560.x. PMID: 10886700.16. Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane-and desflurane-related emergence agitation in children:a meta-analysis of published studies. Br J Anaesth. 2010; 104:216–23. DOI: 10.1093/bja/aep376. PMID: 20047899.17. Locatelli BG, Ingelmo PM, Emre S, Meroni V, Minardi C, Frawley G, et al. Emergence delirium in children:a comparison of sevoflurane and desflurane anesthesia using the Paediatric Anesthesia Emergence Delirium scale. Paediatr Anaesth. 2013; 23:301–8. DOI: 10.1111/pan.12038. PMID: 23043512.18. Aouad MT, Kanazi GE, Siddik-Sayyid SM, Gerges FJ, Rizk LB, Baraka AS. Preoperative caudal block prevents emergence agitation in children following sevoflurane anesthesia. Acta Anaesthesiol Scand. 2005; 49:300–4. DOI: 10.1111/j.1399-6576.2005.00642.x. PMID: 15752392.19. Kim MS, Moon BE, Kim H, Lee JR. Comparison of propofol and fentanyl administered at the end of anaesthesia for prevention of emergence agitation after sevoflurane anaesthesia in children. Br J Anaesth. 2013; 110:274–80. DOI: 10.1093/bja/aes382. PMID: 23103775.20. Shi F, Xiao Y, Xiong W, Zhou Q, Yang P, Huang X. Effects of fentanyl on emergence agitation in children under sevoflurane anesthesia:meta-analysis of randomized controlled trials. PLoS One. 2015; 10:e0135244. DOI: 10.1371/journal.pone.0135244. PMID: 26275039. PMCID: PMC4537096.21. Pacifici GM. Clinical pharmacology of fentanyl in preterm infants. A review. Pediatr Neonatol. 2015; 56:143–8. DOI: 10.1016/j.pedneo.2014.06.002. PMID: 25176283.22. Vittinghoff M, Lönnqvist PA, Mossetti V, Heschl S, Simic D, Colovic V, et al. Postoperative pain management in children:guidance from the pain committee of the European Society for Paediatric Anaesthesiology (ESPA Pain Management Ladder Initiative). Paediatr Anaesth. 2018; 28:493–506. DOI: 10.1111/pan.13373. PMID: 29635764.23. Pande R, Pande M, Bhadani U, Pandey CK, Bhattacharya A. Supraclavicular brachial plexus block as a sole anaesthetic technique in children:an analysis of 200 cases. Anaesthesia. 2000; 55:798–802. DOI: 10.1046/j.1365-2044.2000.01330.x. PMID: 10947696.24. Suresh S, Schaldenbrand K, Wallis B, De Oliveira GS Jr. Regional anaesthesia to improve pain outcomes in paediatric surgical patients:a qualitative systematic review of randomized controlled trials. Br J Anaesth. 2014; 113:375–90. DOI: 10.1093/bja/aeu156. PMID: 24907283.25. Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Paediatr Anaesth. 2010; 20:704–11. DOI: 10.1111/j.1460-9592.2010.03328.x. PMID: 20497353.26. Lundblad M, Marhofer D, Eksborg S, Lönnqvist PA. Dexmedetomidine as adjunct to ilioinguinal/iliohypogastric nerve blocks for pediatric inguinal hernia repair:an exploratory randomized controlled trial. Paediatr Anaesth. 2015; 25:897–905. DOI: 10.1111/pan.12704. PMID: 26095747.27. Park JH, Lim BG, Kim HZ, Kong MH, Lim SH, Kim NS, et al. Comparison of emergence agitation between sevoflurane/nitrous oxide administration and sevoflurane administration alone in children undergoing adenotonsillectomy with preemptive ketorolac. Korean J Anesthesiol. 2014; 66:34–8. DOI: 10.4097/kjae.2014.66.1.34. PMID: 24567811. PMCID: PMC3926999.28. Yang Y, Song T, Wang H, Gu K, Ma P, Ma X, et al. Comparison of two different sevoflurane expelling methods on emergence agitation in infants following sevoflurane anesthesia. Int J Clin Exp Med. 2015; 8:6200–5. PMID: 26131225. PMCID: PMC4483804.29. Hwang BY, Kwon JY, Kim SY, Lee DW, Hong JM, Kim E. The change of sevoflurane to desflurane after anesthesia induction induces rapid emergence without increased cardiovascular responses and emergence delirium in pediatric strabismus surgery patients. Anesth Pain Med. 2015; 10:128–33. DOI: 10.17085/apm.2015.10.2.128.30. Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration:updated guidelines for reporting parallel group randomised trials. BMJ. 2010; 340:c869. DOI: 10.1136/bmj.c869. PMID: 20332511. PMCID: PMC2844943.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided Continuous Axillary Brachial Plexus Block Using a Nerve Stimulating Catheter: EpiStim(R) Catheter
- Bilateral variant locations of the musculocutaneous nerve during ultrasound-guided bilateral axillary brachial plexus block: A case report
- Cases series: ultrasound-guided supraclavicular block in 105 patients
- Comparison of Axillary and Supraclavicular Approach in Ultrasound-Guided Brachial Plexus Block
- Ultrasound Guided Low Approach Interscalene Brachial Plexus Block for Upper Limb Surgery