Cancer Res Treat.
2016 Apr;48(2):641-649. 10.4143/crt.2014.326.
Second Primary Cancer after Diagnosis and Treatment of Cervical Cancer
- Affiliations
-
- 1Gynecologic Cancer Branch, National Cancer Center, Goyang, Korea.
- 2Center for Uterine Cancer, National Cancer Center, Goyang, Korea.
- 3Cancer Registration and Statistics Branch, National Cancer Center, Goyang, Korea. astra67@ncc.re.kr
- 4Center for Breast Cancer, National Cancer Center, Goyang, Korea.
- 5Center for Colorectal Cancer, National Cancer Center, Goyang, Korea.
- KMID: 2454342
- DOI: http://doi.org/10.4143/crt.2014.326
Abstract
- PURPOSE
This study was conducted to investigate the incidence and survival outcomes of second primary cancers after the diagnosis of cervical cancer.
MATERIALS AND METHODS
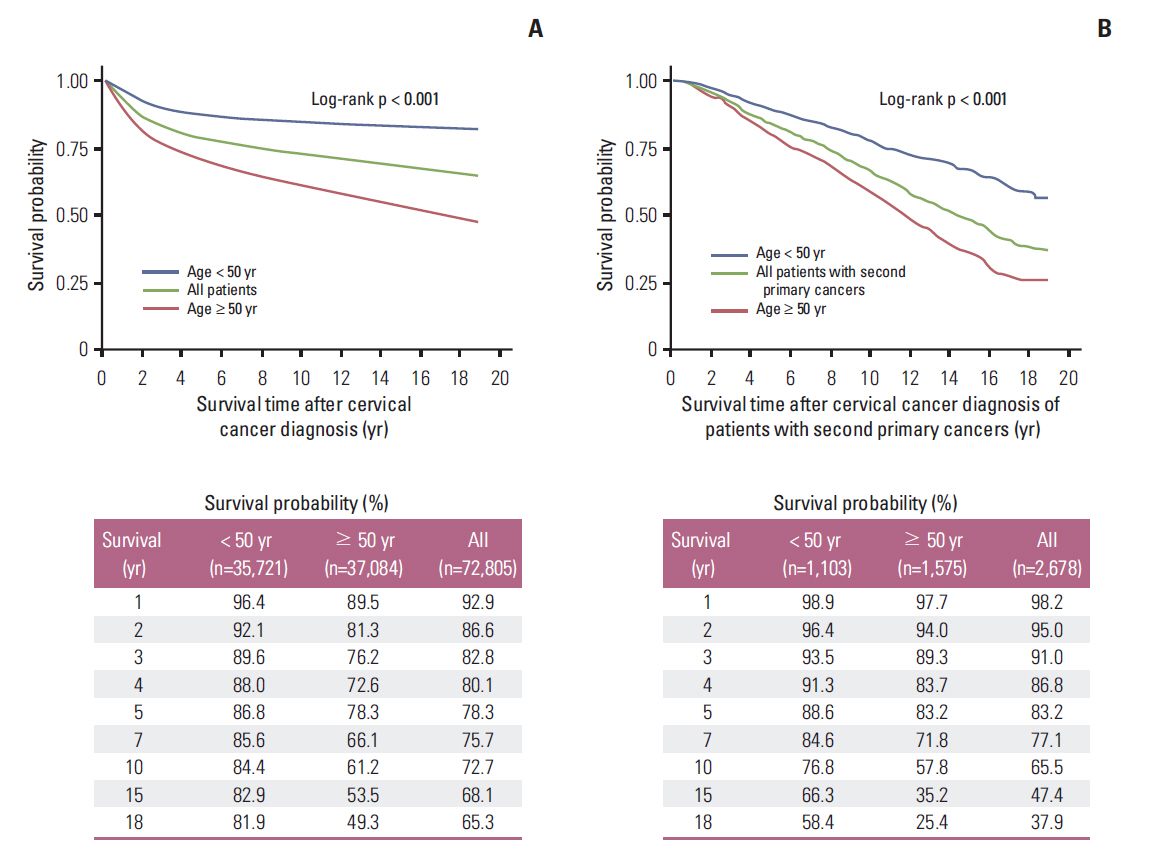
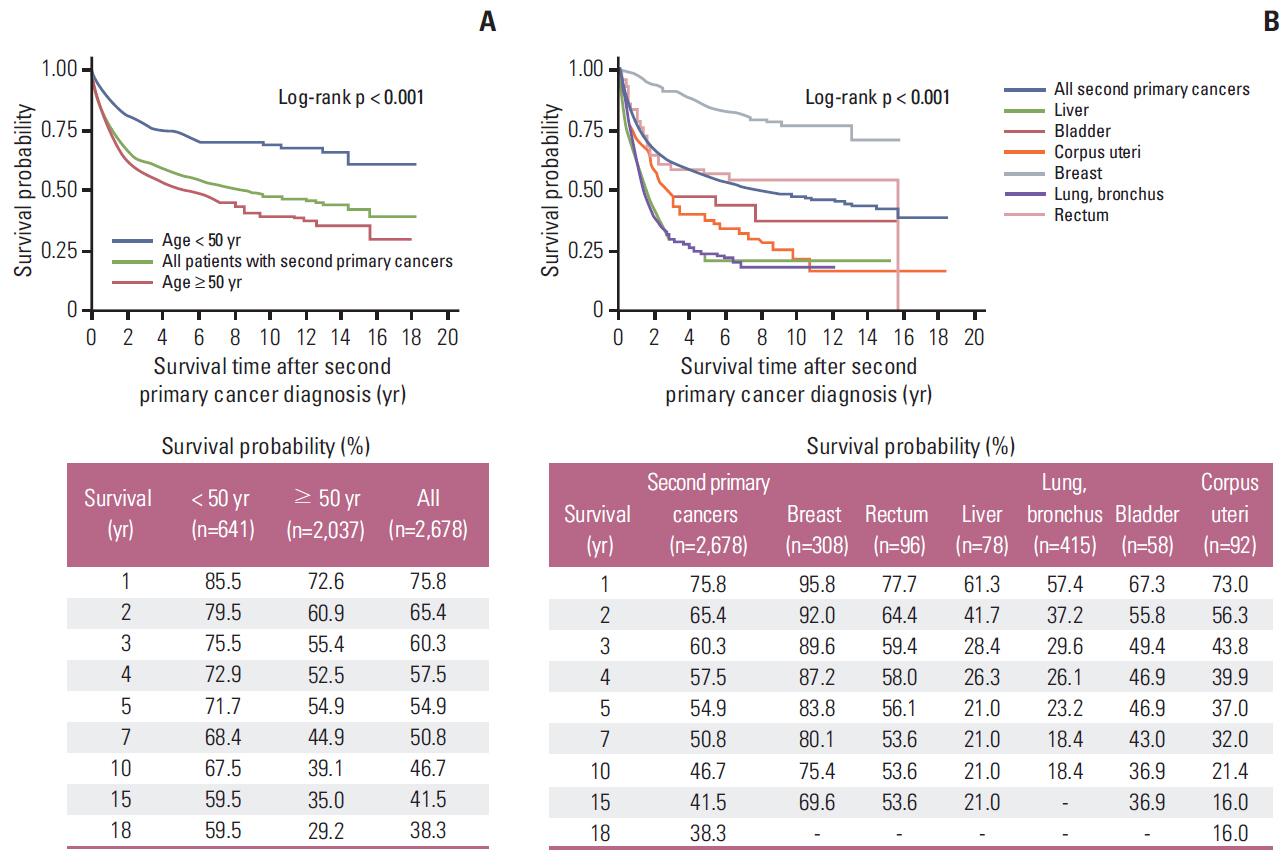
Data from the Korea Central Cancer Registry between 1993 and 2010 were reviewed and analyzed. Standardized incidence ratios (SIRs) of second primary cancers among women with cervical cancer were analyzed. Kaplan-Meier survival curves were constructed for cervical cancer patients with or without a second primary cancer.
RESULTS
Among 72,805 women with cervical cancer, 2,678 (3.68%) developed a second primary cancer within a mean follow-up period of 7.34 years. The overall SIR for a second cancer was 1.08 (95% confidence interval, 1.04 to 1.12). The most frequent sites of second primary cancers were the vagina, bone and joints, vulva, anus, bladder, lung and bronchus, corpus uteri, and esophagus. However, the incidence rates of four second primary cancers (breast, rectum, liver, and brain) were decreased. The 5-year and 10-year overall survival rates were 78.3% and 72.7% in all women with cervical cancer, and for women with a second primary cancer, these rates were 83.2% and 65.5% from the onset of cervical cancer and 54.9% and 46.7% from the onset of the second primary cancer, respectively.
CONCLUSION
The incidence rates of second primary cancers were increased in women with cervical cancer compared to the general population, with the exception of four decreasing cancers. The 10-year overall survival rates were decreased in cervical cancer patients with a second primary cancer.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013; 63:11–30.
Article2. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Prediction of cancer incidence and mortality in Korea, 2013. Cancer Res Treat. 2013; 45:15–21.
Article3. Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012; 30 Suppl 5:F12–23.
Article4. Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013; 24:298–302.
Article5. Le Borgne G, Mercier M, Woronoff AS, Guizard AV, Abeilard E, Caravati-Jouvenceaux A, et al. Quality of life in long-term cervical cancer survivors: a population-based study. Gynecol Oncol. 2013; 129:222–8.
Article6. Kleinerman RA, Boice JD Jr, Storm HH, Sparen P, Andersen A, Pukkala E, et al. Second primary cancer after treatment for cervical cancer: an international cancer registries study. Cancer. 1995; 76:442–52.
Article7. Kleinerman RA, Smith SA, Holowaty E, Hall P, Pukkala E, Vaalavirta L, et al. Radiation dose and subsequent risk for stomach cancer in long-term survivors of cervical cancer. Int J Radiat Oncol Biol Phys. 2013; 86:922–9.
Article8. Chaturvedi AK, Engels EA, Gilbert ES, Chen BE, Storm H, Lynch CF, et al. Second cancers among 104,760 survivors of cervical cancer: evaluation of long-term risk. J Natl Cancer Inst. 2007; 99:1634–43.
Article9. Chen CY, Lai CH, Lee KD, Huang SH, Dai YM, Chen MC. Risk of second primary malignancies in women with cervical cancer: a population-based study in Taiwan over a 30-year period. Gynecol Oncol. 2012; 127:625–30.
Article10. Boice JD Jr, Blettner M, Kleinerman RA, Stovall M, Moloney WC, Engholm G, et al. Radiation dose and leukemia risk in patients treated for cancer of the cervix. J Natl Cancer Inst. 1987; 79:1295–311.11. Fisher G, Harlow SD, Schottenfeld D. Cumulative risk of second primary cancers in women with index primary cancers of uterine cervix and incidence of lower anogenital tract cancers, Michigan, 1985-1992. Gynecol Oncol. 1997; 64:213–23.
Article12. Nakano T, Kato S, Ohno T, Tsujii H, Sato S, Fukuhisa K, et al. Long-term results of high-dose rate intracavitary brachytherapy for squamous cell carcinoma of the uterine cervix. Cancer. 2005; 103:92–101.
Article13. Ota T, Takeshima N, Tabata T, Hasumi K, Takizawa K. Treatment of squamous cell carcinoma of the uterine cervix with radiation therapy alone: long-term survival, late complications, and incidence of second cancers. Br J Cancer. 2007; 97:1058–62.
Article14. Tominaga K, Koyama Y, Sasagawa M, Obata N, Kamata H, Yamaguchi E, et al. A follow-up study of patients with cervical cancer after resection, with special emphasis on the incidence of second primary cancers. Gynecol Oncol. 1995; 56:71–4.
Article15. Underwood JM, Rim SH, Fairley TL, Tai E, Stewart SL. Cervical cancer survivors at increased risk of subsequent tobaccorelated malignancies, United States 1992-2008. Cancer Causes Control. 2012; 23:1009–16.
Article16. Moorman PG, Myers ER, Schildkraut JM, Iversen ES, Wang F, Warren N. Effect of hysterectomy with ovarian preservation on ovarian function. Obstet Gynecol. 2011; 118:1271–9.
Article17. Hwang JH, Yoo HJ, Park SH, Lim MC, Seo SS, Kang S, et al. Association between the location of transposed ovary and ovarian function in patients with uterine cervical cancer treated with (postoperative or primary) pelvic radiotherapy. Fertil Steril. 2012; 97:1387–93.18. Schildkraut JM, Cooper GS, Halabi S, Calingaert B, Hartge P, Whittemore AS. Age at natural menopause and the risk of epithelial ovarian cancer. Obstet Gynecol. 2001; 98:85–90.
Article19. Kim TH, Kim JY, Sohn DK, Kim YJ, Lee YS, Moon SH, et al. A prospective observational study with dose volume parameters predicting rectosigmoidoscopic findings and late rectosigmoid bleeding in patients with uterine cervical cancer treated by definitive radiotherapy. Radiat Oncol. 2013; 8:28.
Article20. Lee W, Nelson R, Akmal Y, Mailey B, McKenzie S, Artinyan A, et al. Racial and ethnic disparities in outcomes with radiation therapy for rectal adenocarcinoma. Int J Colorectal Dis. 2012; 27:737–49.
Article21. Rauh-Hain JA, Clemmer JT, Bradford LS, Clark RM, Growdon WB, Goodman A, et al. Racial disparities in cervical cancer survival over time. Cancer. 2013; 119:3644–52.
Article22. Shiraha H, Yamamoto K, Namba M. Human hepatocyte carcinogenesis (review). Int J Oncol. 2013; 42:1133–8.23. Oh MG, Han MA, Park J, Ryu SY, Park CY, Choi SW. Health behaviors of cancer survivors: the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV, 2007-09). Jpn J Clin Oncol. 2013; 43:981–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic Breast Cancer from Cervical Cancer
- A Case of Multiple Primary Cancer with Cervical Adenocarcinoma and both Ovarian Endometrioid Adenocarcinoma
- 8 Cases of Multiple Primary Gynecologic Cancer
- Concurrent Chemoradiotherapy in Cervical Cancer (A New Paradigm in Cervical Cancer Treatment)
- Metachronous Double Primary Cancer after Treatment of Breast Cancer