Cancer Res Treat.
2016 Apr;48(2):612-620. 10.4143/crt.2014.122.
Oncologic and Functional Outcomes after Partial Nephrectomy Versus Radical Nephrectomy in T1b Renal Cell Carcinoma: A Multicenter, Matched Case-Control Study in Korean Patients
- Affiliations
-
- 1Department of Urology, Korea University College of Medicine, Seoul, Korea. mdksh@korea.ac.kr
- 2Department of Urology, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Urology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 5Department of Urology, College of Medicine, Chungbuk Nation al University, Cheongju, Korea.
- 6Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
- KMID: 2454339
- DOI: http://doi.org/10.4143/crt.2014.122
Abstract
- PURPOSE
The study was to compare the oncologic and functional outcomes of partial nephrectomy (PN) and radical nephrectomy (RN) for pathologically proven T1b renal cell carcinoma using pair-matched groups.
MATERIALS AND METHODS
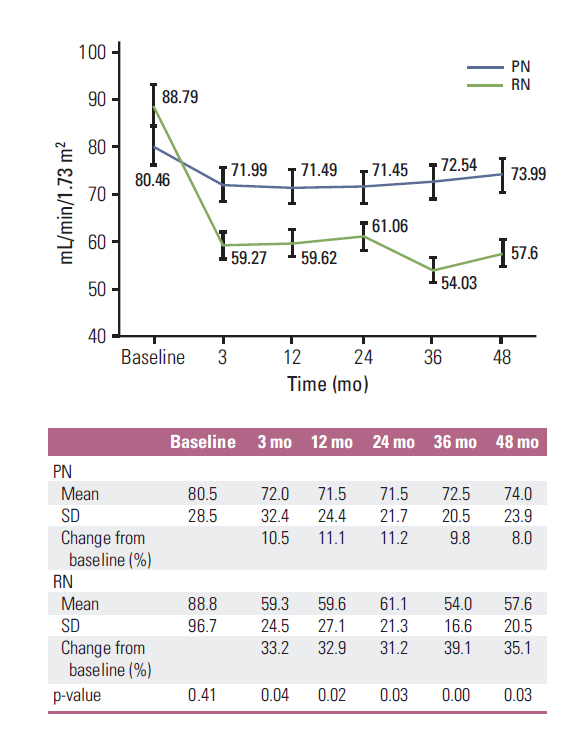
We reviewed our prospectively maintained database for RN and PN in T1b renal tumors surgically treated between 1999 and 2011 at five institutions in Korea. Of 611 patients treated with PN or RN for a solitary and NX/N0 M0 renal mass (4-7 cm), 577 (PN, 100; RN, 477) patients with pathologically confirmed pT1b remained for analysis. Study subjects were grouped by PN or RN, then matched by age, sex, comorbidities, body mass index, tumor size and depth, histologic type, and preoperative estimated glomerular filtration rate (eGFR) using propensities score. To evaluate oncologic outcomes, overall survival (OS), cancer-specific survival (CSS), and progression-free survival (PFS) rates were analyzed. The functional outcomes were evaluated by postoperative eGFR.
RESULTS
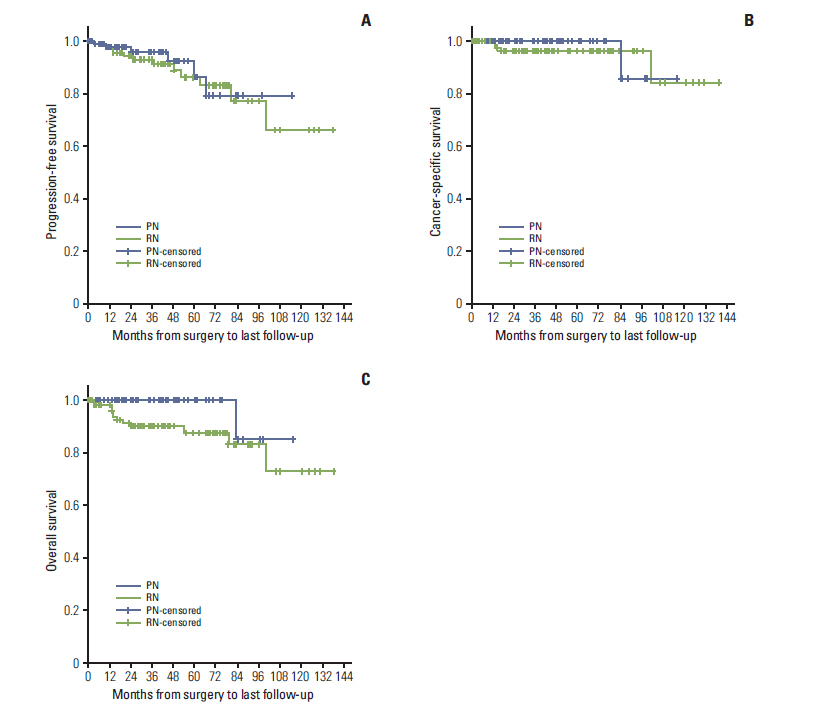
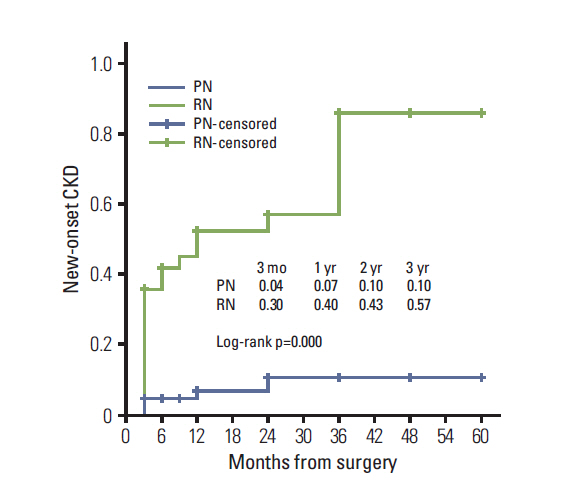
The median follow-up in the RN group was 48.1 and 42.6 months in the PN group. The estimated 10-year CSS rate (PN 85.7% vs. RN 84.4%, p=0.52) and 5- and estimated 10-year PFS rates (PN: 86.4% and 79.2% vs. RN: 86.0% and 66.1%, p=0.66) did not differ significantly between groups. The estimated 10-year OS rate was significantly higher in the PN group (85.7%) compared to the RN group (73.3%) (p=0.003). PN was less likely to induce new-onset chronic kidney disease (CKD) and end-stage CKD compared with RN.
CONCLUSION
Our study suggests that patients treated with PN demonstrate a superior OS rate and postoperative renal function with analogous CSS and PFS rates compared with pair-matched patients treated with RN.
MeSH Terms
Figure
Reference
-
References
1. Van Poppel H, Dilen K, Baert L. Incidental renal cell carcinoma and nephron sparing surgery. Curr Opin Urol. 2001; 11:281–6.
Article2. Lee CT, Katz J, Shi W, Thaler HT, Reuter VE, Russo P. Surgical management of renal tumors 4 cm or less in a contemporary cohort. J Urol. 2000; 163:730–6.
Article3. Clark PE, Schover LR, Uzzo RG, Hafez KS, Rybicki LA, Novick AC. Quality of life and psychological adaptation after surgical treatment for localized renal cell carcinoma: impact of the amount of remaining renal tissue. Urology. 2001; 57:252–6.
Article4. Patard JJ, Pantuck AJ, Crepel M, Lam JS, Bellec L, Albouy B, et al. Morbidity and clinical outcome of nephron-sparing surgery in relation to tumour size and indication. Eur Urol. 2007; 52:148–54.
Article5. Thompson RH, Siddiqui S, Lohse CM, Leibovich BC, Russo P, Blute ML. Partial versus radical nephrectomy for 4 to 7 cm renal cortical tumors. J Urol. 2009; 182:2601–6.
Article6. Campbell SC, Novick AC. Expanding the indications for elective partial nephrectomy: is this advisable? Eur Urol. 2006; 49:952–4.
Article7. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002; 39(2 Suppl 1):S1–266.8. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–13.9. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31–41.
Article10. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139:137–47.
Article11. Leibovich BC, Blute M, Cheville JC, Lohse CM, Weaver AL, Zincke H. Nephron sparing surgery for appropriately selected renal cell carcinoma between 4 and 7 cm results in outcome similar to radical nephrectomy. J Urol. 2004; 171:1066–70.
Article12. Badalato GM, Kates M, Wisnivesky JP, Choudhury AR, McKiernan JM. Survival after partial and radical nephrectomy for the treatment of stage T1bN0M0 renal cell carcinoma (RCC) in the USA: a propensity scoring approach. BJU Int. 2012; 109:1457–62.
Article13. Weight CJ, Lieser G, Larson BT, Gao T, Lane BR, Campbell SC, et al. Partial nephrectomy is associated with improved overall survival compared to radical nephrectomy in patients with unanticipated benign renal tumours. Eur Urol. 2010; 58:293–8.
Article14. Iizuka J, Kondo T, Hashimoto Y, Kobayashi H, Ikezawa E, Takagi T, et al. Similar functional outcomes after partial nephrectomy for clinical T1b and T1a renal cell carcinoma. Int J Urol. 2012; 19:980–6.
Article15. Kim SP, Murad MH, Thompson RH, Boorjian SA, Weight CJ, Han LC, et al. Comparative effectiveness for survival and renal function of partial and radical nephrectomy for localized renal tumors: a systematic review and meta-analysis. J Urol. 2012. Oct. 18. [Epub]. http://dx.doi.org/10.1016/j.juro.2012.10.026.
Article16. Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011; 59:543–52.
Article17. Kletsche BA, Qian J, Bostwick DG, Andrews PE, Zincke H. Prospective analysis of multifocality in renal cell carcinoma: influence of histological pattern, grade, number, size, volume and deoxyribonucleic acid ploidy. J Urol. 1995; 153(3 Pt 2):904–6.18. Kobayashi M, Hashimoto S, Tokue A. Nephron-sparing surgery is still controversial for patients with renal cell carcinoma and normal contralateral kidney: risks predictable by AgNOR counts in satellite lesions. Mol Urol. 2000; 4:21–9.19. Roos FC, Brenner W, Muller M, Schubert C, Jager WJ, Thuroff JW, et al. Oncologic long-term outcome of elective nephron-sparing surgery versus radical nephrectomy in patients with renal cell carcinoma stage pT1b or greater in a matched-pair cohort. Urology. 2011; 77:803–8.
Article20. Lane BR, Campbell SC, Gill IS. 10-year oncologic outcomes after laparoscopic and open partial nephrectomy. J Urol. 2013; 190:44–9.
Article21. Hafez KS, Fergany AF, Novick AC. Nephron sparing surgery for localized renal cell carcinoma: impact of tumor size on patient survival, tumor recurrence and TNM staging. J Urol. 1999; 162:1930–3.
Article22. Thompson RH, Leibovich BC, Lohse CM, Zincke H, Blute ML. Complications of contemporary open nephron sparing surgery: a single institution experience. J Urol. 2005; 174:855–8.
Article23. Gill IS, Matin SF, Desai MM, Kaouk JH, Steinberg A, Mascha E, et al. Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol. 2003; 170:64–8.
Article24. Papalia R, Simone G, Ferriero M, Guaglianone S, Costantini M, Giannarelli D, et al. Laparoscopic and robotic partial nephrectomy without renal ischaemia for tumours larger than 4 cm: perioperative and functional outcomes. World J Urol. 2012; 30:671–6.25. Yossepowitch O, Thompson RH, Leibovich BC, Eggener SE, Pettus JA, Kwon ED, et al. Positive surgical margins at partial nephrectomy: predictors and oncological outcomes. J Urol. 2008; 179:2158–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Treatment Outcomes of a Partial Nephrectomy in the Management of Renal Cell Carcinomas
- A Case of Renal Cell Carcinoma with Hyperglycemia Corrected after Radical Nephrectomy
- Comparison of Partial and Radical Nephrectomy for pT1b Renal Cell Carcinoma
- Laparoscopic versus Open Radical Nephrectomy in T2 Renal Cell Carcinoma: Long-Term Oncologic Outcomes
- Preserving Renal Function through Partial Nephrectomy Depends on Tumor Complexity in T1b Renal Tumors