J Korean Acad Prosthodont.
2019 Jul;57(3):271-279. 10.4047/jkap.2019.57.3.271.
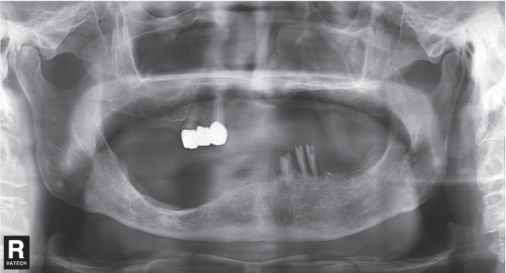
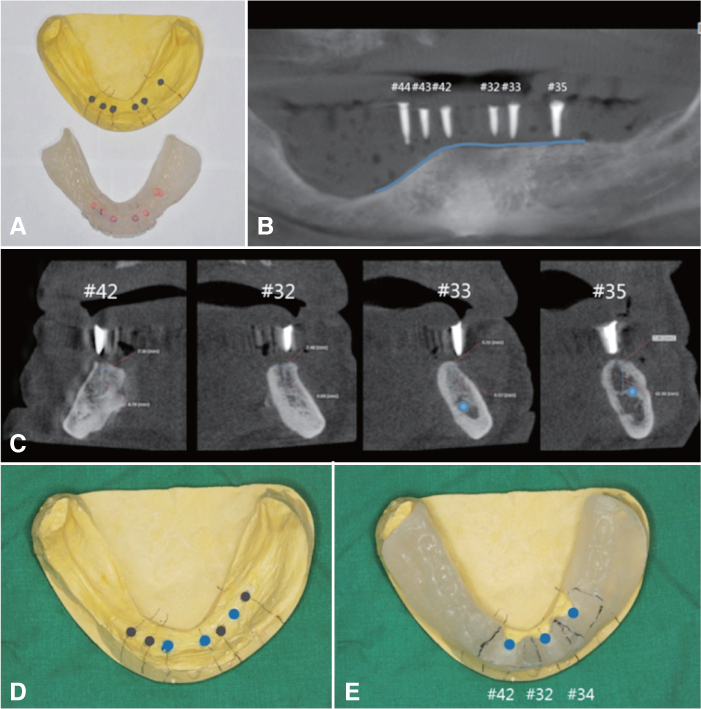
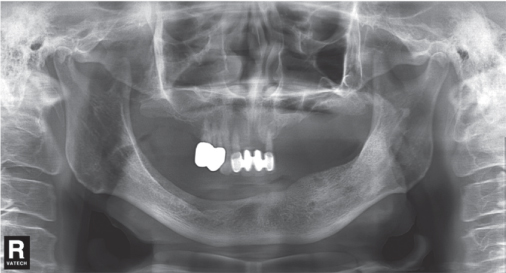
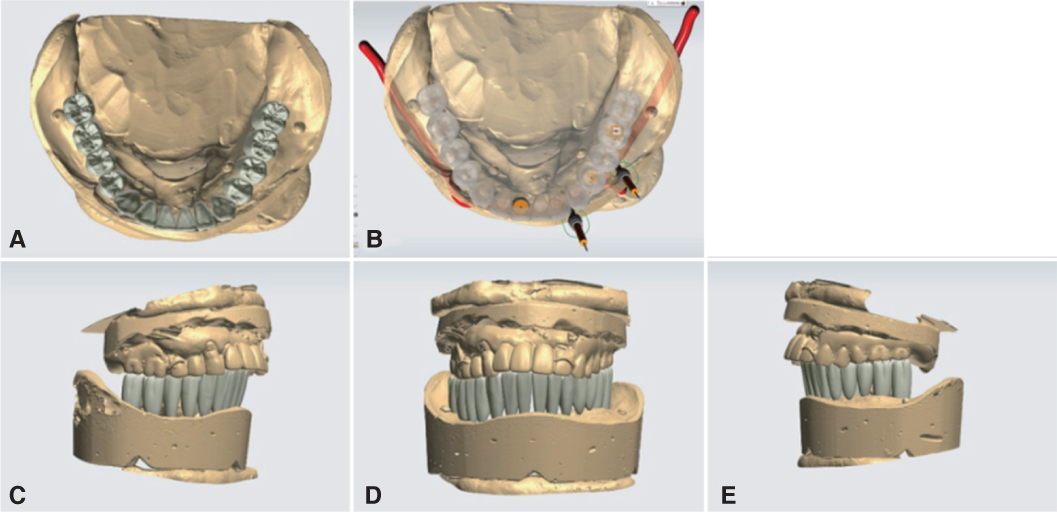
Implant overdenture of mandible with severe unilateral atrophy: Report of two cases
- Affiliations
-
- 1Dental Clinic Center, Pusan National University Hospital, Busan, Republic of Korea. soyeunkim179@gmail.com
- 2Department of Prosthodontics, School of Dentistry, Pusan National University, Yangsan, Republic of Korea.
- KMID: 2453782
- DOI: http://doi.org/10.4047/jkap.2019.57.3.271
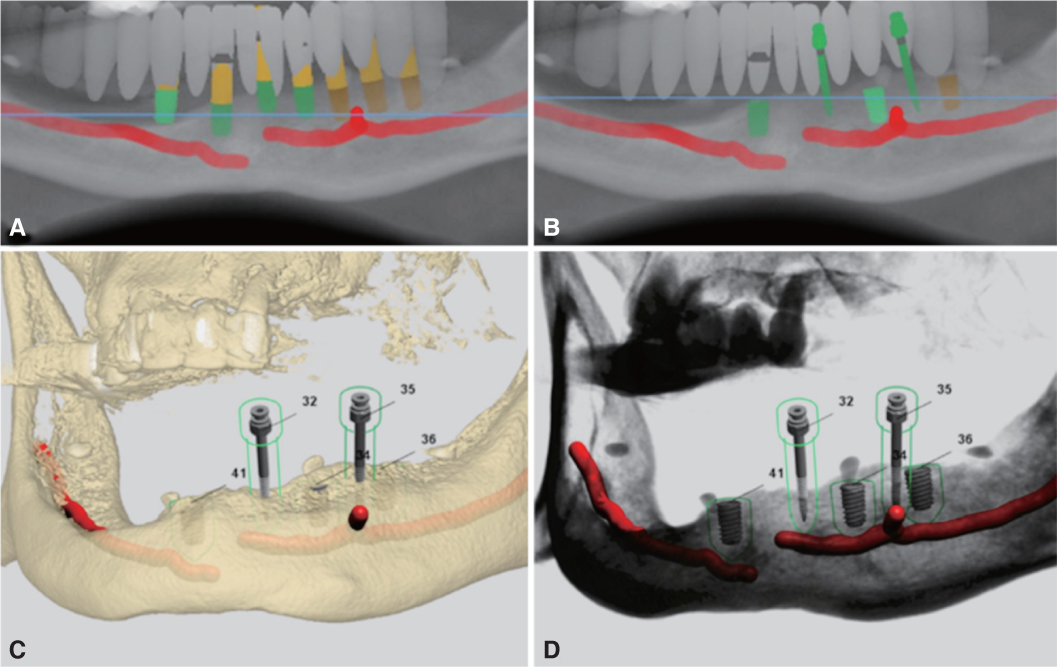
Abstract
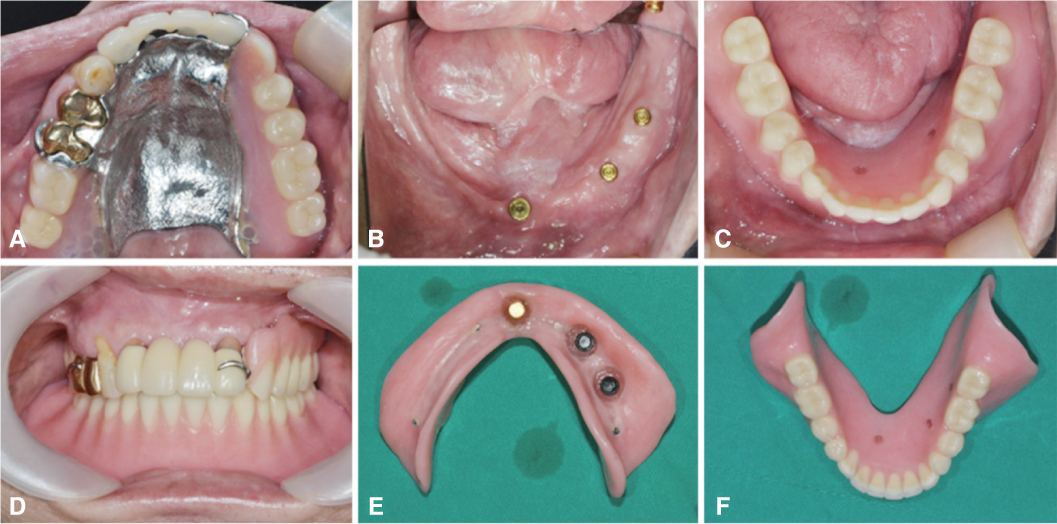
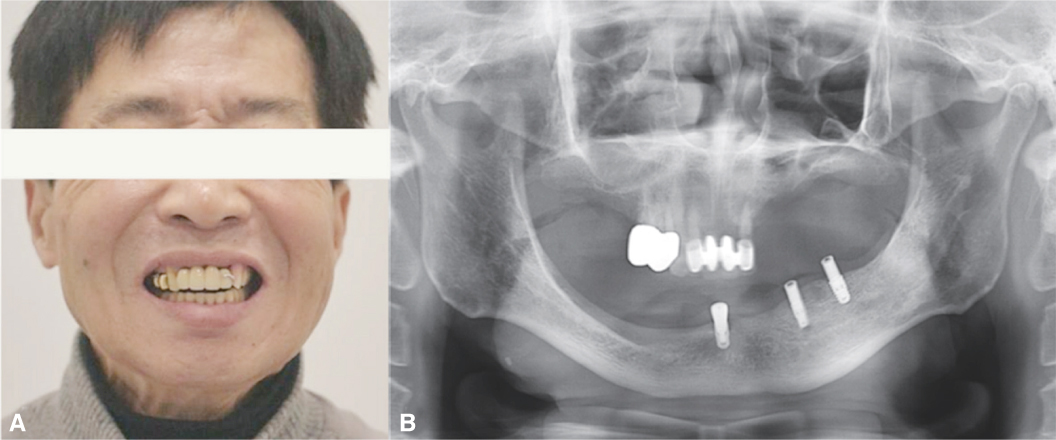
- There are several unfavorable conditions regarding alveolar bone condition that may compromise the denture patient's satisfaction. Chewing efficiency may not be satisfactory when alveolar bone is deficient, and the denture stability could hardly be achieved when alveolar bone shape is irregular. Implant overdenture can be useful to provide satisfactory denture experience compared to conventional denture. The attachment for implant overdenture can be classified into bar attachment and solitary attachment. When the positions of the implants are in the mandibular anterior region, bar attachment may be favorable to obtain a rigid support of the entire denture. When implants are distributed both on anterior and posterior region, a solitary attachment could be considered for ease of removal and maintenance. This report presents implant overdenture cases with the patients that had unilateral mandibular alveolar bone atrophy conditions. Different abutments were chosen based on the individual patient's mandibular alveolar bone condition and the treatments were successful in terms of patient satisfaction.
Keyword
MeSH Terms
Figure
Reference
-
1. van der Bilt A, Olthoff LW, van der Glas HW, van der Weelen K, Bosman F. A mathematical description of the comminution of food during mastication in man. Arch Oral Biol. 1987; 32:579–586.
Article2. Wismeijer D, Van Waas MA, Vermeeren JI, Mulder J, Kalk W. Patient satisfaction with implant-supported mandibular overdentures. A comparison of three treatment strategies with ITI-dental implants. Int J Oral Maxillofac Surg. 1997; 26:263–267.3. Naert I, Quirynen M, Theuniers G, van Steenberghe D. Prosthetic aspects of osseointegrated fixtures supporting overdentures. A 4-year report. J Prosthet Dent. 1991; 65:671–680.
Article4. Trakas T, Michalakis K, Kang K, Hirayama H. Attachment systems for implant retained overdentures: a literature review. Implant Dent. 2006; 15:24–34.
Article5. Gotfredsen K, Holm B. Implant-supported mandibular overdentures retained with ball or bar attachments: a randomized prospective 5-year study. Int J Prosthodont. 2000; 13:125–130.6. Abi Nader S, de Souza RF, Fortin D, De Koninck L, Fromentin O, Albuquerque RF Junior. Effect of simulated masticatory loading on the retention of stud attachments for implant overdentures. J Oral Rehabil. 2011; 38:157–164.
Article7. Burns DR. Mandibular implant overdenture treatment: consensus and controversy. J Prosthodont. 2000; 9:37–46.
Article8. Närhi TO, Geertman ME, Hevinga M, Abdo H, Kalk W. Changes in the edentulous maxilla in persons wearing implant-retained mandibular overdentures. J Prosthet Dent. 2000; 84:43–49.
Article9. Lee JY, Yoon JY, Oh NS. The use of surgical guide stent for implant placement. J Korean Acad Prosthodont. 2014; 52:366–375.
Article10. English CE. Bar patterns in implant prosthodontics. Implant Dent. 1994; 3:217–229.
Article11. Takeshita S, Kanazawa M, Minakuchi S. Stress analysis of mandibular two-implant overdenture with different attachment systems. Dent Mater J. 2011; 30:928–934.
Article12. Bergendal T, Engquist B. Implant-supported overdentures: a longitudinal prospective study. Int J Oral Maxillofac Implants. 1998; 13:253–262.13. Geckili O, Bilhan H, Bilgin T. Locator® attachments as an alternative to ball attachments in 2-implant retained mandibular overdentures. J Can Dent Assoc. 2007; 73:691–694.14. Min BK, Shin EJ, Vang MS, Yang HS, Park SW, Yun KD, Lim HP. Overdentures of the patient with Parkinson's disease: A case report. J Korean Acad Prosthodont. 2015; 53:352–358.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implant overdenture treatment using several solitary attachment systems on mandibular edentulous patients
- The Implant Retained Overdenture by Locator Attachments on the Edentulous Mandible: A Case Report
- The use of implant-assisted removable partial denture in the partially edentulous maxilla with a few unilateral remaining teeth and implant overdenture in the mandible: A case report
- Mandibular implant overdenture using milled bar attachment on implants with unfavorable fixture angulation: A case report
- Implant-supported milled bar overdenture with two implant surgical guides