Korean J Radiol.
2019 Aug;20(8):1285-1292. 10.3348/kjr.2019.0127.
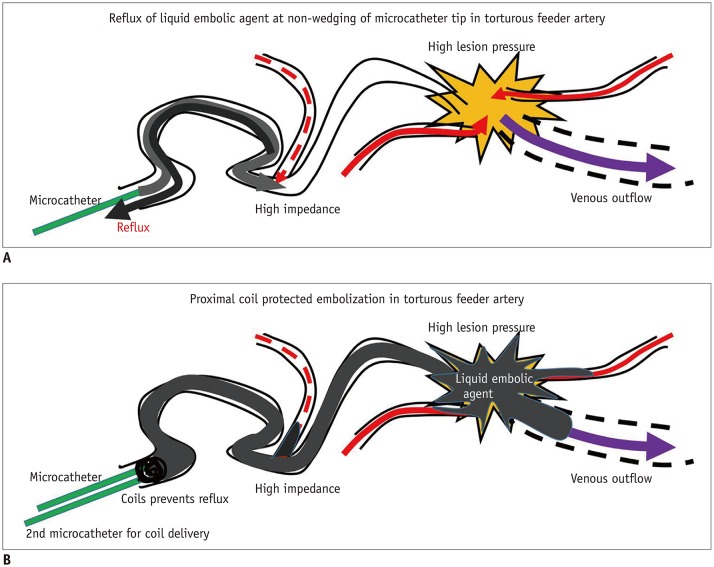
Coil-Protected Technique for Liquid Embolization in Neurovascular Malformations
- Affiliations
-
- 1Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- 3Division of Interventional Neuroradiology and Department of Radiology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. bmoon21@hanmail.net
- KMID: 2453078
- DOI: http://doi.org/10.3348/kjr.2019.0127
Abstract
OBJECTIVE
To evaluate the safety and efficacy of the coil-protected technique for liquid embolization in neurovascular malformations.
MATERIALS AND METHODS
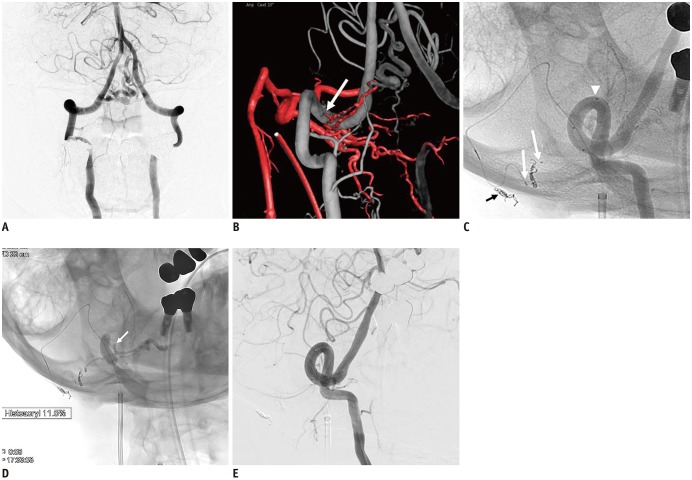
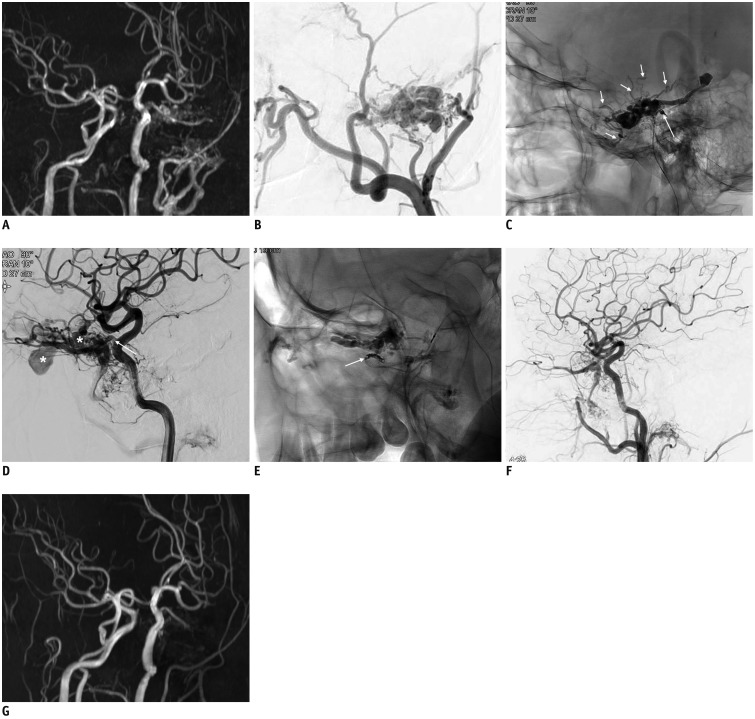
Twenty-two patients who underwent coil-protected liquid embolization for symptomatic cranial (n = 13) and spinal (n = 9) arteriovenous fistula (AVF) or arteriovenous malformations (AVMs) were identified. A total of 36 target feeder vessels were embolized with N-butyl cyanoacrylate and/or Onyx (Medtronic). This technique was used to promote delivery of a sufficient amount of liquid embolic agent into the target shunt or nidus in cases where tortuous feeding arteries preclude a microcatheter wedging techniqu and/or to prevent reflux of the liquid embolic agent in cases with a short safety margin. The procedure was considered technically successful if the target lesion was sufficiently filled with liquid embolic agent without unintentional reflux. Angiographic and clinical outcomes were retrospectively evaluated.
RESULTS
Technical success was achieved for all 36 target feeders. Post-embolization angiographies revealed complete occlusion in 16 patients and near-complete and partial occlusion in three patients each. There were no treatment-related complications. Of the six patients who showed near-complete or partial occlusion, five received additional treatments: two received stereotactic radiosurgery for cerebral AVM, two underwent surgical removal of cerebral AVM, and one underwent additional embolization by direct puncture for a mandibular AVM. Finally, all patients showed complete (n = 19) or near-complete (n = 3) occlusion of the target AVF or AVM on follow-up angiographies. The presenting neurological symptoms improved completely in 15 patients (68.2%) and partially in seven patients (31.8%).
CONCLUSION
The coil-protected technique is a safe and effective method for liquid embolization, especially in patients with various neurovascular shunts or malformations who could not be successfully treated with conventional techniques.
MeSH Terms
Figure
Cited by 3 articles
-
Embolization Tactics of Spinal Epidural Arteriovenous Fistulas
Abdulrahman Hamad Al-Abdulwahhab, Yunsun Song, Boseong Kwon, Dae Chul Suh
Neurointervention. 2021;16(3):252-259. doi: 10.5469/neuroint.2021.00220.In Vitro Head-to-Head Comparison of Flow Reduction between Fibered and Non-Fibered Pushable Coils
Jong-Tae Yoon, Boseong Kwon, Joon Ho Choi, Sun Moon Hwang, Mihyeon Kim, Sungbin Hwang, Yunsun Song, Deok Hee Lee
Neurointervention. 2024;19(1):31-38. doi: 10.5469/neuroint.2024.00031.Pediatric Cerebral Vascular Malformations : Current and Future Perspectives
Edward R. Smith
J Korean Neurosurg Soc. 2024;67(3):326-332. doi: 10.3340/jkns.2024.0011.
Reference
-
1. Kim DJ, Willinsky RA, Krings T, Agid R, TerBrugge K. Intracranial dural arteriovenous shunts: transarterial glue embolization--experience in 115 consecutive patients. Radiology. 2011; 258:554–561. PMID: 21177391.
Article2. Carlson AP, Taylor CL, Yonas H. Treatment of dural arteriovenous fistula using ethylene vinyl alcohol (onyx) arterial embolization as the primary modality: short-term results. J Neurosurg. 2007; 107:1120–1125. PMID: 18077948.
Article3. Van Dijk JM, TerBrugge KG, Willinsky RA, Farb RI, Wallace MC. Multidisciplinary management of spinal dural arteriovenous fistulas: clinical presentation and long-term follow-up in 49 patients. Stroke. 2002; 33:1578–1583. PMID: 12052994.4. Sherif C, Gruber A, Bavinzski G, Standhardt H, Widhalm G, Gibson D, et al. Long-term outcome of a multidisciplinary concept of spinal dural arteriovenous fistulae treatment. Neuroradiology. 2008; 50:67–74. PMID: 18026943.
Article5. Nelson PK, Russell SM, Woo HH, Alastra AJ, Vidovich DV. Use of a wedged microcatheter for curative transarterial embolization of complex intracranial dural arteriovenous fistulas: indications, endovascular technique, and outcome in 21 patients. J Neurosurg. 2003; 98:498–506. PMID: 12650420.
Article6. Debrun GM, Aletich V, Ausman JI, Charbel F, Dujovny M. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery. 1997; 40:112–120. discussion 120–121. PMID: 8971833.7. Kim JW, Kim BM, Park KY, Kim DJ, Kim DI. Onyx embolization for isolated type dural arteriovenous fistula using a dual-lumen balloon catheter. Neurosurgery. 2016; 78:627–636. PMID: 26488328.
Article8. Cohen JE, Moscovici S, Itshayek E. The advantages of balloon assistance in endovascular embolization of spinal dural arteriovenous fistulas. J Clin Neurosci. 2013; 20:141–143. PMID: 23146212.
Article9. Spiotta AM, Hughes G, Masaryk TJ, Hui FK. Balloon-augmented Onyx embolization of a dural arteriovenous fistula arising from the neuromeningeal trunk of the ascending pharyngeal artery: technical report. J Neurointerv Surg. 2011; 3:300–303. PMID: 21990848.
Article10. Rhim JK, Cho YD, Yoo DH, Kang HS, Cho WS, Kim JE, et al. Endovascular treatment of bilateral cavernous sinus dural arteriovenous fistula: therapeutic strategy and follow-up outcomes. Korean J Radiol. 2018; 19:334–341. PMID: 29520192.
Article11. Andreou A, Ioannidis I, Nasis N. Transarterial balloon-assisted glue embolization of high-flow arteriovenous fistulas. Neuroradiology. 2008; 50:267–272. PMID: 17960371.
Article12. Rangel-Castilla L, Barber SM, Klucznik R, Diaz O. Mid and long term outcomes of dural arteriovenous fistula endovascular management with Onyx. Experience of a single tertiary center. J Neurointerv Surg. 2014; 6:607–613. PMID: 24062253.
Article13. Zhao LB, Shim JH, Lee DG, Suh DC. Two microcatheter technique for embolization of arteriovenous fistula with liquid embolic agent. Neurointervention. 2014; 9:32–38. PMID: 24642961.
Article14. Suh DC, Cho SH, Park JE, Liu H, Jung SC. Induced-wedge technique to improve liquid embolic agent penetration into spinal dural arteriovenous fistula. World Neurosurg. 2016; 96:309–315. PMID: 27637163.
Article15. Takasawa C, Seiji K, Matsunaga K, Matsuhashi T, Ohta M, Shida S, et al. Properties of N-butyl cyanoacrylate-iodized oil mixtures for arterial embolization: in vitro and in vivo experiments. J Vasc Interv Radiol. 2012; 23:1215–1221.e1. PMID: 22920981.
Article16. Guillevin R, Vallee JN, Cormier E, Lo D, Dormont D, Chiras J. N-butyl 2-cyanoacrylate embolization of spinal dural arteriovenous fistulae: CT evaluation, technical features, and outcome prognosis in 26 cases. AJNR Am J Neuroradiol. 2005; 26:929–935. PMID: 15814948.17. Su IC, terBrugge KG, Willinsky RA, Krings T. Factors determining the success of endovascular treatments among patients with spinal dural arteriovenous fistulas. Neuroradiology. 2013; 55:1389–1395. PMID: 24113713.
Article18. Gounis MJ, Lieber BB, Wakhloo AK, Siekmann R, Hopkins LN. Effect of glacial acetic acid and ethiodized oil concentration on embolization with N-butyl 2-cyanoacrylate: an in vivo investigation. AJNR Am J Neuroradiol. 2002; 23:938–944. PMID: 12063221.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transcatheter Coil Embolization of Diffuse Pulmonary Arteriovenous Malformation
- Safety and Efficacy of Venous Coil-Embolization of Type IIa Pelvic Arteriovenous Malformations
- Manual Aspiration Technique to Retrieve a Prematurely Detached Coil during Cerebral Aneurysm Embolization
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)
- Coil-Protected Embolization Technique for a Branch-Incorporated Aneurysm