J Korean Fract Soc.
2019 Jul;32(3):121-127. 10.12671/jkfs.2019.32.3.121.
Computed Tomography Image Analysis of the Fusion Site of Subtalar Arthrodesis for Traumatic Arthritis after a Displaced Intraarticular Calcaneal Fracture
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. oselite@gilhospital.com
- KMID: 2453064
- DOI: http://doi.org/10.12671/jkfs.2019.32.3.121
Abstract
- PURPOSE
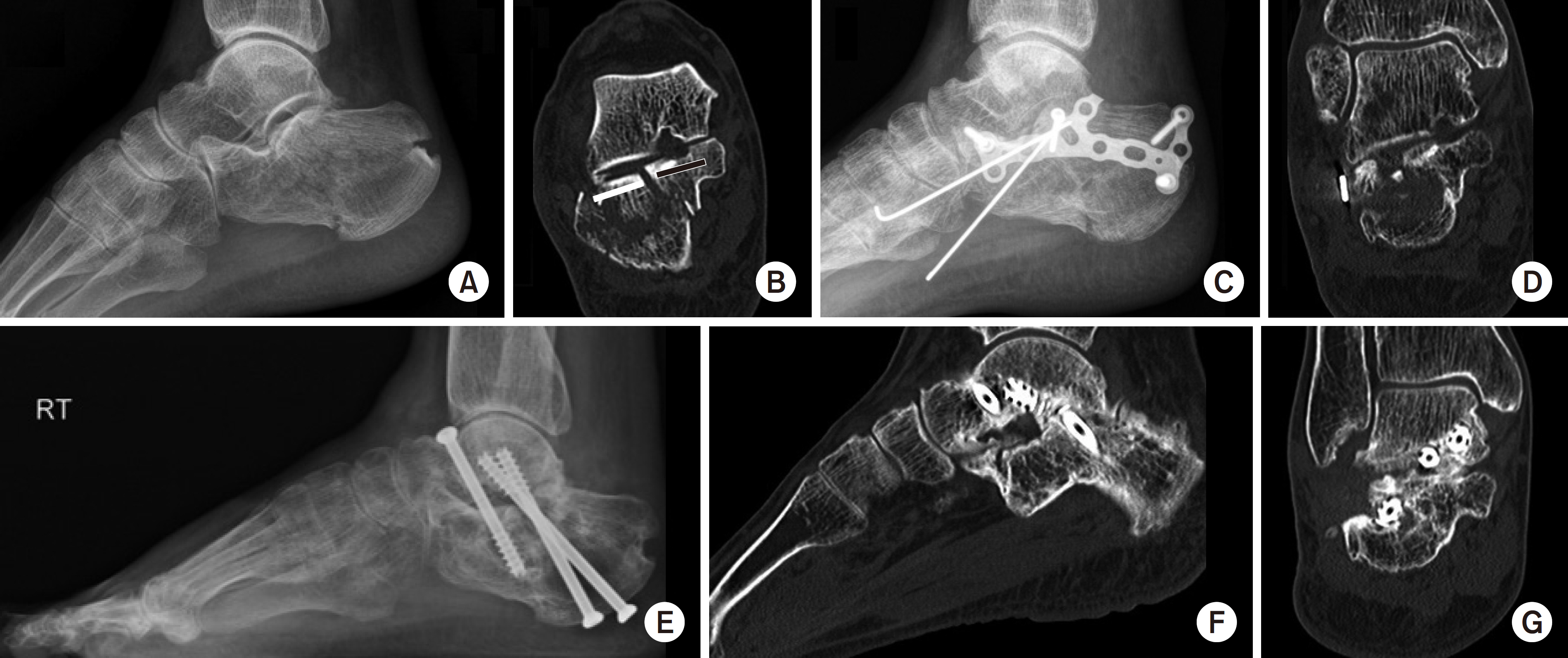
The study examined the fusion site and characteristics of the subtalar arthrodesis after intraarticular calcaneal fractures using computed tomography.
MATERIALS AND METHODS
The clinical results and computed tomographic analysis of the fusion site were reviewed in 18 patients who were followed-up for a minimum of six months after undergoing subtalar arthrodesis due to traumatic arthritis caused by an intra-articular calcaneal fracture from December 2012 to April 2017.
RESULTS
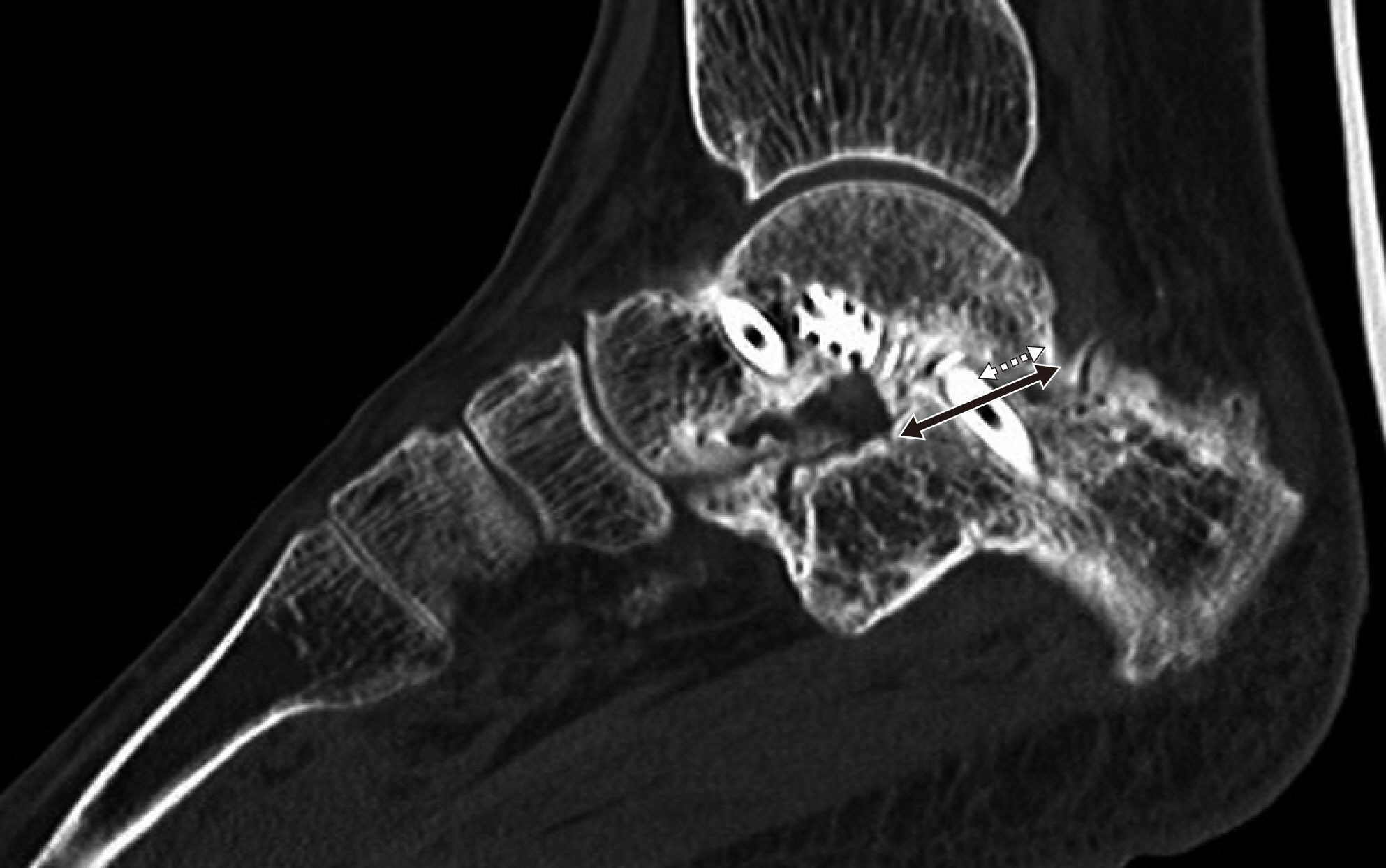
An evaluation of clinical results after subtalar arthrodesis revealed statistically significant improvements. In all cases, arthritis was found in the injured articular surface, which was displaced superolaterally from the initial primary fracture line of the calcaneus. Six months after arthrodesis, the subtalar fusion rate was 80.0% (16/20). Of these, 14 cases had a cannulated screw inserted in the uninjured site that is medial to the primary fracture line. Joint fusion was observed on the uninjured articular surface in 17 cases (85.0%).
CONCLUSION
Joint fusion was initially achieved at the uninjured posterior facet after subtalar arthrodesis due to traumatic arthritis caused by a displaced intra-articular calcaneal fracture. This suggests that meticulous surgical techniques and cannulated screw positioning at the uninjured site will promote joint fusion.
Keyword
Figure
Reference
-
References
1. Easley ME, Trnka HJ, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am. 82:613–624. 2000.
Article2. Ferrao PN, Saragas NP, Strydom A. Isolated subtalar arthrodesis. JBJS Essent Surg Tech. 6:e12. 2016.
Article3. Tuijthof GJ, Beimers L, Kerkhoffs GM, Dankelman J, Dijk CN. Overview of subtalar arthrodesis techniques: options, pitfalls and solutions. Foot Ankle Surg. 16:107–116. 2010.
Article4. Bèzes H, Massart P, Delvaux D, Fourquet JP, Tazi F. The operative treatment of intraarticular calcaneal fractures. Indications, technique, and results in 257 cases. Clin Orthop Relat Res. 290:55–59. 1993.5. Myerson MS. Primary subtalar arthrodesis for the treatment of comminuted fractures of the calcaneus. Orthop Clin North Am. 26:215–227. 1995.
Article6. Vulcano E, Ellington JK, Myerson MS. The spectrum of indications for subtalar joint arthrodesis. Foot Ankle Clin. 20:293–310. 2015.
Article7. Jones CP, Coughlin MJ, Shurnas PS. Prospective CT scan evaluation of hindfoot nonunions treated with revision surgery and low-intensity ultrasound stimulation. Foot Ankle Int. 27:229235. 2006.
Article8. Coughlin MJ, Grimes JS, Traughber PD, Jones CP. Comparison of radiographs and CT scans in the prospective evaluation of the fusion of hindfoot arthrodesis. Foot Ankle Int. 27:780–787. 2006.
Article9. Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: longterm (10–20 years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma. 28:551–563. 2014.10. Cohen MM, Vela ND, Levine JE, Barnoy EA. Validating a new computed tomography atlas for grading ankle osteoarthritis. J Foot Ankle Surg. 54:207–213. 2015.
Article11. Dorsey ML, Liu PT, Roberts CC, Kile TA. Correlation of arthrodesis stability with degree of joint fusion on MDCT. AJR Am J Roentgenol. 192:496–499. 2009.
Article12. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 15:349–353. 1994.
Article13. DiDomenico LA, Butto DN. Subtalar joint arthrodesis for elective and posttraumatic foot and ankle deformities. Clin Podiatr Med Surg. 34:327–338. 2017.
Article14. Davies MB, Rosenfeld PF, Stavrou P, Saxby TS. A comprehensive review of subtalar arthrodesis. Foot Ankle Int. 28:295–297. 2007.
Article15. Chahal J, Stephen DJ, Bulmer B, Daniels T, Kreder HJ. Factors associated with outcome after subtalar arthrodesis. J Orthop Trauma. 20:555–561. 2006.
Article16. Kitaoka HB, Patzer GL. Subtalar arthrodesis for posterior tibial tendon dysfunction and pes planus. Clin Orthop Relat Res. 345:187–194. 1997.
Article17. Vilá y Rico J, Jiménez Díaz V, Bravo Giménez B, Mellado Romero MÁ, Ojeda Thies C. Results of arthroscopic subtalar arthrodesis for adult-acquired flatfoot deformity vs posttraumatic arthritis. Foot Ankle Int. 37:198–204. 2016.
Article18. Scranton PE Jr. Results of arthrodesis of the tarsus: talocalcaneal, midtarsal, and subtalar joints. Foot Ankle. 12:156–164. 1991.
Article19. Ishikawa SN, Murphy GA, Richardson EG. The effect of cigarette smoking on hindfoot fusions. Foot Ankle Int. 23:996–998. 2002.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Talonavicular Subluxation Accompanied by Calcaneal Malunion: A Case Report
- The Comparison of Radiographic Parameters and Clinical Results after Operative Treatment of Displaced Intraarticular Calcaneal Fractures
- Calcaneal Malunion
- Operative treatment of displaced intraarticular fractures of the calcaneus
- The Classiflcation and Management of Intraarticular Calcaneal Fracture Based on Computed Tomography