Nationwide incidence and treatment pattern of benign prostatic hyperplasia in Korea
- Affiliations
-
- 1Department of Urology, Seoul National University Hospital, Seoul, Korea.
- 2Department of Urology, Dongguk University Ilsan Medical Center, Goyang, Korea.
- 3Department of Urology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea. volley@snu.ac.kr
- 4Department of Urology, Samsung Medical Center, Seoul, Korea.
- 5Department of Urology, Inje University Busan Paik Hospital, Busan, Korea.
- 6Department of Urology, Eulji General Hospital, Seoul, Korea.
- KMID: 2451401
- DOI: http://doi.org/10.4111/icu.2016.57.6.424
Abstract
- PURPOSE
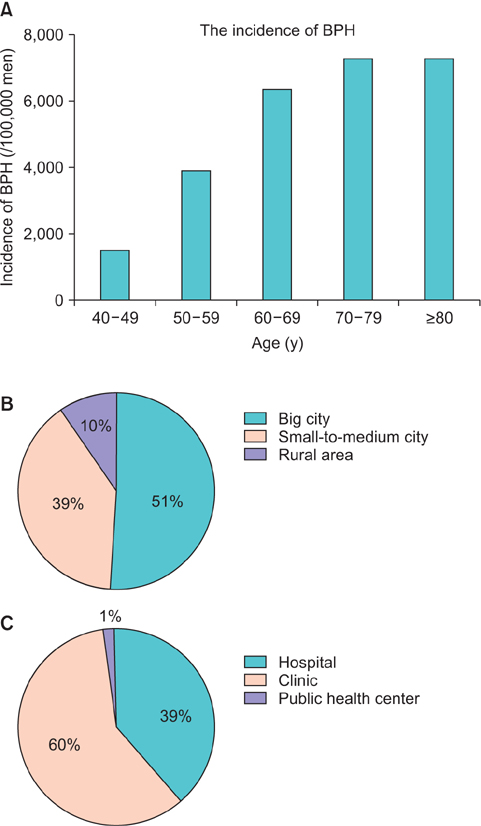
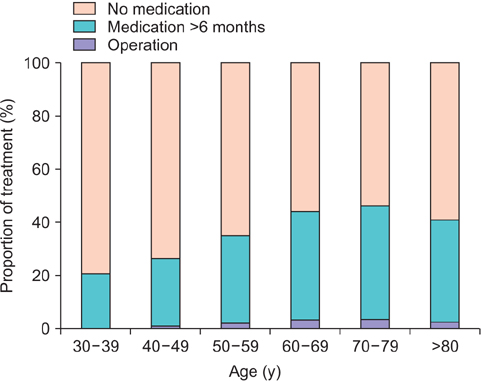
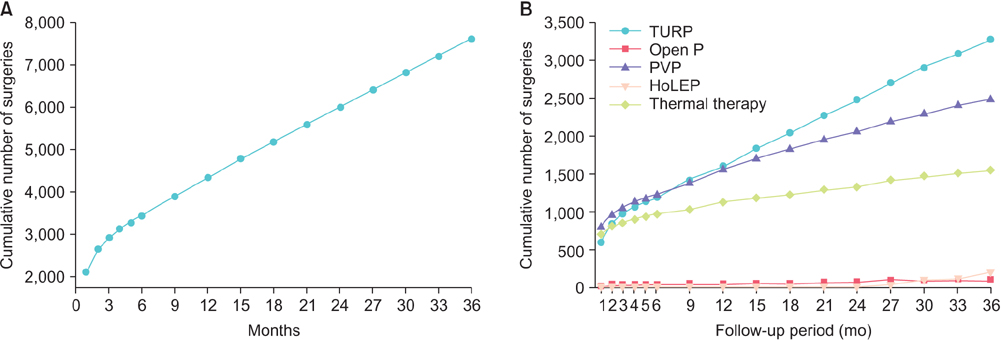
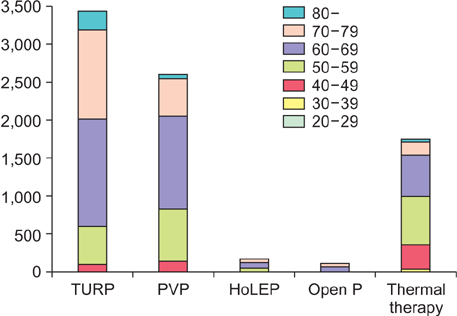
To investigate the incidence of benign prostatic hyperplasia (BPH) in Korea and treatment patterns for 3 years after the diagnosis in a nationwide database.
MATERIALS AND METHODS
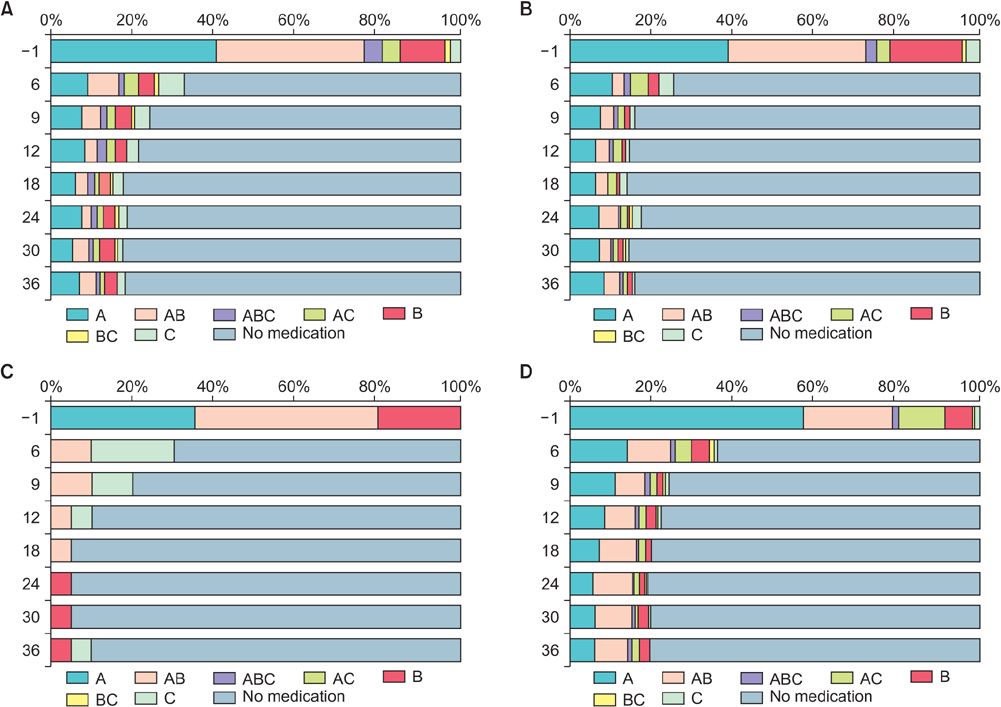
We created a cohort of patients diagnosed of BPH between 2007 and 2011 from the Health Insurance Review & Assessment database, a nationwide database of reimbursement. The diagnosis of BPH was defined as having the diagnosis of BPH (N40.0 in International Classification of Diseases, 10th revision) as a primary or secondary diagnosis ≥2 times in 2008. The incidence of BPH in 2008 was calculated. Treatment patterns were determined in 3 months interval and traced for 3 years. The incidence and timing of surgery were also determined. For patients taking medications preoperatively, medication-free rate was calculated.
RESULTS
The incidence of BPH was 2,105 per 100,000 men (mean age, 59.7±11.4 years), and increased with age. Surgery was performed for 7,955 patients (2.1%), half of the surgery being performed within the first 6 months. Transurethral resection of the prostate was the most commonly performed surgery. The proportion of treatment increased with age until the 7th decade of life. The patients taking medication for >1 year after the initial diagnosis was 21.4%. On average, 82% of patients became medication-free at postoperative 1 year. For patients taking preoperative anticholinergics, 1 year medication-free rate was 73.3%.
CONCLUSIONS
The incidence of BPH increased with age. Surgery was performed in 2.1% of patients. More than 4/5 patients discontinued medication after surgery, while patients taking preoperative anticholinergics were less likely to.
MeSH Terms
Figure
Cited by 3 articles
-
Corn silk extract improves benign prostatic hyperplasia in experimental rat model
So Ra Kim, Ae Wha Ha, Hyun Ji Choi, Sun Lim Kim, Hyeon Jung Kang, Myung Hwan Kim, Woo Kyoung Kim
Nutr Res Pract. 2017;11(5):373-380. doi: 10.4162/nrp.2017.11.5.373.Improvement of Persistent Detrusor Overactivity through Treatment with a Phytotherapeutic Agent (WSY-1075) after Relief of Bladder Outlet Obstruction
Su Jin Kim, Seung Hwan Jeon, Eun Bi Kwon, Hyun Cheol Jeong, Sae Woong Choi, Woong Jin Bae, Hyuk Jin Cho, U-Syn Ha, Sung Hoo Hong, Ji Youl Lee, Sung Yeoun Hwang, Sae Woong Kim
World J Mens Health. 2018;36(2):153-160. doi: 10.5534/wjmh.17010.Early Experiences of a Minimal Invasive Intra-Prostatic Implant, Prostatic Urethral Lift for Benign Prostatic Hyperplasia Treatment in Korea
Jonghyup Yang, Dongho Shin, Jaewoo Sung, Shinjay Cho, Sungmin Kang, Hyun Cheol Jeong, Sae Woong Choi, Woong Jin Bae, Sae Woong Kim
Urogenit Tract Infect. 2019;14(3):80-86. doi: 10.14777/uti.2019.14.3.80.
Reference
-
1. Bosch JL, Hop WC, Kirkels WJ, Schröder FH. Natural history of benign prostatic hyperplasia: appropriate case definition and estimation of its prevalence in the community. Urology. 1995; 46:3 Suppl A. 34–40.2. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479.3. Schroeck FR, Hollingsworth JM, Kaufman SR, Hollenbeck BK, Wei JT. Population based trends in the surgical treatment of benign prostatic hyperplasia. J Urol. 2012; 188:1837–1841.4. Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009; 104:352–360.5. Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014; 18:126–132.6. Verhamme KM, Dieleman JP, Bleumink GS, van der Lei J, Sturkenboom MC, Artibani W, et al. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care: the Triumph project. Eur Urol. 2002; 42:323–328.7. Logie J, Clifford GM, Farmer RD. Incidence, prevalence and management of lower urinary tract symptoms in men in the UK. BJU Int. 2005; 95:557–562.8. Platz EA, Joshu CE, Mondul AM, Peskoe SB, Willett WC, Giovannucci E. Incidence and progression of lower urinary tract symptoms in a large prospective cohort of United States men. J Urol. 2012; 188:496–501.9. Wallner LP, Slezak JM, Loo RK, Quinn VP, Van Den Eeden SK, Jacobsen SJ. Progression and treatment of incident lower urinary tract symptoms (LUTS) among men in the California Men's Health Study. BJU Int. 2015; 115:127–133.10. Martin S, Lange K, Haren MT, Taylor AW, Wittert G. Members of the Florey Adelaide Male Ageing Study. Risk factors for progression or improvement of lower urinary tract symptoms in a prospective cohort of men. J Urol. 2014; 191:130–137.11. Parsons JK, Wilt TJ, Wang PY, Barrett-Connor E, Bauer DC, Marshall LM, et al. Progression of lower urinary tract symptoms in older men: a community based study. J Urol. 2010; 183:1915–1920.12. Sarma AV, Jacobsen SJ, Girman CJ, Jacobson DJ, Roberts RO, Rhodes T, et al. Concomitant longitudinal changes in frequency of and bother from lower urinary tract symptoms in community dwelling men. J Urol. 2002; 168(4 Pt 1):1446–1452.13. Jacobsen SJ, Girman CJ, Guess HA, Rhodes T, Oesterling JE, Lieber MM. Natural history of prostatism: longitudinal changes in voiding symptoms in community dwelling men. J Urol. 1996; 155:595–600.14. Malmsten UG, Molander U, Peeker R, Irwin DE, Milsom I. Urinary incontinence, overactive bladder, and other lower urinary tract symptoms: a longitudinal population-based survey in men aged 45-103 years. Eur Urol. 2010; 58:149–156.15. Jacobsen SJ, Guess HA, Panser L, Girman CJ, Chute CG, Oesterling JE, et al. A population-based study of health care-seeking behavior for treatment of urinary symptoms. The Olmsted County Study of Urinary Symptoms and Health Status Among Men. Arch Fam Med. 1993; 2:729–735.16. Kaplan S, Garvin D, Gilhooly P, Koppel M, Labasky R, Milsten R, et al. Impact of baseline symptom severity on future risk of benign prostatic hyperplasia-related outcomes and longterm response to finasteride. The Pless Study Group. Urology. 2000; 56:610–616.17. Kang JY, Min GE, Son H, Kim HT, Lee HL. National-wide data on the treatment of BPH in Korea. Prostate Cancer Prostatic Dis. 2011; 14:243–247.18. Oh CY, Lee SH, Yoo SJ, Chung BH. Korean urologist's view of practice patterns in diagnosis and management of benign prostatic hyperplasia: a nationwide survey. Yonsei Med J. 2010; 51:248–252.19. Han HH, Ko WJ, Yoo TK, Oh TH, Kim DY, Kwon DD, et al. Factors associated with continuing medical therapy after transurethral resection of prostate. Urology. 2014; 84:675–680.20. Cho SY, Ro YK, Kim H, Son H. Preoperative urinary retention increased the risk of urinary retention after photoselective vaporization of the prostate. World J Mens Health. 2015; 33:182–187.21. Nam JK, Kim HW, Lee DH, Han JY, Lee JZ, Park SW. Risk factors for transient urinary incontinence after holmium laser enucleation of the prostate. World J Mens Health. 2015; 33:88–94.22. Nomura H, Seki N, Yamaguchi A, Naito S. Comparison of photoselective vaporization and standard transurethral resection of the prostate on urodynamics in patients with benign prostatic hyperplasia. Int J Urol. 2009; 16:657–662.23. de Nunzio C, Franco G, Rocchegiani A, Iori F, Leonardo C, Laurenti C. The evolution of detrusor overactivity after watchful waiting, medical therapy and surgery in patients with bladder outlet obstruction. J Urol. 2003; 169:535–539.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Prominently Large Glans penis as a Possible sign of Benign Prostatic Hyperplasia
- Histopathologic Study of non-Cancerous Lesion of the Prostate
- Clinical Observation on Tumor of the Prostate During Recent Ten Years
- The Effects of Abdominal Obesity on the Increased Prevalence Rate of Hypertension and Diabetes Mellitus in Benign Prostatic Hyperplasia Patients
- The influence of age and endocrine factors on the volume of benign prostatic hyperplasia